1 Introduction
Left ventricular hypertrophy [LVH] is defined on a normative basis; based on 2 standard deviations above the mean left ventricular mass [LVM] in the general population or based on the healthy population without obesity or hypertension. LVH confers an increased risk of cardiovascular and all-cause mortality in the general population.Citation1,Citation2
Obesity is reaching an epidemic scale worldwide. Obesity cardiomyopathy is defined as myocardial disease in obese individuals that cannot be explained by diabetes mellitus, hypertension, coronary artery disease or other etiologies, the presentation of this condition varies from asymptomatic left ventricular dysfunction to overt dilated cardiomyopathy. LV remodeling, increased LVM, LVH, and LV dilatation are among the documented cardiac changes in obese individuals.Citation3–Citation5
Known mechanisms to explain obesity cardiomyopathy include: increased preload and afterload in response to the high metabolic activity of adipose tissue, lipotoxicity in the form of fatty acids and triglycerides accumulation in parenchymal myocytes, hyperleptinemia, hypoadiponectinemia, and proinflammatory state.Citation5
Insulin resistance and associated hyperinsulinemia are key players in this condition through 4 mechanisms: insulin binding to myocardial IGF-1 receptors inducing LVH, activation of RAAS with angiotensin II exerting a proliferative hypertrophic action, activation of SNS leading to induction of cardiac fetal program, and finally endothelial dysfunction leading to failure to recruit to myocardial microcirculation in response to stress.Citation5
Blood pressure is considered the most important hemodynamic factor in the development and extent of left ventricular hypertrophy. Hypertensive left ventricular hypertrophy is associated with a threefold increase in cardiovascular morbidity and mortality. A powerful relation between LV mass and risk of cardiovascular disease in subjects with uncomplicated untreated essential hypertension, even below the upper normal limits of LV mass values. A significant relationship continues to exist between left ventricular mass and blood pressure in hypertensives even under treatment.Citation6,Citation7
A relation between LVH, LVMI, and parathormone [PTH] has been demonstrated in clinical and experimental studies. PTH was found to be associated with LVMI in several disease populations including primary hyperparathyroidism, end stage renal disease with secondary hyperparathyroidism, essential hypertension, and patients after aortic valve replacement. The relation between PTH and LVH was not only shown in disease states, but also for general population and elderly population.Citation8–Citation16
Possible mechanisms mediating ventricular hypertrophic effect of PTH can be divided into direct and indirect. Indirectly, high PTH has been shown to be associated with high BMI, systolic, diastolic, and central blood pressures, all are established risk factors for LVH.Citation8,Citation17
Direct mechanisms include: A positive chronotropic action, intact PTH 1–84 with 3 folds greater potency compared to PTH 1–39, stimulates adenylate cyclase leading to increased intracellular cyclic AMP which will activate cardiac L-type Ca2+ channels leading to increased L-type Ca2+ currents with increased intracellular Ca influx.Citation18
Increase sinoatrial node automaticity by increasing pace maker currents in SAN.Citation17 A positive inotropic action, through increasing both heart rate, and coronary blood flow.Citation17 A direct hypertrophic effect, via activation of protein kinase C and mediated by the functional domain [28–34] e.g. PTH 1–34 or PTH 28–48, through increasing collagen synthesis, increased cellular protein mass, re-expression of fetal proteins like creatine kinase BB.Citation18
The aim of this work was to study the role of PTH as a determinant of LV mass in hypertensive and/or obese patients.
2 Subjects
The study included 85 subjects of both male and female gender with age between 20 and 50 years. They were classified into 3 groups, group I: 30 obese hypertensive patients, group II: 30 obese non-hypertensive patients, attending the Internal Medicine and the Endocrinology Outpatient Clinics in Alexandria Main University Hospital, and group III: 25 healthy matched subjects that served as a control group.
Alexandria Faculty of Medicine Ethical committee approved the protocol of the study, and all study participants provided a written informed consent after being explained the nature and aim of the study.
Exclusion criteria: subjects with cardiac disease (coronary artery disease, rheumatic heart disease), diabetes mellitus (fasting plasma glucose ≥126 mg/dl or the use of antidiabetic drugs), left ventricular systolic dysfunction (EF < 40%), renal diseases, hepatic diseases, other endocrinal dysfunction, receiving anti-hypertensive drugs affecting renin angiotensin aldosterone system were excluded. e.g. angiotensin converting enzyme inhibitors, angiotensin receptor blockers and aldosterone receptor antagonists.
3 Methods
All patients were subjected to the following:
Complete physical examination was performed, including blood pressure measurement. Height, weight, and waist and hip circumferences were measured and BMI was calculated using the formula [weight in kg/height in m2].
Body fat mass percentage was calculated using the Deurenberg equation as follows: [body fat percentage = 1.2 × BMI + 0.23 × age − 10.8 × sex − 5.4], with age being in years and sex being designated as 1 for male and 0 for female patients.Citation19
3.1 Biochemical assays
venous sampling was carried out in the morning (8.00–10.00 a.m.) after an overnight fast of 8–10 h. The blood was drawn into an empty tube and then centrifuged for 10 min. The separated serum was used for the following assays: fasting plasma glucose level, lipid profile (triglycerides, cholesterol, HDL-C and LDL-C), renal function tests: serum creatinine and blood urea, total calcium, and phosphorus. Serum parathormone level was also measured by using radioimmunoassay method [ DIAsource hPTH-120 min-IRMA Kit, DIAsource ImmunoAssays S.A., Belgium].Citation20
3.2 Echocardiography
echocardiographic imaging was performed using HD11XE echo machine (Philips, USA). Cardiac dimensions and wall thicknesses were measured according to standard recommendations. Left ventricular mass was calculated by the following formula: LVM (Penn) = 1.04[(LVIDD + PWTD + IVSTD)3 − LVIDD3] − 13.6 g and was indexed to body surface area using the Dubois formula [BSA = 0.007184 × H0.725 × W0.425]. Left ventricular ejection fraction (LVEF) and left ventricular fractional shortening were estimated. Left ventricular diastolic function was assessed by measuring mitral flow E wave, A wave, E/A ratio, and mitral annulus tissue velocities.Citation21
3.3 Statistical analysis of the data
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0, Armonk, NY: IBM Corp. Comparison between different groups regarding categorical variables was tested using Chi-square test. When more than 20% of the cells have expected count less than 5, correction for chi-square was conducted using Fisher’s exact test or Monte Carlo correction. The distributions of quantitative variables were tested for normality. For normally distributed data, comparison between more than two populations were analyzed using F-test (ANOVA) and Post Hoc test (Scheffe). For abnormally distributed data, Kruskal Wallis test was used to compare between different groups and pair wise comparison was assessed using Mann-Whitney test. Significance of the obtained results was judged at the 5% level.
4 Results
All studied groups were matched for age and sex. A significant increase in BMI, waist circumference, hip circumference, and body fat percentage was detected among obese patients with or without hypertension in relation to normal individuals [P = <.001 for all 4 parameters in both groups I, and II versus control group] [].
Table 1 Anthropometric, Clinical, Biochemical, and Echocardiographic data of the three studied groups.
There were statistically significantly higher levels of serum PTH in group I and group II compared to group III [P = .005, .044 respectively]. Higher levels were found in group I compared to group II but it did not reach statistical significance [P = .287] [].
There was no statistically significant difference in serum calcium among the three studied groups [], there was no significant correlation between serum PTH and serum calcium.
LVMI was significantly higher in both group I and group II in comparison to healthy subjects [P = <.001, <.001 respectively]. It was also significantly elevated in group I versus group II [P = <.001] [].
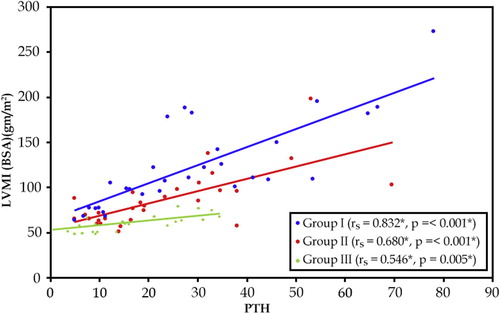
A significant positive correlation was found between serum PTH and left ventricular mass index in the three studied groups [P = <.001, <.001, .005 for groups I, II, and III respectively] [].
E/A ratio was significantly lower in group I in comparison to group III [P = .006]. There was no significant difference in MPAP (mean pulmonary arterial pressure) between the three groups. Left atrial diameter was significantly higher in obese subjects (group I and II) compared to healthy control [P = .003, <.001 respectively]. Left atrial volume was significantly higher in group I and group II compared to group III [P = .008, <.001 respectively] [].
5 Discussion
The aim of this work was to study the role of PTH as a determinant of LV mass in hypertensive and/or obese patients. Our results revealed significantly higher levels of serum PTH along with significantly higher LVMI in both group I and group II in comparison to healthy subjects. A significant positive correlation was found between serum PTH and left ventricular mass index in the three studied groups. This correlation is independent of Ca2+ and blood pressure as there was no statistically significant difference in serum calcium among the three studied groups, and there was no significant correlation between serum PTH and serum calcium or BP.
In 36 untreated patients with mild to moderate essential hypertension, there was a very significant correlation between LVMI and PTH (p = .00001) even after adjustment for mean 24-h systolic and diastolic BPs [p = .00001, p = .00003 respectively]. No significant correlations could be found among office systolic and diastolic BPs and PTH, however, there was a significant correlation between mean ambulatory diastolic BP and PTH (p = .020). Similar to our findings, there was neither correlation between parathyroid hormone and calcium nor between calcium and LV mass index.Citation11
Furthermore, there was no significant correlation between office systolic and diastolic BPs and LVMI, however, a significant correlation existed between mean ambulatory systolic BP, mean ambulatory diastolic BP, and LVMI (p = .026, p = .004 respectively).Citation11
In Another study including 62 essential hypertension patients and 20 normotensive healthy subjects, when classified as hypertensive versus control, PTH was significantly higher in the essential hypertension group (p < .001). when classified as those with LVH [LVMI > 125 g/m2 in men, and >120 g/m2 in women] versus those without, PTH was significantly higher in those with LVH (p < .005). There was a highly significant correlation between LVMI and PTH (p < .0025).Citation12
Recently, Helvacı et al. in a study that included Twenty-seven newly diagnosed hypertension patients, and 20 healthy individuals as control, they found that PTH level was significantly higher in the hypertensive group (p = .006). They also found A significant correlation between LVMI and PTH level in the hypertensive group (p = .001). There were no correlations between LVMI, and ambulatory BP, neither between PTH and BP.Citation13
It has been suggested that the higher levels of PTH in essential hypertension patients may be due to high levels of serum sodium in patients with essential hypertension, which may be related to excessive dietary salt intake or a defect in the excretion of sodium, which leads to excessive urinary calcium excretion, PTH release increases to compensate for this hypernatremia induced calciuresis.Citation13
To the best of our knowledge, our study is the first to show a significant association between PTH and LVMI in obese subjects without hypertension (group II). This finding may suggest obesity related secondary hyperparathyroidism as a novel mechanism to explain obesity cardiomyopathy.
High PTH [secondary hyperparathyroidism] is well documented in obese individuals with a prevalence ranging from 21% in obese individuals not requiring bariatric surgery to 53% in morbidly obese patients requiring bariatric surgery. Weight was the main determinant of increased PTH in morbid obesity and it decreases significantly with weight loss. Obesity related secondary hyperparathyroidism is independent from 25 OH D3, Ca+2, and renal function. A plausible mechanism may be a direct effect of adipokines, namely leptin, on PTH secretion as leptin has been shown to be a PTH secretagogue.Citation22–Citation24
In 2040 general population cohort of healthy subjects without established cardiovascular disease and not taking antihypertensive drugs, PTH was a significant predictor of LVMI in males and females, older and younger than 60 years of age, respectively [P < .01, <.05]. It was also observed that serum PTH values in the upper normal range were associated with 14% higher LVMI compared to values in the lower normal range, and the difference was significant in both sexes. Finally, serum PTH was significantly higher in men with LVH compared with the rest of the cohort (P < .01).Citation15
Limitations of this study include lack of ambulatory BP measurement that showed better correlation to PTH than office BP in one study. Another limitation was lack of vitamin D status determination; however, it has been shown that obesity related secondary hyperparathyroidism is independent from vitamin D status.Citation11,Citation23
In conclusion, PTH is strongly related to LVMI in obese patients with or without hypertension as well as normal individuals, independent of Ca2+ and blood pressure. To the best of our knowledge, our study is the first to suggest obesity related secondary hyperparathyroidism as a novel mechanism to explain obesity cardiomyopathy.
Conflict of interest
The authors declared that there is no conflict of interest.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
References
- T.H.MarwickT.C.GillebertG.AurigemmaRecommendations on the use of echocardiography in adult hypertension: a report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE)J Am Soc Echocardiog282015727754
- C.CuspidiR.FacchettiM.BombelliPrognostic value of left ventricular mass normalized to different body size indexes: findings from the PAMELA populationJ Hypertens33201510821089
- MarieGlobal, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013Lancet3842014766781
- O.J.RiderJ.M.FrancisM.K.AliDeterminants of left ventricular mass in obesity; a cardiovascular magnetic resonance studyJ Cardiovasc Magn Reson1120099
- C.WongT.H.MarwickObesity cardiomyopathy: pathogenesis and pathophysiologyNat Clin Pract Cardiovasc Med42007436443
- L.H.MissaultM.L.De BuyzereD.D.De BacquerRelationship between left ventricular mass and blood pressure in treated hypertensionJ Human Hypertens1620026166
- G.SchillaciP.VerdecchiaC.PorcellatiContinuous relation between left ventricular mass and cardiovascular risk in essential hypertensionHypertension352000580586
- P.AnderssonE.RydbergR.WillenheimerPrimary hyperparathyroidism and heart disease – a reviewEur Heart J25200417761787
- N.Al-HilaliN.HussainA.I.AtaiaHypertension and hyperparathyroidism are associated with left ventricular hypertrophy in patients on hemodialysisIndian J Nephrol192009153157
- R.B.RandonL.E.RohdeL.ComerlatoThe role of secondary hyperparathyroidism in left ventricular hypertrophy of patients under chronic hemodialysisBraz J Med Biol Res38200514091416
- F.R.BauwensD.A.DuprezM.L.De BuyzereInfluence of the arterial blood pressure and nonhemodynamic factors on left ventricular hypertrophy in moderate essential hypertensionAm J Cardiol681991925929
- Y.HuiY.HaoX.ChenRelationship between some humoral factors and left ventricular hypertrophy in essential hypertensionChin Med J Engl1091996885887
- A.HelvacıB.ÇopurM.AdaşCorrelation between left ventricular mass index and calcium metabolism in patients with essential hypertensionBalkan Med J3020138589
- M.-H.LaflammeH.MahjoubA.MahmutParathyroid hormone is associated with the LV mass after aortic valve replacementHeart100201418591864
- F.N.SalehH.SchirmerJ.SundsfjordParathyroid hormone and left ventricular hypertrophyEur Heart J24200320542060
- W.T.ChangC.H.WuL.W.HsuSerum vitamin D, intact parathyroid hormone, and Fetuin A concentrations were associated with geriatric sarcopenia and cardiac hypertrophySci Rep720174099641003
- L.A.FitzpatrickJ.P.BilezikianS.J.SilverbergParathyroid hormone and the cardiovascular systemCurr Osteoporos Rep620087783
- K.D.SchluterH.M.PiperCardiovascular actions of parathyroid hormone and parathyroid hormone-related peptideCardiovasc Res3719983441
- P.DeurenbergJ.A.WeststrateJ.C.SeidellBody mass index as a measure of body fatness: age-and sex-specific prediction formulasBrit J Nutr651991105114
- R.BouillonW.CoopmansD.DegrooteD.RadouxP.EliardImmunoradiometric assay of parathyrin with polyclonal and monoclonal region-specific antibodiesClin Chem361990271276
- M.FoppaB.B.DuncanL.E.RohdeEchocardiography-based left ventricular mass estimation. How should we define hypertrophy?Cardiovasc Ultras3200517
- R.S.VasconcelosM.ViégasT.F.MarquesFactors associated with secondary hyperparathyroidism in premenopausal women undergoing Roux-en-Y gastric bypass for the treatment of obesityArq Bras Endocrinol Metabol542010233238
- E.GrethenR.McClintockC.E.GuptaVitamin D and hyperparathyroidism in obesityJ Clin Endocrinol Metab96201113201326
- T.AndersenP.McNairL.HyldstrupSecondary hyperparathyroidism of morbid obesity regresses during weight reductionMetabolism371988425428