Abstract
Background
Pineal region tumors represent 1.5–8.5% of the pediatric brain tumors. Management includes endoscopic third ventriculostomy and biopsy in cases presenting with hydrocephalus. In addition, surgical resection provides survival advantage in selected cases. The supracerebellar infratentorial approach is a widely preferred approach for such region.
Methods
After approval of the local ethics committee of Alexandria University and acquisition of the appropriate formal consents according to the committee’s standards, we have reviewed the records of fifteen cases presenting with pineal region tumors in Alexandria main university hospital from 2013 to 2016. The mean age at the diagnosis was 14 years (2–54 years). All cases had supracerebellar infratentorial approach for surgical resection. Follow up period was from 12 to 59 months.
Results
All 15 cases presented with hydrocephalus and increased intracranial pressure manifestations. Out of the 15 cases, 3 cases were germ-cell tumors, 2 cases were pineoblastomas, one parenchymal tumor with intermediate differentiation (PPID), one pineocytoma, 2 cases were anaplastic ependymomas and 6 cases were astrocytomas. Gross total resection (GTR) was achieved in 4 cases, subtotal resection was achieved in 7 cases and partial resection in 4 cases. Major surgical complications included severe post-operative cerebellar edema in 2 cases that required further decompression and hemorrhage in one case that has been managed conservatively.
Conclusion
In Alexandria university, the supracerebellar infratentorial approach is considered a safe approach with minimal morbidity and no surgery related mortality.
1 Introduction
Tumors of the pineal region and the posterior third ventricle are rare and account for 0.4–1% of intracranial tumors of adults and 1.5–8.5% of tumors in childrenCitation1 The absence of national brain tumor registry in Egypt makes it challenging to obtain valid local data.
The first successful removal of pineal tumors happened in 1913 by Oppenheim and Krause. The later was the first to describe the supracerebellar infratentorial approach which, has been further developed and modified in the microsurgical era by Stein.Citation2 After the 1970s, the increased use of the operative microscope increased the interest into direct surgical approaches to the pineal region.Citation3 The capability of removing such tumors through more aggressive approaches led to better tissue diagnosis and greater awareness of the histological diversity of such tumors.Citation4 Some of these tumors were found to be with mixed nature, containing benign as well as malignant or even glial elements.Citation5
The widely preferred approach to the region is the infratentorial supracerebellar approach. The patient is placed either in the sitting position or the concord position.Citation6 The pros of this approach include: it is directed towards the epicenter of the tumor and allows easy orientation, it is ventral to the velum interpositum and the deep venous system and no normal tissue is violated. It is extra-axial to the third ventricle and not associated with any morbidity that is related to the retraction of the parietal or the occipital lobes.Citation7 The cons of the approach include: poor visualization of any supratentorial component, the floor of the third ventricle and the paramedian parts of the lesion. The surgeon may need to split the vermis if the tent is highly angulated.Citation8 The most difficult part of the surgery is the dissection of the inferior surface of the tumor, as it may get adherent to the midbrain tectum and difficult to be visualized.Citation6
2 Methods
2.1 Patients
We reviewed the records of fifteen consecutive cases that were admitted to Alexandria main university hospital from 2013 to 2016 presenting with pineal region tumors and hydrocephalus (). There were 13 males and 2 females. Mean age of at diagnosis was 14 years (2–54 years). Twelve cases were considered within the pediatric age group (<18).
Table 1 Summary of cases in our series.
2.2 Preoperative data
The clinical presentation of all cases is summarized in . All cases had Magnetic resonance imaging (MRI) with contrast enhancement before the procedure. CSF diversion was done in 13 cases before surgery. The diversion was done either using ETV or VP shunt according to the patient age and availability of the endoscope in the emergency setting.
2.3 Indications for surgery
| 1. | Negative tumor markers and absence or inconclusive biopsy after ETV). | ||||
| 2. | If the pathology was known to show survival advantage if it is resected. | ||||
| 3. | More than 50% increase in size and/or worsening of neurological manifestations in tectal gliomas | ||||
| 4. | Minimal or no response to adjuvant therapy of germ-cell tumors. | ||||
2.4 Surgical technique
Position: The patients were placed in the concord position.Citation6 With either the head tilted to the opposite side or skewed slightly to allow neutral visualization of the pineal gland while the surgeon is standing on the left side of the patient. Due to absence of 3 pin-head holder we used a regular doughnut head rest. Extra care was done to avoid any continuous compression on the patients’ eyes ().
Skin incision: Along midline incision was placed between the spinous process of the third cervical vertebrae downwards to the occipital region upwards. The muscle and the pericranium were elevated on each side.
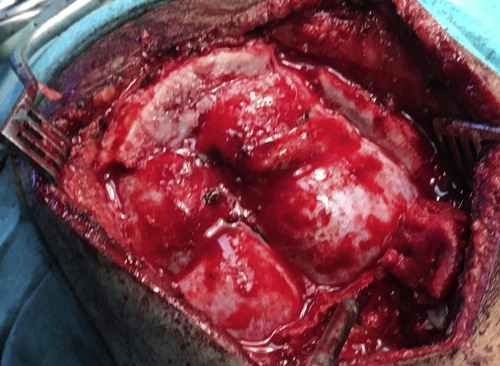
Craniotomy: A wide craniotomy was done () using Hudson’s Burr-hole and Gigli saw. It was supposed to show the lower part of the superior sagittal sinus, the torcula and the transvere sinuses, extending downwards below the sinuses but not as far as the foramen magnum.
Fig. 2 Exposure of the transverse sinus and the confluence of sinuses after the craniotomy procedure.
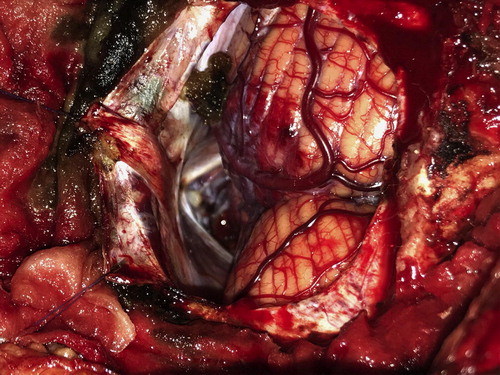
Technique: Elevation of the head of the bed, dehydration using mannitol, CSF drainage from the cisterna magna and occasionally ventricular drainage were used to relax the brain. () The dura was usually opened in a transverse fashion on each side of the midline, allowing the ligation and cutting of the cerebellar sinus together with the cerebellar falx. After opening the dura, the microscope was introduced. We used a Zeiss® OPMI Vario® S88 microscope in all cases. The cerebellum was then freed from the tent by adequate dissection of the arachnoid and using cottonoids. We tried to preserve bridging veins as much as possible, however, it was necessary to sacrifice some of them over the dorsum of the cerebellum for adequate visualization. The quadrigeminal cistern is usually surrounded by thickened and sometimes opaque arachnoid. It must be opened microsurgically and well dissected to allow adequate exposure of the tumor and to be able to appreciate all the anatomy. The precentral vein was usually seen extending from the vermis to the vein of Galen. Basal veins of Rosenthal were usually seen at the medial aspect of the temporal lobe. Through our experience we refined the approach through paramedian extension of the corridor to allow working around the bridging veins to preserve them. Usually, the most difficult part of the surgery was the dissection of the inferior surface of the tumor, as it may get adherent to the midbrain tectum and difficult to be visualized. If the tumor is benign or well encapsulated, it may be removed completely. Oxidized cellulose in the form of Surgicel® can be put carefully on the raw areas in a fashion that does not allow it to float into the third ventricle, not to obstruct the aqueduct. After surgery was done, dura was closed in a watertight fashion, bone flap is repositioned and fixed using absorbable sutures.
2.5 Follow up
Immediate post-operative CT was done in all cases to check for tumor bed hematoma and other complications as cerebellar edema or hydrocephalus. Post-operative MRI brain was done in all cases to assess the degree of tumor removal, presence of residual tumor or recurrence. Gross total resection is defined when no residual is seen in the post-operative images. Subtotal resection is defined when more than 80% of the lesion has been resected. If more than 20% of the residual is found it was considered a partial resection. Follow up period was 12–59 months. One case has died 7 months after the procedure due disease progression.
3 Results
All 15 cases presented with hydrocephalus and increased ICP manifestations. Six cases presented to the emergency department with disturbed level of consciousness. Five cases had Parinaud syndrome at presentation, 2 cases had abducent palsy and 2 cases presented to the ED with disturbed level of consciousness.
The ETV was done in 6 cases and was successful in 5 of them (83.3%) with resolution of hydrocephalus. On case has failed and required VP shunt later on. On the other hand, VP shunt was inserted in 7 cases, in 6 of them VP shunt was inserted upfront and one case after failure of ETV.
Out of the 15 cases, 3 cases were germ-cell tumors, 2 cases were pineoblastomas, one parenchymal tumor with intermediate differentiation (PPID), one pineocytoma and 2 cases were anaplastic ependymomas.
Gross total resection (GTR) was achieved in 4 cases, subtotal resection was achieved in 7 cases and partial resection in 4 cases. The 4 cases that had limited resection included the anaplastic astrocytomas and grade 2 tectal gliomas ().
Two of the diagnosed germ-cell tumors had STR and one case had GTR. None of these cases showed any progression at subsequent imaging in follow up period of 15.1–48.9 months. Four cases were diagnosed with pineal parenchymal tumors A pineocytoma and a pineoblastoma had GTR while another pineoblastoma and PPID had subtotal resection. Both cases that had STR had progressed after 3 and 32 months respectively.
In our series, the 6 tectal gliomas cases were in the form of: 1 pilomyxoid astrocytoma that had GTR, 1 pilocytic astrocytoma that had STR, two cases were grade 2 tectal gliomas and 2 cases were anaplastic astrocytoma. All the grade 2 and anaplastic gliomas had partial tumor resection. Only one of the anaplastic astrocytomas showed progression after a period of 41.6 months.
The 2 cases that were diagnosed with anaplastic ependymoma had subtotal resection. One progressed after 9 months and the second one progressed after 12 months. Both required redo surgery, GTR of the residual was achieved only in the first case.
Surgical complications included severe post-operative cerebellar edema in 2 cases. The first one had the precentral vein coagulated during the approach. In the second one the precentral vein was identified, the paramedian corridor was chosen for resection, however, post-operative edema was explained by the continuous static retraction that was used during surgery. Both of which had declined level of consciousness in the immediate post-operative period and required surgical decompression. Both cases had persistent truncal ataxia later on. One case had small hemorrhage in the tumor bed that was treated conservatively. One case had pseudomeningocele that required aspiration twice and was completely resolved later on.
The 1-year progression free survival of the whole series was 86.7%. Five cases have progressed in this series. These cases included 2 anaplastic ependymomas, 1 anaplastic astrocytoma, 1 pineoblastoma and 1 PPID. All of which have received adjuvant therapy according to the tumor type post-operatively. None of the progressed cases had GTR in the immediate postoperative images.
4 Discussion
The anatomical location of the tumor, the degree of familiarity of the surgeons towards certain approach and the patient’s anatomical variation, all aid in the choice of the best approach. In general, the three adopted approaches to the pineal region include: the infratentorial supracerebellar, the occipital transtentorial, the transcallosal interhemispheric approaches and less commonly the transcortical transventricular approach.Citation9
In our series, we have chosen the concord position for all cases that had the supracerebellar infratentorial approach. Sitting position was not used because of the lack of positioning equipment. In addition, absence of anesthetic equipment such as trans esophageal echo to guard against air embolism made the sitting position a dangerous choice.Citation6 Continuous cerebellar retraction was avoided during most of the surgeries by draining enough CSF from both cisterna magna and quadrigeminal cisterns in addition to elevation of the head of the bed and meticulous arachnoid dissection.
The initial management for cases with pineal region tumors presenting with obstructive hydrocephalus should be CSF diversion and CSF sampling. If the CSF tumor markers are elevated, the patient is diagnosed with GCT and usually proceeds to adjuvant treatment.Citation6,Citation10 Surgery is indicated if tissue sampling was inconclusive by endoscopic biopsy and the tumor markers are within normal which was the cases in two of our cases. Also, it is indicated if there is a residual tumor after adjuvant treatment especially if it is showing progression on serial imaging.Citation6,Citation10,Citation11 Only one of our cases had showed elevated tumor markers however; he required surgery later on as described above.
Out of 196 cases of pineal region GCTs obtained from 3 registries in the US, 90.8% of cases had microscopic confirmation after biopsy acquisition.Citation1 Surgical resection was done in 42–45% of the cases.Citation1
Open surgery is still considered the treatment of choice for pineal parenchymal tumors, for adequate tissue acquisition and better progression free survival. In pineocytomas it is considered the treatment of choice with superior progression free survival as regards gross total resection. None of the patient diagnosed with pineocytoma was reported to have a recurrence in the literature, in comparison with 9.5% rate of recurrence after subtotal resection and radiotherapy. Also pineoblastomas have been observed to be associated with prolonged overall survival when grossly resected.Citation12 The rate of major postoperative morbidity is considered to be low, lying between 0 and 5% in several studies.Citation12,Citation13 The reported median overall survival for pineoblastomas is 20 months and 10% 5-year survival.Citation12 None of our surgical cases had any major post-operative complication.
Brain stem gliomas represent 10–20% of all pediatric primary brain tumors. Tectal gliomas are considered a subgroup of focal brain stem gliomas and represents 5% of all brain stem glioma in pediatrics.Citation14 Most commonly they are low grade in nature (80%) with good prognosis,Citation15 for this reason it has been frequently mentioned in the literature as “indolent”.Citation14 Pilocytic astrocytoma is the most frequent pathology (36%), followed by grade 2 astrocytoma (21%), oligastrocytoma and high-grade astrocytoma (7%) is the least frequent.Citation14 Lines of treatment include: observation, CSF diversion for hydrocephalus, tumor biopsy, resection, radiotherapy and chemotherapy.Citation16
Low grade-tectal plate gliomas are typically indolent and only few will show progression (18–31%).Citation14,Citation15 The later requires treatment in the form of surgery and/or radiotherapy and chemotherapy. ETV has proved to be an effective procedure for CSF diversion with reported success 70–90%.Citation17–Citation19
Other than CSF diversion, the management of tectal gliomas is still controversial.Citation14,Citation20 Some authors have recommended only observation after CSF diversion and consider that histopathological differentiation is only for academic interest.Citation21 Others advocated for biopsy and radiotherapy.Citation22 Some authors considered a 50% growth in size after serial MRI brain is indicative for surgical excision.Citation15 The aim of the surgical choice rather than radiotherapy is to limit radiation to the developing brain if surgery can be safely achieved.Citation14In addition, authors who recommended surgical intervention have observed significant correlation between the lesion volume at the time of presentation and progression on follow up imaging.Citation14 Thus, the volume has significantly influenced the decision for surgery.
Although radiological progression has been an important indication for surgery in many series, still it is controversial as usually it is not associated with progression of clinical symptomsCitation14 Ternier et al. have divided tectal gliomas into 3 subgroups <4 cm3, 4–10 cm3, >10 cm3 most of the cases >4 cm3 were considered surgical.Citation14 The authors in this study have recommended only follow up images for the small subgroup, frequent follow up for the moderate size subgroup or surgery if progression has been observed. They also have recommended surgery for the large subgroup.Citation14 Out of the 40 cases in Ternier’s series, 14 cases were deemed surgical the majority of which was found to be benign. Post-operative morbidity was in the form of transient Parinaud, nystagmus and transient hemisensory deficit.
Intra-operatively tectal lesions are almost identical to normal brain tissue which makes it surgically challenging.Citation14 Ternier et al. have reported that gross total resection has been rarely achieved. In our series, out of the 6 surgical cases only one case had GTR, 2 cases had STR and the three others had partial resection. Invasion of surrounding tissue and presence of neurological deficit are considered poor prognostic factors.Citation14
Ependymomas represents 6–10% of all intracranial tumors in pediatrics.Citation23 The current standard of care for ependymomas is surgical resection followed by radiotherapy alone.Citation23 In a systematic review done on 197 peer-reviewed articles, the most significant factor that improved the progression free survival (PFS) rate in supratentorial ependymomas (12.7 years) was GTR.Citation23 On the other hand STR followed by adjuvant radiotherapy resulted in better overall in infratentorial ependymomas.Citation23 The favorable outcome with STR in the later group was explained by the decreased morbidity associated with the more conservative surgical approach.Citation23
In our series, we had 2 cases that were diagnosed with anaplastic ependymoma. Both had STR, however, they had short progression free survival and required redo surgeries. This could be explained by the natural history of anaplastic ependymomas.
Out of the 15 surgical cases, 4 cases (25%) had gross total resection (GTR), 7 cases had subtotal resection (STR) (44%) and 4 cases (31%) had partial resection. The extent of resection is lower than others reported in the literature, in which GTR ranges from 37% to 91%.Citation11,Citation24 This could be explained by the fact that 6 cases were tectal gliomas which are known to be rarely excised gross totally.Citation14 Some of these studies were done on spectrum of cases in which benign tumors were either the majority or all of the cases.Citation24 Other studies were done in high volume centers that usually result in better surgeons’ experience.Citation13,Citation25
Despite of the fact that it has been reported in the literature that bridging veins between the tentorium and the cerebellum can be safely sacrificed.Citation24,Citation26 Several authors have reported similar complications including odema and venous infarction of the cerebellum and advocated preserving them.Citation13 Jakola et al., has reported cerebellar venous infarction after the scarification of a single bridging vein through a paramedian approach.Citation27 Therefore, it is better to sacrifice smaller thin walled veins and to preserve large ones keeping in mind that there it is difficult to predict which vein when occluded will result in serious complication.Citation26,Citation28 Avoidance of static retraction prevents continuous stretch of the bridging veins that could result in their injury or thrombosis. In addition, ischemic insult that result from continuous retraction may contribute to the post-operative cerebellar edema.Citation26 If retraction is needed it is better to be dynamic by the use of the shaft of the suction tip.Citation26 The precentral vein is considered to be safe to be sacrificed, however, Kanno et al. have described a case report in which the occlusion of the precentral vein resulted in progressive thrombosis of the basal veins of Rosenthal and eventually ended up in massive fatal hemorrhagic infarction.Citation28 For this reason, it is better to excise the tumor in a piece meal fashion through the corridor between the precentral vein and the basal veins. If it has to be sacrificed, it should be cut as distal as possible form the vein of Galen.Citation26
5 Conclusions
Indications of surgery to pineal region and tectal lesions include: histopathological diagnosis if it could not be reached through minimal invasive procedures, maximum safe resection as in pineal parenchymal tumors for better survival rates and as a salvage procedure for GCTs if there is no or minimal response to adjuvant treatment. Surgery is still controversial in low-grade tectal gliomas. The supracerebellar infratentorial approach is considered the approach of choice for most of tumors occurring in such region in most centers of the world. Our experience in Alexandria university shows that it is a safe approach with minimal morbidity no surgery related mortality. The most important complication we observed was cerebellar edema. The incidence of such complication can be minimized by preservation of the bridging veins and avoidance of the static retraction.
Conflict of interest
The authors declared that there is no conflict of interest.
supplementary-material 1
Download MS Word (3.7 MB)Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 21 March 2018
References
- J.L.VillanoJ.M.ProppK.R.PorterMalignant pineal germ-cell tumors: an analysis of cases from three tumor registriesNeuro Oncol102008121130
- F.KrauseOperative Frielegung der Vierhügel, nebst Beobachtungen über Hirnduk und DekompressionZentrabl Chir53192628122819
- W.S.ReidW.K.ClarkComparison of the infratentorial and transtentorial approaches to the pineal regionNeurosurgery3197818
- B.M.SteinM.R.FetellTherapeutic modalities for pineal region tumorsClin Neurosurg321985445455
- Bruce JN, Connolly, E.S., Stein, B.M. Pineal and germ cell tumors. In: Kaye AH, Laws, ER, editors. Brain tumors. London: Chirchill livingstone; 1995. p. 725–55.
- J.N.BruceManagement of pineal region tumorsA.Quinones-HinjosaSchimdek and Sweet operative neurosurgical techniques: indications, methods and results6th ed.2012ElsevierPhiladelphia, PA357366
- I.YamamotoPineal region tumor: surgical anatomy and approachJ Neurooncol542001263275
- H.Aboul-EneinA.A.El-Aziz SabryFarhoud A.HafezSupracerebellar infratentorial approach with paramedian expansion for posterior third ventricular and pineal region lesionsClin Neurol Neurosurg1392015100109
- J.N.BruceA.T.OgdenSurgical strategies for treating patients with pineal region tumorsJ Neurooncol692004221236
- M.A.ZaazoueL.C.GoumnerovaPineal region tumors: a simplified management schemeChilds Nerv Syst32201620412045
- A.M.SonabendS.BowdenJ.N.BruceMicrosurgical resection of pineal region tumorsJ Neurooncol1302016351366
- M.C.TateM.J.RutkowskiA.T.ParsaContemporary management of pineoblastomaNeurosurg Clin N Am222011409412 ix
- J.N.BruceB.M.SteinSurgical management of pineal region tumorsActa Neurochir (Wien)1341995130135
- J.TernierA.WrayS.PugetN.BodaertM.ZerahC.Sainte-RoseTectal plate lesions in childrenJ Neurosurg104Suppl. 62006369376
- A.KershenovichZ.SilmanD.de RungsK.KoralL.GarganB.WeprinTectal lesions in children: a long-term follow-up volumetric tumor growth analysis in surgical and nonsurgical casesPediatr Neurosurg5120166978
- C.J.GriessenauerE.RizkJ.H.MillerPediatric tectal plate gliomas: clinical and radiological progression, MR imaging characteristics, and management of hydrocephalusJ Neurosurg Pediatr1320141320
- D.HellwigJ.A.GrotenhuisW.TirakotaiEndoscopic third ventriculostomy for obstructive hydrocephalusNeurosurg Rev282005134 discussion 35-38
- A.V.KulkarniJ.M.DrakeC.L.MallucciEndoscopic third ventriculostomy in the treatment of childhood hydrocephalusJ Pediatr1552009254259 e251
- O.SackoS.BoettoV.Lauwers-CancesM.DupuyF.E.RouxEndoscopic third ventriculostomy: outcome analysis in 368 proceduresJ Neurosurg Pediatr520106874
- C.IgboechiA.VaddipartiE.P.SorensonC.J.RozzelleR.S.TubbsM.LoukasTectal plate gliomas: a reviewChilds Nerv Syst29201318271833
- F.A.Gomez-GosalvezF.MenorA.MorantTectal tumours in paediatrics. A review of eight patientsRev Neurol332001605611
- P.L.RobertsonK.M.MuraszkoJ.A.BrunbergR.A.AxtellR.C.DauserA.T.TurrisiPediatric midbrain tumors: a benign subgroup of brainstem gliomasPediatr Neurosurg2219956573
- T.A.CageA.J.ClarkD.ArandaA systematic review of treatment outcomes in pediatric patients with intracranial ependymomasJ Neurosurg Pediatr112013673681
- J.HernesniemiR.RomaniB.S.AlbayrakMicrosurgical management of pineal region lesions: personal experience with 119 patientsSurg Neurol702008576583
- S.QiJ.FanX.A.ZhangH.ZhangB.QiuL.FangRadical resection of nongerminomatous pineal region tumors via the occipital transtentorial approach based on arachnoidal consideration: experience on a series of 143 patientsActa Neurochir (Wien)156201422532262
- T.KoderaO.BozinovO.SurucuN.H.UlrichJ.K.BurkhardtH.BertalanffyNeurosurgical venous considerations for tumors of the pineal region resected using the infratentorial supracerebellar approachJ Clin Neurosci18201114811485
- A.S.JakolaJ.BartekJr.T.MathiesenVenous complications in supracerebellar infratentorial approachActa Neurochir (Wien)1552013477478
- S.MatsuoS.BaydinA.GungorMidline and off-midline infratentorial supracerebellar approaches to the pineal glandJ Neurosurg126201719841994
Appendix A
Supplementary material
Supplementary data associated with this article can be found, in the online version, at http://doi:10.1016/j.ajme.2018.02.003.