Abstract
Objectives
The study aimed to evaluate the dose delivered to the heart during radiotherapy of left-sided and right-sided breast cancer (BC) patients, correlate the dose and laterality of radiotherapy to the possible cardiac damage and evaluate whether Left-ventricular Ejection Fraction (LVEF), Troponin-I (TnI), Creatinine Kinase (CK), Creatine Kinase-MB Relative Index (CK-MBRI) or Lactic Dehydrogenase (LDH) could be used to detect the possible onset of radiotherapy-related cardiotoxicity.
Subjects and methods
80 females were assigned as; 30 left-sided BC patients, 30 right-sided BC patients and 20 healthy females. Patients were treated by radical mastectomy followed by FAC-based chemotherapy and radiotherapy. CT-based 3D-planning was used to generate cardiac dose-volume histograms to assess mean dose received by the heart.
Echocardiography was done to all patients before and 1 year after completing radiotherapy. In serum, TnI and CK-MB concentration and CK and LDH activities were determined before and 1 year after radiotherapy.
Results
In left-sided patients, mean dose delivered to the heart was significantly higher in left-sided patients with significant association with total radiotherapy dose in left- but not right-sided patients. LVEF before and after radiotherapy were statistically different only in left-sided patients. LVEF one year after radiotherapy dropped 20% or more (ΔLVEF) in 6 patients, all were left-sided.
Using cut-off values 0.08 ng/mL for TnI and 1.4 for CK-MBRI; 11 left-sided patients had abnormal TnI and CK-MBRI vs 5 right-sided patients, the 6 patients identified with ΔLVEF ≥ 20 were all among them.
Conclusion
the mean dose delivered to the heart is significantly higher in left-sided patients, and it was correlated to the total radiotherapy dose. One year after radiotherapy, ΔLVEF is possibly good marker of cardiotoxicity onset, however, the persistent elevation of both TnI and CK-MBRI could identify both patients with cardiotoxicity and patients that are thought to be in subclinical phase of cardiac damage.
1 Introduction
Breast cancer (BC) is the utmost recurring cancer type and the 2nd principal cause of cancer death in women, surpassed only by lung cancer.Citation1 Higher incidence rates are reported in more developed countries, but relatively higher mortality is found in developing countries because of the deficiency in early detection and access to treatment facilities.Citation2 Breast cancer represented 33.5% of all freshly diagnosed cancers in Egyptian women during the year 2014, with an age-standardized ratio of incidence of 49.5 per 100,000.Citation3
The part played by radiotherapy is well acknowledged in every stage of BC treatment. The most common schedules for irradiation are 50 Gy in 25 fractions or 42 Gy in 16 fractions delivered to the whole breast or chest wall, executed five days per week for five weeks.Citation4,Citation5 Adjuvant radiotherapy for BC was able to diminish mortality in many BC categories. In irradiated women, there was a significant increase in incidence of non-breast-cancer mortality, at least with some older radiotherapy regimens. This increase was slight during the first 5 years, but continued after year 15. The excess mortality was mainly from heart disease with a rate ratio of 1.27, which reduces the profitable effect of radiotherapy on overall survival.Citation6
Left ventricular ejection fraction (LVEF) estimated during echocardiography is a crucial marker of myocardial function before and after therapy. The main limiting factor for using echocardiography for diagnosis is its relatively low reproducibility because of elevated intra- and inter-observer inconsistency.Citation7 Along with several serum cardiac makers as Troponin I (TnI), Creatine Kinase (CK), Creatine Kinase-MB Relative Index (CK-MBRI) and Lactic Dehydrogenase (LDH). Although cardiac markers could confer acceptable sensitivity, they mostly lack specificity. However, none of these had been evaluated as a possible tool to evaluate patients undergoing adjuvant therapy who might be at higher risk of therapy-induced cardiac dysfunction or cardiotoxicity.Citation8
The study aimed to evaluate the dose delivered to the heart during radiotherapy of left-sided and right-sided BC patients, correlate the dose and laterality of radiotherapy to the possible cardiac damage and evaluate whether LVEF, TnI, CK, CK-MBRI or LDH could be used to detect the possible onset of radiation-induced cardiotoxicity.
2 Patients and methods
The study included 80 females in three groups; 30 left-sided BC patients, 30 right-sided BC patients and 20 normal healthy females of matched age. A local ethics committee approved the study and each subject signed an informed consent before being enrolled. Exclusion criteria included patients with ischemic or valvulary heart disease, baseline LVEF < 50%, hypertension and cardiac tumor. Patients were treated by modified radical mastectomy followed by FAC-based chemotherapy, radiotherapy and hormone therapy according to their clinical condition. Radiotherapy included isocentrically irradiating the chest wall by two tangential beams with selective multi-leaf blocking to protect organs that might be at risk, the regimen of radiation delivery used were conventional 50 Gy/25-fractions or hypo-fractionation 42 Gy/16 fractions. Internal mammary lymph nodes (IMLN), if indicated, were included in the tangential beams. The two arms (left- and right BC patients) were kept balanced, where each arm contained 30 patients; 11 received 50 Gy/25 fractions and 9 received 42 Gy/16 fractions, with 8 receiving IMLN radiotherapy. Patients were followed up for 12 months after completing radiotherapy.
Radiotherapy regimen used for each patient was reconstructed on CT-based 3D planning system. The heart and coronary arteries were contoured, including the right atrium and excluding the pulmonary trunk, ascending aorta and superior vena cava, with the caudal myocardial border being the lower most heart contour. The left main coronary artery was included with the contour of the left anterior descending coronary artery. For every patient, cardiac dose volume histograms were engendered to estimate the mean dose received by the heart for all patients.
Echocardiography was done for all patients twice; before and 12 months after radiotherapy to assess LVEF (2D Simpson's method) before and after therapy. From each breast cancer patient, two blood samples were obtained, before and 12 months after completing radiotherapy. One blood sample was drawn from each control subject to set reference normal range of the measured cardiac markers. After sampling, sera from all samples were collected and stored at -70 °C till time of assay.
TnI in serum was assayed by the Calbio tech cardiac troponin I ELISA kit (Calbiotech Inc., Spring Valley, CA). The TnI ELISA test is a solid phase ELISA system that utilizes four monoclonal antibodies that recognize distinct antigenic determinants on TnI. CK activity in serum was determined colorimetrically by the Abcam ab 155,901 creatine kinase activity assay kit (Abcam, UK). CK enzyme catalyzes a reversible reaction between creatine and ATP to form phosphocreatine and ADP, which react with CK Enzyme Mix to form an intermediate. Thae intermediate reduces a colorless agent forming a colored product with 450 nm absorbance. Also LDH activity was measured colorimetrically by the Abcam ab 155,901 lactate dehydrogenase activity assay kit (Abcam, UK). LDH carries out the catalysis of the reversible reaction of lactate and NAD+ to form pyruvate and NADH. Then NADH interacts with a probe to produce a colored product with a strong 450 nm absorbance. CK-MB was assayed by CKMB Human ELISA Kit (Abcam, UK). Abcam's CKMB Human ELISA Kit is an in vitro assay for the quantitative measurement of human CKMB in serum using two anti-CK-MB antibodies.
Data were statistically analyzed by SPSS (Statistical Package for the Social Sciences) software package, version 19.0 (SPSS Inc., Chicago, IL, USA). Comparisons of means were made by Chi square test or student's paired t-test. Two-tailed p values of <.05 were considered significant. Spearman correlation analysis was used to assess relationships between parameters. Receiver Operating Characteristic (ROC) curves were drawn for all parameters and a cut-off level was selected for each to evaluate patients in terms of normal or abnormal levels. These cut-offs were 0.08 ng/mL for TnI, 109 U/L for CK, 1.4 for CK-MBRI and 287 U/L for LDH.
3 Results
The study included 80 females divided into three groups; two patients' groups, included 30 females with right-sided BC and 30 females with left-sided BC and 20 normal healthy females matching patients groups in age as a control group.
represents the clinical characterization of the patients' groups involved in the study. As shown, the patients' age ranged from 28 to 67 years with a median of 47 y. Premenopausal women comprised 73.3% of right-sided and 63.3% of left-sided BC patients. The major bulk of patients had a single tumor, with no significant difference found between right and left sided BC patients conforming to tumor multiplicity (p = .668). Although left-sided BC patients had a higher prevalence of grade II tumors (93.3%) than right-sided BC patients (76.7%), the difference was not statistically significant (p = .145).
Table 1 Clinical characterization of patients.
According to TNM staging, no significant difference was found between right- and left-sided patients (p = 1.000). 66.7% of right-sided BC patients and 70% of left-sided BC patients were positive for vascular invasion, however, no significant difference existed between the two groups (p = .781).
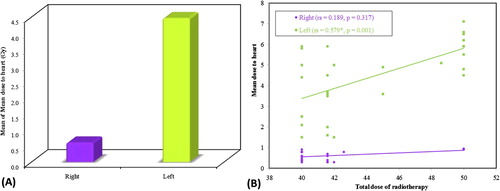
As shown in A, the mean dose delivered to the heart in left-sided BC patients was statistically significantly higher than that in right-sided BC patients (z = 6.668, p < .001). The radiation dose delivered to the heart ranged from 0.3 to 0.95 Gy in right-sided BC patients with a mean of 0.60 Gy and from 1.5 to 7.1 Gy in left-sided BC patients with a mean of 4.46 Gy. There was a highly significant correlation between the total dose of radiotherapy and mean dose delivered to the heart in left-sided (rs = 0.579, p = .001) but not in right-sided BC patients (rs = 0.189, p = .317); B.
Fig. 1 The mean dose delivered to the heart in right- and left-sided BC patients (A) and the correlation between total radiotherapy dose and mean dose delivered to heart in each group (B). rs: Spearman coefficient, *: Statistically significant at p ≤ .05.
represents LVEF in right- and left-sided BC patients comparing baseline LVEF measured before radiotherapy and that measured one year after completion of radiotherapy. Mean baseline LVEF was 68.4% in right-sided BC patients and 69.37% in left-sided BC patients, while mean LVEF after radiotherapy was 66.57% in right-sided BC patients and 64.5% in left-sided BC patients. The difference between right and left-sided BC patients was not statistically significant according to LVEF before or after radiotherapy (p = .645 and .210; respectively). In left-sided BC patients, LVEF before and after radiotherapy were statistically different (p = .021), however, that difference was not significant in right-sided patients (p = .194). LVEF measured one year after radiotherapy dropped 20% or more from baseline (ΔLVEF ≥ 20) in only 6 patients, all them were left-sided, that resulted in a statistically significant difference between right and left-sided BC patients regarding LVEF dropping 20% or more from baseline (p = .024). Also the mean dose delivered to those 6 patients (6.1 Gy) was significantly higher than the remaining 24 left-sided patients (3.9 Gy).
Table 2 LVEF presented as M ± SD in right- versus left-sided BC patients before and after radiotherapy (RT) and the fraction of patients with LVEF drop ≥20%.
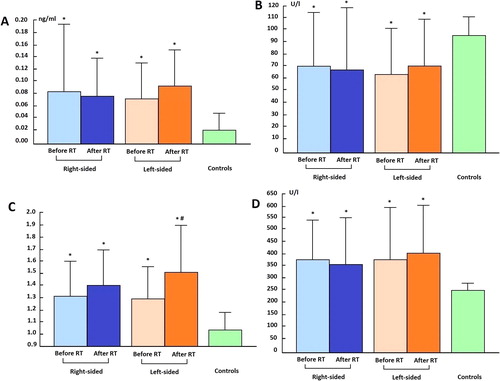
represents the mean values of TnI, CK, CK-MBRI and LDH in right- and left-sided BC patients and in controls. TnI levels presented as mean ± SD were 0.083 ± 0.11 and 0.078 ± 0.06 ng/mL before and after RT in right-sided patients and 0.073 ± 0.06 and 0.091 ± 0.055 ng/mL before and after RT in left-sided patients. All of them were significantly different from the control level (0.02 ± 0.03 ng/mL). CK values were 69.7 ± 43.5 and 68.1 ± 51.2 U/L before and after RT in right-sided patients and 63.0 ± 38.2 and 70.0 ± 39.4 U/L before and after RT in left-sided patients. All of them were significantly different from the control level (93.6 ± 17.6 U/L). CK-MBRI values were 1.32 ± 0.28 and 1.40 ± 0.31 before and after RT in right-sided patients and 1.30 ± 0.25 and 1.51 ± 0.39 before and after RT in left-sided patients. All of them were significantly different from the control level (1.03 ± 0.17). LDH levels were 370 ± 172 and 353 ± 198 U/L before and after RT in right-sided patients and 371 ± 228 and 402 ± 201 U/L before and after RT in left-sided patients. All these means were significantly different from the control level (247 ± 34 U/L). None of the tested biochemical parameters showed any significant difference between right- and left-sided patients either before or after RT. Only CK-MBRI was significantly higher after radiotherapy than before in left-sided BC patients (p = .37), and not in right-sided BC patients.
Fig. 2 mean levels of TnI (A), CK (B), CKMB-RI (C) and LDH (D) in right and left-sided BC patients and in controls before and after radiotherapy (RT). * : Significantly different at p ≤ .05 when compared to controls. # : Significantly different at p ≤ .05 when comparing before and after radiotherapy.
ROC curves for all parameters were used to draw cut-off values to evaluate patients in terms of normal or abnormal levels, presented in . Yet, there was no significant difference between before and after RT either on right- or left-sided BC patients in any of the parameters tested, except in CK-MBRI. As for CK-MBRI a significant difference was noted between before and after radiotherapy in left-sided but not in right-sided BC patients. In left sided-BC patients after radiotherapy, 11 patients had abnormal TnI and CK-MBRI vs 5 in the right-sided patients. The 6 patients identified with ΔLVEF ≥ 20 were all included in those 11 patients.
Table 3 Number and percent of patients above and below cut-offs for TnI, CK and LDH.
ΔLVEF, TnI, CK, CK-MBRI and LDH were not found to be correlated with any of the clinicopathological parameters of BC in either right- or left-sided patients; including tumor multiplicity, tumor size, tumor grade, lymph node involvement or vascular invasion. Three significant correlations were found in left sided BC patients between mean dose delivered to the heart and each of ΔLVEF (r = −0.422, p = .020), TnI levels (r = 0.410, p = .031) and CK-MBRI (r = 0.392, p = .030), however these correlations were found missing in right-sided patients (r = −0.343, p = .064; r = 0.241, p = .175 and r = 0.185, p = .445; respectively), .
Table 4 Correlation between the mean doses of radiation delivered to the heart in right and left-sided BC patients and ΔLVEF, TnI and CK-MBRI.
4 Discussion
Radiotherapy is an important treatment strategy after breast conservative surgery or after mastectomy in BC patients. For long, the irradiation of the heart that occurs casually during radiotherapy was not of concern, as the heart has traditionally been considered a radio-resistant organ that would be unaffected by doses below 30 Gy. The severity of the problem of radiotherapy-induced cardiac disease did not become widely recognized until the 1990s, when randomized trials in early-stage BC proved that radiotherapy-related cardiac damage almost completely outweighed its survival benefits.Citation9 Recently, the potential problem of radiation-induced cardiac disease has received much attention which is contributing to attempts to reduce heart dose.Citation10
The mechanism of radiation-induced myocardial impairment is not thoroughly understood. It may result from the effect on microvasculature with diffuse interstitial fibrosis, which begins with the injury of endothelial cells within heart blood capillaries, which leads to an acute inflammatory reaction, followed by endothelial cells proliferation and obstruction of myocardial capillary lumen. In a later stage, ischemia and myocardial cell death result from vessel lumen obstruction and formation of thrombi, that result in replacement of cardiac tissue by fibrotic tissue and may lead to chronic heart failure.Citation11,Citation12 Radiation may cause damage to major arteries, by inducing inflammation and oxidative damage in large vessels. In combination with high cholesterol, that could increase oxidation of LDL which allows them to be engulfed by macrophages, thus triggering the atherosclerotic process.Citation13 Myocardial cells involved with conduction may be damaged, leading to arrhythmias. Pericardium injury may emerge as excessive pericardial effusion, fibrotic thickening, pericardial adhesions, and pericarditis.Citation14,Citation15
The mean dose of radiation delivered to the heart was estimated for all patients and it was significantly higher in left-sided than in right-sided BC patients. For left-sided patients the heart was contiguous to the tangential fields, and the average mean heart dose was 4.46 Gy. In contrast, for the patients who received right-sided irradiation, the heart was remote from the fields and received only scattered dose, so the average mean heart dose was 0.6 Gy. In a similar study, Taylor el al.Citation16 reported an average mean heart dose of 2.3 Gy in left-sided patients, which was much lower than that reported in this study, and 1.5 Gy in right-sided patients.
In the present work, a highly significant correlation was noted between the total dose of radiotherapy and the mean dose delivered to the heart in left-sided BC patients, which implies that increasing the total dose of radiotherapy would increase the mean heart dose in left-sided but not in right-sided patients. Therefore, treatment planning should consider the heart dose delivered as a modifying factor in left-sided BC patients, so as not to deliver a heart dose higher than the tolerable dose of various cardiac tissues.
Among the most common manifestations of radiation-driven cardiotoxicity is the development of left ventricular dysfunction which presents as an asymptomatic decrease in LVEF from the baseline value measured before the beginning of treatment. LVEF significantly decreased from baseline in left-sided breast cancer patients after one year of completing radiotherapy, but not in right-sided patients. This significant decrease in LVEF in left-sided patients is thought to reflect the possible effects of radiation on the heart. Cardiac toxicity is speculated if LVEF drops either more than 10% from baseline to levels below 50% or 20% or more from baseline despite still normal. It was assumed that radiation-induced cardiac toxicity would need several years to develop. However, in this study despite the very short follow up time of only one year, according to the forementioned criteria, cardiac toxicity was assumed in 6 patients, which were all left-sided.
Several studies have investigated cardiac function in left- and right-sided BC patients receiving radiotherapy, and their findings were similar to the results in this study.Citation6,Citation10,Citation14,Citation16,Citation17 The frequency of cardiac toxicity in our study seems much lower than previous reports, which might be related to the fact that follow up time of our study is shorter than previous studies; some of the cardiac injury may still be in subclinical phase and the actual cardiac damage may be under evaluated.
Detectable changes in LVEF usually accompany significant functional impairment, at which point the ability to regain normal cardiac function becomes limited. Thus, the classical way for detecting cardiotoxicity is suboptimal and there remains a need to effectively identify patients at risk of developing serious cardiac ramifications following radiotherapy. Radiation-induced injury develops over a prolonged time period, making diagnosis more difficult, and the ability of the heart to compensate may further delay injury recognition for years. Many biomarkers have emerged as an alternative approach and a promising complement to routine echocardiography, to describe the risk of cardiac dysfunction in clinically asymptomatic patients. Classic cardiac biomarkers, TnI, CK, CK-MBRI and LDH, were investigated as possible markers of subclinical radiation-induced cardiotoxicity.
All biochemical parameters under investigation were significantly different from controls both before and after radiotherapy, where TnI, CK-MBRI and LDH were significantly higher and CK was significantly diminished than their corresponding controls, however, left- and right-sided BC patients were not significantly different regarding any of the markers tested. Since all patients received chemotherapy followed by radiotherapy, so it was hard to draw exclusive conclusions regarding the effect of radiotherapy alone and this pattern may reflect the fact that cardiac damage has already begun as a result of chemotherapy, before radiotherapy started.
Many biochemical parameters have been previously assessed during and after chemotherapy to evaluate its cardiac side-effect.Citation8,Citation18–Citation22 Cardiac TnI has demonstrated clinical value in predicting subsequent cardiotoxicity after high-dose chemotherapy,Citation18,Citation19 while decreased CK levels and elevated CK-MBRI values were reported in breast cancer irrespective of treatment,Citation20,Citation21 and LDH was reported to increase with chemotherapy.Citation22 Since publications dealing with radiotherapy alone are relatively scarce, only TnI had been evaluated as a marker of radiation-induced cardiotoxicity, with a discrepancy in results that made them hard to interpret. In the current study, before radiotherapy all parameters were significantly different from their normal levels, which limited their value in detecting radiation-induced cardiac damage. Thus usage of cutoffs was necessary.
Using the fore-mentioned cutoffs, TnI and CK-MBRI both remained elevated 1 year after radiotherapy in 5 right-sided and 11 left-sided patients, which may reflect the onset of cardiac damage in these patients. Cardiotoxicity was already confirmed by ΔLVEF > 20% in 6 of them. The in 5-patients of the right-sided group is probably more relevant to the onset of chemotherapy-induced cardiac damage, since the dose received by the heart in this group was quite small, but in left-sided group 11 patients showed elevation of TnI and CK-MBRI, since the effect of chemotherapy is expected to be similar in both groups, the excess fraction in the left-sided group is probably more connected to radiation-induced cardiac damage. However, verification of that assumption might require longer follow up. CK and LDH were not beneficial in predicting or recognizing patients at risk of radiation induced cardiac damage.
In conclusion, during radiotherapy, the mean dose delivered to the heart in left-sided BC patients is significantly higher than right-sided BC patients (4.46 vs 0.6 Gy), and cardiac dose was correlated to the total dose. After 1 year of completing radiotherapy, ΔLVEF was a good marker to detect the onset of cardiotoxicity, however, the persistent elevation of both TnI ≥ 0.08 ng/ml and CK-MBRI ≥ 1.4 was a more sensitive indicator that identified both patients with cardiotoxicity and a higher fraction of patients that are thought to be in subclinical phase of cardiac damage either due to chemotherapy alone or combined with radiotherapy. Neither CK nor LDH showed any significant value in identifying patients at risk of radiation induced cardiac damage.
Conflict of interest
The authors declare that there is no conflict of interest.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 10 January 2018
References
- U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2014 Incidence and Mortality Web-based Report. Atlanta (GA): Department of Health and Human Services, Centers for Disease Control and Prevention, and National Cancer Institute; 2017.
- J.FerlayI.SoerjomataramR.DikshitCancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012Int J Cancer1362015E359E386
- A.S.IbrahimH.M.KhaledN.N.H.MikhailH.BarakaH.KamelCancer incidence in egypt: results o f the national population-based cancer registry programJ Cancer Epidemiol2014201418https://doi.org/10.1155/2014/437971
- E.C.HalperinC.A.PerezL.W.BradyPrinciples and Practice of Radiation Oncology5th ed.2008Lippincott Williams & WilkinsPhiladelphia
- T.A.KoulisT.PhanI.A.OlivottoHypofractionated whole breast radiotherapy: current perspectivesBreast Cancer (Dove Med Press)72015363370
- K.BouillonN.HaddyS.DelalogeLong-term cardiovascular mortality after radiotherapy for breast cancerJ Am Coll Cardiol572011445452
- M.GalderisiF.MarraR.EspositoV.S.LomorielloM.PardoO.de DivitiisCancer therapy and cardiotoxicity: the need of serial Doppler echocardiographyCardiovasc Ultrasound52007417
- E.S.ChristensonT.JamesV.AgrawalB.H.ParkUse of biomarkers for the assessment of chemotherapy-induced cardiac toxicityClin Biochem482015223235
- Early Breast Cancer Trialists' Collaborative Group. Radiotherapy for early breast cancer. Cochrane Database Syst Rev 2002; 2: CD003647.
- A.SardaroM.F.PetruzzelliM.P.D'ErricoL.GrimaldiG.PiliM.PortaluriRadiation-induced cardiac damage in early left breast cancer patients: risk factors, biological mechanisms, radiobiology, and dosimetric constraintsRadiother Oncol1032012133142
- A.BurgerH.LöfflerM.BambergH.P.RodemannMolecular and cellular basis of radiation fibrosisInt J Radiat Biol731998401408
- S.C.DarbyD.J.CutterM.BoermaRadiation-related heart disease: current knowledge and future prospectsInt J Radiat Oncol Biol Phys762010656665
- K.GabrielsS.HovingI.SeemannLocal heart irradiation of ApoE(-/-) mice induces microvascular and endocardial damage and accelerates coronary atherosclerosisRadiother Oncol1052012358364
- M.MartinouA.GayaCardiac complications after radical radiotherapySemin Oncol402013178185
- J.R.StewartL.F.FajardoS.M.GilletteL.S.ConstineRadiation injury to the heartInt J Radiat Oncol Biol Phys31199512051211
- C.W.TaylorA.NisbetP.McGaleS.C.DarbyCardiac exposures in breast cancer radiotherapy: 1950s to 1990sInt J Radiat Oncol Biol Phys69200714841495
- D.WoolfR.BakhshiS.FawcittAn observational study using γ-H2AX foci to investigate cardiac doses of radiation following adjuvant radiotherapy for breast cancer: standard external beam radiotherapy to the breast versus intraoperative radiotherapyJ Clin Oncol2915-suppl2011TPS129
- D.CardinaleM.T.SandriA.ColomboPrognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapyCirculation109200427492754
- S.TianK.M.HirshfieldS.K.JabbourSerum biomarkers for the detection of cardiac toxicity after chemotherapy and radiation therapy in breast cancer patientsFront Oncol42014277
- H.PanK.XiaW.ZhouLow serum creatine kinase levels in breast cancer patients: a case-control studyPLoS One82013e62112
- C.C.ChangC.B.LiouM.J.SuCreatine Kinase (CK)-MB-to-Total-CK Ratio: a laboratory indicator for primary cancer screeningAsian Pac J Cancer Prev16201565996603
- J.B.DennisonJ.R.MolinaS.MitraLactate dehydrogenase B: a metabolic marker of response to neoadjuvant chemotherapy in breast cancerClin Cancer Res19201337033713
