Abstract
Purpose
To delineate the significant association between the peroneal tendons injury and the lateral ankle joint anatomical variants.
Subjects
Retrospective revision of the last 600 ankle MRI examinations, with dividing such candidates into: Group A: Inclusion group including patients with pure Peroneal tendon injury & lateral ankle anatomical variants. Group B: Control group including patients with Peroneal Tendonsinjury & no anatomical variants. Group C: Exclusion group including patients with other different types of ankle injuries.
Technique
Standard MRI ankle joint protocols.
Results
Group A: 73 patients (40.3%) had PTT including: straight/convex RMG in 48 (26.5%) patients; 19 of them (39.6%) had PTT, PT hypertrophy in 39 (21.6%) patients; 14 (35.9%) of them had PTT. RCE hypertrophy in 33 (18.3%) patients; 12 of them (36.4%) had PTT. PQ muscle was seen in 15 (8.3%) patients; 7 (46.7%) of them had PTT. Low PB muscle belly was found in 29 (16%) patients; 13 (44.9%) of them had PTT. OP was found in 17 (9.3%) patients; 8 (47%) of them had PTT. Group B: 26 of them (18%) had PTT. Fisher exact test 0 P value.
Conclusion
The lateral ankle joint anatomical variants facilitate peroneal tendons injury, ending in chronic lateral joint instability.
1 Introduction
Peroneal muscles injury is one of the frequently miss-diagnosed Peroneal tendons injuries; despite that it is one of the common responsible causes of chronic lateral ankle pain and instability. Ankle twisting is the commonest encountered lateral ankle joint injury seen in practice, which may not heal completely; leaving persistent lateral ankle pain. Peroneal tendons complex, which are one of the major lateral ankle joint stabilizing factors, are commonly injured in this lateral ankle trauma. Different types of peroneal tendon complex injuries are responsible for a considerable percentage of this long lasting lateral ankle pain and instability. These peroneal complex injuries include tenosynovitis, full or partial thickness tears of the peroneal tendons, superior and inferior peroneal retinaculum injuries, and tendon subluxations or dislocations from the retromalleolar groove (RMG).Citation1,Citation2 History of trauma is commonly achieved in these patients with chronic lateral ankle pain, however if absent it is not an exclusive character for this traumatic etiology of the pain, as it still may be due to repetitive unnoticed micro-trauma. Careful orthopedic examination and meticulous imaging studies are crucial for accurate diagnosis. Some anatomical variants of the lateral ankle structures, which may facilitate peroneal tendons injuries, are commonly seen. Being acquainted by these anatomical variants and annotating this in the ankle MRI report is crucial. This may help the orthopedics for managing some correctable variants, in attempt to maintain lateral ankle joint stability and avoid the possible recurrent similar injuries facilitated by these variants, if not corrected.Citation3,Citation4
1.1 Anatomy
The Peroneal tendons complex includes the peroneus brevis muscle and tendon (PB), peroneus longus muscle and tendon (PL), the common synovial sheath which splits at the peroneal tubercle, the superior retinaculum and inferior retinaculum. This complex includes also the os peroneum, which is a small sesamoid bone within the vicinity of the PL tendon. The PB muscle has its origin from the distal two thirds of the fibula and the intermuscular septa of leg, while its tendon inserts at the tuberosity of the lateral surface of the base of the fifth metatarsal bone. The muscle assists in weak plantar flexion and eversion of the foot.Citation5
The PL arises from the head and upper two-thirds of the lateral surface of the body of the fibula, from the deep surface of the fascia and from the intermuscular septa and occasionally also have few fibers from the lateral condyle of the tibia. Between its fibular head and body attachment, there is a gap, through which the common fibular nerve passes to the front of the leg. PL has a long tendon, which runs with the tendon of the PB in a common synovial sheath behind the lateral malleolus, in a canal covered by the superior and inferior peroneal retinaculum (SPR&IPR). Distally, the tendon extends obliquely transverse on the lateral side of the calcaneus, to be inserted into the lateral side of the base of the first metatarsal bone and the lateral side of the medial cuneiform. The PL main action is the plantar flexion of the foot, in conjunction with some help in eversion.Citation5,Citation3
SPR plays an important role in stabilizing the peroneal tendons in the RMG, as a fibrous covering band which extends from the lateral malleolus posteriorly and inferiorly to be inserted at the lateral aspect of the calcaneus. The fibers of the IPR are continuous in front with those of the cruciate crural ligament; behind they are attached to the lateral surface of the calcaneus; some of the fibers are fixed to the peroneal trochlea, forming a septum between the tendons of the Peroneus longus and brevis. Also, the calcaneofibular ligament provides additional stability to the peroneal tendons in the RMG. The OP is a small sesamoid bone located inside the PLT, close to the cuboid. It is seen in 5–26% of the population and is bilateral in 60% of them. Painful os peroneum syndrome (POPS) is a term coined by Sobel et al. which results from a spectrum of conditions, including OP fracture or a diastasis of multipartite OP. These aforementioned OP abnormalities could result in or facilitate PL tendon tear or tenosynovitis, and POPS is frequently missed as a causative factor ().Citation6,Citation7
Fig. 1 Anatomy of the peroneal tendon (A) T1 SE sagittal image of the lateral ankle showing PB (Notched arrow) and PL (Arrow) tendons below the lateral malleolus with bright signal owing to the magic angle. (B) T2* axial image showing the superior peroneal retinaculum (arrow). (C) Consecutive coronal T2 weighted FSE showing the course of the PB (short arrows) & PL tendons (long arrows) from the fibular tip to their insertions. Axial T1 fat-saturated post-contrast image showing the oblique course of the PL tendon (arrow) in the plantar region.Citation3
2 Subjects and methods
2.1 Objective
The objective of this study is to check if the known lateral ankle joint anatomic variants are incriminated in facilitating repetitive peroneal tendons injury ending in chronic lateral ankle instability. This was carried through comparative study for patients with Peroneal tendons injury with and without lateral ankle anatomic variants.
2.2 Subjects
This study was carried out during the period from January 2014 to March 2017, at the radiology department of Al-Mana General Hospital, Eastern Province, Saudi Arabia. The study protocol was approved by the scientific and ethics committee in Al-Mana General Hospital. The study was conducted as a retrospective revision of 600 ankle MRI examinations that were done at the hospital during this period ().
Table 1 The study groups.
2.3 Inclusion criteria (Group A)
181 (30.1%) patients with Peroneal tendons injury & lateral ankle anatomical variants. The average group age was 34 years.
2.4 Control group (Group B)
The remaining 196 (32.7%) patients who were presented with Peroneal tendons injury with no anatomical variants. The average group age was 36 years.
2.5 Exclusion criteria (Group C)
223 (37.2%) ankle MRI examinations were excluded from the study due to their other ankle complaints, rather than the pure lateral injury type… e.g. Associated fractures and/or dislocation, history of previous surgery, infections … etc. at the ankle region. Average bone age was 29 years for this group ().
2.6 Imaging Technique
All examinations were performed through Intera 1.5T, Closed Magnet MRI, Philips Medical Systems, 5656 AE Eindhoven, the Netherlands, with a dedicated surface coil. All patients were placed within the MRI unit in feet first supine position with the foot in about 20° of plantar flexion. Plantar flexion helps to avoid the magic angle effect, as much as possible, and accentuates the fat plane between the peroneal tendons, as well as improving the visualization of the calcaneofibular ligament. A dedicated surface coil is used in all ankle MRI examinations at our department. Sagittal images were obtained at 90° to intermalleolar axis; including the surrounding skin of the hind foot. Coronals were aligned to the intermalleolar axis, while axials were aligned 90° to tibia. The used MRI sequences and parameters were tabulated in ().
Table 2 The parameters of the ankle MRI sequences.
3 Results
Group A (181 (30.1%) patients):Different anatomical variants were seen in this group's patients; Overall 73 of them (30.1%) had Peroneal tendons injury (PTT). Straight and convex RMG was found in 48 patients (26.5%), PTT occurred in 19 of them (39.6%), Peroneus tubercle (PT) hypertrophy (>5mm) was found in 39 (21.6%) patients; 14 of them (35.9%) had PTT. Retrotrochlear eminence (>5mm) hypertrophy had been detected in 33 (18.3%) patients; 12 of them (36.4%) had PTT. Peroneus Quartus accessory muscle was seen in 15 (8.3%) patients; 7 of them (46.7%) had PTT. Low PB muscle Belly was found in 29 (16%) patients; 13 of them (44.9%) had tendinous injury. Os Peroneum (OP) accessory bone was in 17 patients (9.3%); 8 of them (47%) had tendinous injury. Group B included 196 (32.7%) patients who had normal ankle structures with no variants and subjected to lateral ankle trauma. PTT had been only recorded in 26 patients (18%). Group C included 223 (37.2%), who did ankle MRI for other types of ankle injuries (). Statistic comparison in between the two groups A&B was made through Fisher exact test had given a p value of 0; considering that the result is significant at p < .05Citation8 ().
Table 3 Results of the study.
Table 4 Fisher exact test calculator.Citation7
4 Discussion
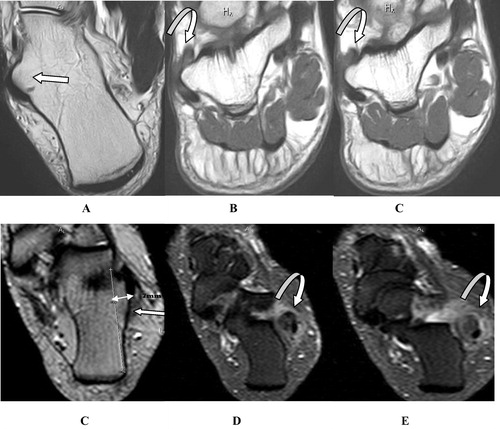
The peroneal muscles tendons are one of the major lateral ankle stabilizing factors; consequently their injury is associated with lateral ankle functional instability. Revision for 600 ankle MRI study was done in this study, in attempt to check if there is high susceptibility of the ankle joints, which have one of the known lateral bony or soft tissue structural variants, to have peroneal tendons tear. Comparative study was done through grouping the candidates into three groups; (A) The inclusion study group including the patients with positive lateral ankle structural variants (181 patients (30.1%)), (B) the control group including localized lateral ankle trauma, having no variants (196 (32.7%)) and (C) the exclusion group including all other ankle injuries rather than lateral injuries (223 (37.2%)). Normally, the retrofibular groove has a slightly concave configuration; forming a smooth shallow groove for the peroneal tendons securing their stability (). First subgroup of patients in group A, were those who were presented with fibular RMG variants i.e. flat or convex configuration which was recorded in 48 patients (26.5% of group A candidates). Peroneal tendons injuries was found in 19 of them (39.6%). This could be explained by the fact that the flat or convex configuration may predispose to lateral tendon subluxation. This together with the associated surface irregularity which is commonly encountered in these two variants facilitates different injury grades of the peroneal tendons. Also, this associated surface irregularity alone may be responsible for chronic lateral ankle pain due to persistent tendinous irritation.Citation8,Citation9 This matches the results published by Vega et al.Citation10 who stated that correction of these fibular groove variants with tendoscopic deepening of the groove had provided a favorable outcome for patients suffering from recurrent subluxation of the peroneal tendons. Hence, the importance of recommending stating the shape of the fibular groove to be a standard item in the ankle MRI reports (&).
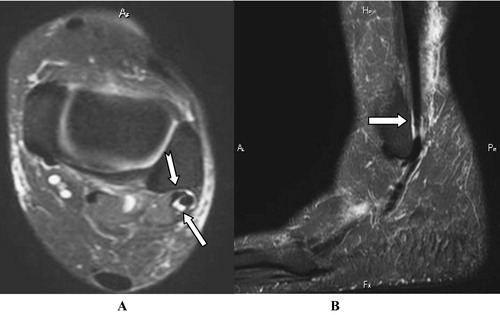
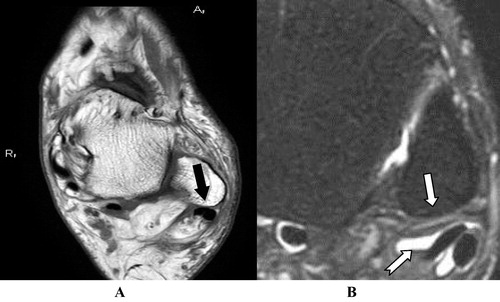
Fig. 2 (A) Axial T1-weighted and (B) STIR axial MR images depicts a normal concave retromalleolar groove (arrow), lodging the peroneal tendons (Notched Arrow).
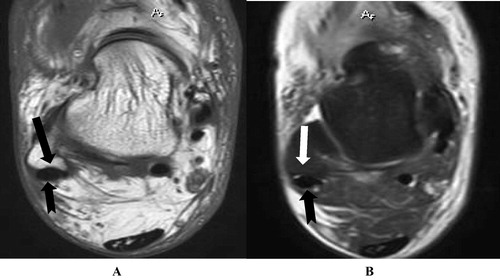
Fig. 3 Axial STIR images showing lost concavity of the fibular retromalleolar groove with straight border (curved Arrow), associated with PB tendon severe laceration (Arrow in A) and missed segment (Arrow in B), together with sweollen PL tendom (Notched Arrow in B).
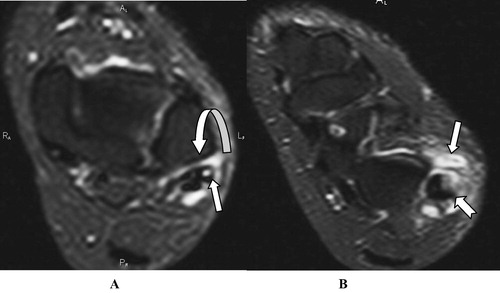
Fig. 4 (A) axial T1w and (B) Zoomed Axial STIR images showing slightly convex fibular groove (Arrow) with associated tendinopathy and synovial sheath effusion of both peroneal tendons (Notcched arrow).
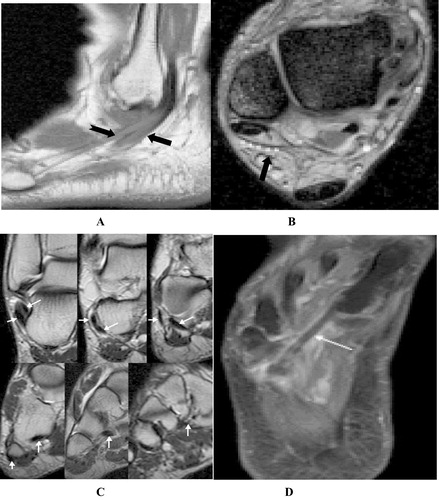
Two lateral calcaneal bony protuberances are also considered to play some role in lateral ankle stability. The posterior one, which is the RCE, is located posterior to the peroneal tendons. The anterior one, which is called the PT, is situated immediately inferior to the lateral malleolus. The common synovial sheath that covers the two peroneal tendons proximal to the tubercle splits to enclose each tendon separately at the tubercle and distally. The peroneus brevis lies anterior to the tubercle, and the peroneus longus lies posterior to the tubercle.Citation11,Citation12 A maximum width of 5 mm can be used as a cut off level to diagnose an enlarged PT or RCE, which was seen in 21.6% and 18.3% of group A patients; respectively. These enlarged tubercles, can impinge the peroneus tendons and may facilitate chronic inflammatory process like stenosing tenosynovitis or different grades of tendons tears. In candidates with enlarged PT or RCE variants, we recorded PTT incidences of 35.9% and 36.4%; respectively. These results match what was published by Celikyay et al. at their published study named: Tenosynovitis of the peroneal tendons associated with a hypertrophic PT: radiography and MRI findingsCitation13 ().
Fig. 5 (A) Axial T2w image (B&C) Zoomed coronal T1w show significantly prominent PT (Arrows) with its clear severe impinging effect on the related peroneal tendons showing grade I tendinopathy. (Curved Arrows) Another patient (C) Axial T2w shows an enlarged retrotrochlear eminence (arrow), as it measures 7 mm in width (double-headed arrow) relative to the lateral calcaneal cortex. (D&E) More distal Axial STIR images in the same patient showing associated swelling and severe laceration of the peroneal tendons. (Curved Arrows).
Many types of accessory muscles may be superimposed at the lateral compartment of the ankle, the most common one is the peroneus quartus muscle. It lies along the posteromedial aspect of the peroneal tendons, with variable appearance according to its belly and tendon lengths. It had been reported to have an incidence ranging from 12% to 22%. It had been seen in only 8.3% of this study candidates; 46.7% of them had tendinous injuries. The peroneus quartus muscle usually originates from the PB muscle and inserts at the RCE or at the base of the fifth metatarsal. Uncommonly, its muscle belly inserts directly onto the lateral aspect of the calcaneus.Citation14,Citation15 The peroneus quartus is usually incidentally discovered without special signs or symptoms, however it may cause injury of the adjacent peroneal tendons, due to soft tissues overcrowding at the RMG. This may lead to chronic irritation of the peroneus tendons with resultant tenosynovitis or predisposes to partial or complete or even longitudinal split tendinous tearsCitation16 (A). Our findings, regarding the impinging effect of this anomalous accessory muscles, may simulate what was published by Davda et al.Citation17, who recorded 6–22% incidence of the presence of this accessory muscle. Also, they enhanced this concept of the impinging effect of the peroneus quartus muscle over the peroneal tendons.
Fig. 6 (A) Axial T1 of right ankle showing PL tendon (Curved arrow), PB tendon (Arrow) and PQ tendon (Chevron) which causes crowding underneath the SPR (Stripped arrow). (B) Another patient’s left ankle axial T1w image showing low lying peroneus muscle belly (Chevron) with only two tendons (Arrows), also it causes crowding underneath the SPR (Stripped arrow). A meniscus-like low-signal-intensity triangular fibrocartilaginous ridge seen at the SPR lateral malleolar insertion site (Curved arrow).
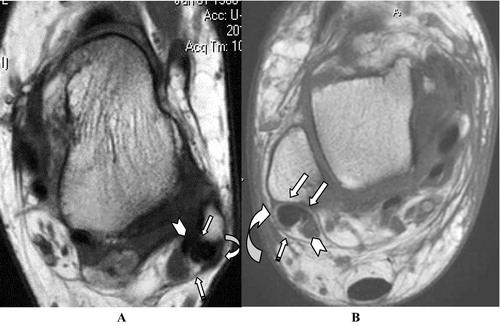
Another similar Peroneal tendons impinging factor could be seen, which is the low lying PB muscle belly. It may add more crowding to the structures of the RMG, as this may lead to significant stenosis in the RMG and increases the vulnerability of the PB tendon or SPR to be torn. The position of PB musculotendinous junction is highly variable, a low-lying PB muscle belly is considered, only if its belly is still seen at a location >15 mm distal to the distal fibular tip. In this study we diagnosed this PB muscle belly variant position in 29 (16%) patients, 44.9% of them had tendinous injuries (B). Nearby results of the presence of this accessory muscle (peroneus quartus) was published by Cheung et al.Citation18 Some orthopedics recommend elective resection of a low-lying peroneus brevis muscle belly and peroneus quartus muscle in the RMG, which will allow a better gliding ability of the peroneus brevis and longus tendons as they course around the ankle. This will help to avoid or limit the peroneal tendons injury around the ankle.Citation19,Citation20
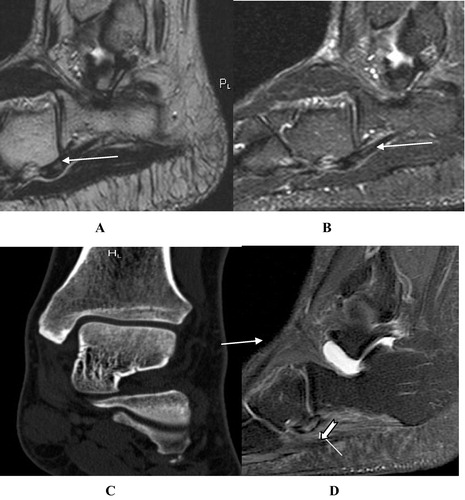
Os peroneum and os vesalianum are two sesamoid bones which infrequently may be seen in PL and PB tendons; respectively. They are considered to be another impinging elements as described in the literatures. Both are fibrocartilaginous type of sesamoids which may be missed in X ray, if still not ossified. MR imaging can confidently demonstrate them, as intra-tendinous oval well-corticated ossicle or cartilaginous structures if still not ossified. These two sesamoids should not be confused with other tendon pathologies such as avulsion fracture or apophysis of the 5th metatarsal bone.Citation21,Citation22 Although theses sesamoid bones are usually discovered incidentally; it may be complicated causing acute or chronic considerable regional lateral plantar foot pain, which is known as painful os peroneum syndrome (POPS). The POPS could be a result of acute trauma, or more frequently has chronic presentation secondary to repetitive injuries of the foot. OP was seen in 9.3% of our candidates; 47% of them had POPS. The POPS spectrum includes: an acute fracture or diastasis of a multipartite os peroneum, old fracture with callus formation. These all will end in stenosing PL tenosynovitis; partial or complete tear of the peroneus longus tendonCitation21,Citation23 (). In Group B patients who had no anatomical variants; only 18% had PTT. Fisher exact test revealed significant difference between the two groups; denoting the higher susceptibility of patients of group A ().
Fig. 7 (A) Sagittal T2w image shows an os peroneum, within the substance of the PL tendon, as it arches around the cuboid bone. (Arrow) (B) Sagittal PD fat sat image shows hyperintense signal within PL tendon. (Arrow) (C) CT scan ankle coronal reformat of the same patient showing two os peroneum accessory bones inferior to the cuboid bone. (Arrow) (D) MRI sagittal PD fat sat in another patient shows os peroneum marrow edema as hyperintense signal (Arrow head) and high signal within the PL tendon. (Arrow).
5 Conclusion
PT injury is not uncommon, but is infrequently reported in the literatures. It is the 3rd cause of post traumatic lateral ankle pain, next to capsular and ligamentous injuries. The normal tendons rarely get torn as a result of a single trauma; however, some regional anatomical variants predisposition play an important role in the pathogenesis of degenerative tendinosis and subsequent partial or complete tears of the PT. Early or even simultaneous correction of these variants with the peroneal injuries helps to limit the possible recurrence of these injuries or chronic lateral ankle joint instability.
Conflict of interest
The authors declare that there are no conflict of interest.
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 21 March 2018
References
- D.S.HeckmanS.ReddyD.PedowitzK.L.WapnerS.G.ParekhOperative treatment for peroneal tendon disordersJ Bone Joint Surg Am.902008404418
- P.RosenfeldAcute and chronic peroneal tendon dislocationsFoot Ankle Clin122007643657
- R.SchubertMRI of peroneal tendinopathies resulting from trauma or overuseBr J Radiol86201320110750
- P.KannusL.JozsaHistopathologic changes preceding spontaneous rupture of a tendonJ Bone Joint Surg Am73199115071525
- X.T.WangZ.S.RosenbergM.B.MechlinM.E.SchweitzerNormal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging featuresRadiographics252005587602
- S.JeongY.KimS.KimM.KimPainful Os Peroneum Syndrome presenting as lateral plantar foot painAnn Rehabil Med362012163166
- V.J.SammarcoD.J.CutticaG.J.SammarcoLasso stitch with peroneal retinaculoplasty for repair of fractured os peroneum: a report of two casesClin Orthop Relat Res468201010121017
- http://www.socscistatistics.com/tests/fisher/Default2.aspx.
- J.VegaJ.P.BatistaP.GolanóA.DalmauR.ViladotTendoscopic groove deepening for chronic subluxation of the peroneal tendonsFoot Ankle Int342013832840https://doi.org/10.1177/1071100713483098
- Luijkx Tim, et al. http://radiopaedia.org/articles/calcaneus.
- Y.CheungZ.S.RosenbergT.MageeL.ChinitzNormal anatomy and pathologic conditions of ankle tendons: current imaging techniquesRadiographics121992429444
- Leah M.OchoaRahul.BanerjeeRecurrent hypertrophic peroneal tubercle associated with peroneus brevis tendon tearJ Foot Ankle Surg462007403408
- Celikyay F, Yuksekkaya R, Almus F, Bilgi E. Tenosynovitis of the peroneal tendons associated with a hypertrophic peroneal tubercle: radiography and MRI findings. BMJ Case Rep Published online: http://doi:10.1136/bcr-2013-200204.
- M.SobelM.E.LevyW.H.O.BohneCongenital variations of the peroneus quartus muscle: an anatomic studyFoot Ankle Surg1119908189
- B.MartinelliS.BernobiPeroneus quartus muscle and ankle painFoot Ankle Surg82002223225
- J.MackenzieN.JacobA.StavrosCadaveric case report: clinical implications of novel variants of the fibularis (peroneus) quartus muscle inserting onto the cuboid bone: peroneocuboideus and peroneocalcaneocuboideusFoot Ankle Surg522013118121
- K.DavdaK.MalhotraP.O’DonnellD.SinghN.CullenEFORT Open Rev22017281292
- Y.CheungZ.S.RosenbergMR imaging of the accessory muscles around the ankleMagn Reson Imag Clin N Am92001465473
- R.MirmiranC.SquireD.WassellThe prevalence and role of low lying peroneus brevis muscle belly in patients with peroneal tendon pathologies: a potential source for tendon subluxationJ Foot Ankle Surg542015872875
- T.H.LuiTendoscopic resection of low-lying muscle belly of peroneus brevis or quartusFoot Ankle Int332012912914
- J.J.PetersonL.W.BancroftOs peroneal fracture with associated peroneus longus tendinopathyAJR Am J Roentgenol1772001257258
- T.C.WilsonR.C.WilsonK.G.OuzounovThe symptomatic os vesalianum as an uncommon cause of lateral foot pain: a case reportJ Am Podiatr Med Assoc1012011356359
- B.N.KalantariL.L.SeegerK.MotamediK.ChowAccessory ossicles and sesamoid bones: spectrum of pathology and imaging evaluationAppl Radiol28–372007