Abstract
Background
The success of any tuberculosis (TB) control/intervention programme hinges on the understanding of transmission dynamics of TB within that setting. However, there is paucity of data in high disease burdened countries like Nigeria on the associated risk factors of childhood TB and this supports the need for this research.
Objective
This study was undertaken to determine the prevalent associated risk factors of childhood pulmonary TB in a high diseased burdened setting.
Subjects and method
We carried out a cross sectional study among children aged 18 months to 15 years in six selected health facilities in Nasarawa State, Nigeria. The subjects were screened for pulmonary TB using chest X-ray, sputum or gastric aspirate acid-fast bacilli microscopy and mycobacterium culture. They were also screened for HIV infection. Detailed information was taken regarding history of contact with adult TB source case, house-hold contact, duration of contact, house-hold size, number of people sleeping in a room, cross ventilation, BCG immunization, socio-economic, educational and HIV status of parents, and ingestion of unpasteurized milk and chronic illness other than TB. The subjects had physical examination for BCG scar and nutritional status.
Results
A total of 150 subjects were selected for the study with mean age of 9.12 ± 4.66 years and median age of 10.0 years. The prevalence of definite TB cases found among them was 32% which is 5.5 times higher than the reported national average. The risk factors associated with pulmonary TB include lower socioeconomic status (79.2%), history of contact with an adult TB case source (72.9%), overcrowding (72.9%), absence of cross ventilation (68.8%), ingestion of unpasteurized milk (45.8%) and severe malnutrition among children under five using MUAC parameter (12.5%). The most significant independent predictors of TB in children were absence of cross ventilation (OR = 3.27), contact with adult source case (OR = 2.91) and overcrowding (OR = 2.30).
Conclusion
Absent of cross ventilation, contact with adult source case and overcrowding are the most significant predictors of pulmonary TB in children. Although ingestion of unpasteurized milk is a significant predictor and important source of TB, it is not a major source of TB transmission when compared to contact with adult source case (Open TB).
1 Introduction
The knowledge of the global burden of TB and its associated risk factors in children is limited to a certain extent.Citation1 The risk factors of TB infection is more or less same in both children and adults. However, children bear much of the brunt of the disease because they are easily infected by house-hold contact with infected adults, mostly their caregivers.Citation2 Generally, young children aged 0–4 years are the most vulnerable to the disease due to vulnerability of their immune systems.Citation3 A small proportion of children with TB (generally older children) develop post-primary TB either due to reactivation in the lungs, after a latent period of dormant bacilli acquired from a primary infection, or by re-infection.Citation4 Immuno-suppression, commonly from Human Immunodeficiency Virus (HIV) infection, multiplies the risk of progression to disease in children.Citation1,Citation4,Citation5 Severe malnutrition has a strong association with TB.Citation6 Other risk factors known to be associated with TB infection include poverty, poor immunization status (unvaccinated with BCG), low parental education especially maternal education, overcrowding, high population density, contact with adult infectious TB cases, ingestion of unpasteurized milk, and chronic diseases.Citation4,Citation7–Citation13
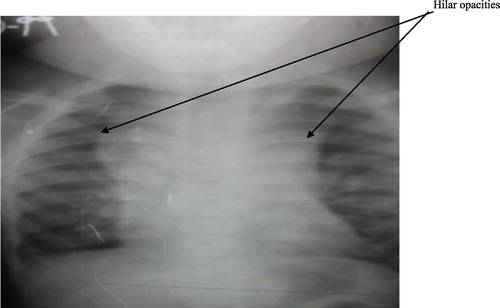
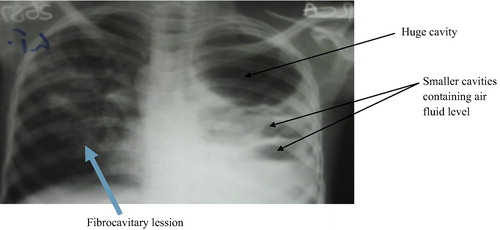
The advent of Human Immunodeficiency Virus (HIV) infection has changed the global trend of TB with number of TB cases rising especially in the developing countries of southeast Asia and sub-Saharan Africa, where co-infection with HIV and TB are prevalent.Citation14 Nigeria continues to record the highest TB incidence in sub-Saharan Africa as a result of the prevalence of the aforementioned risk factors worsen by protracted poverty, recent large pool of internally displaced persons and population migration due to ethno-religious conflicts/insurgency. It is therefore imperative to ascertain the risk factors that are associated with pulmonary TB amongst children in the region who bear huge burden of the disease which is rarely appreciated due to under reporting.Citation5 The study is aimed at finding out the associated risk factors for Pulmonary TB among children aged 18 months to 15 years in an endemic setting (see and ).
2 Materials and methods
This cross sectional descriptive study was carried out in six selected health facilities in Nasarawa State, Nigeria over a period of six months; February to July 2012. One hundred and fifty (150) children were enrolled based on 8.9% smear positive prevalence of TB in children previously reported in Ibadan, Nigeria.Citation15 The study subjects were children between the ages of 18 months to 15 years seen in the selected health facilities both out- and in-patient who have consented and are anti-tuberculosis chemotherapy naive. Multi-stage sampling technique was used to select the health facility and study subjects starting from the local government councils in the three senatorial districts of the state. Ethical approval was obtained from the Human Research Ethics Committee of the Nasarawa State Ministry of Health, and informed written consent was taken from parents of study subjects.
The subjects were screened for pulmonary TB depending on their age using either sputum or gastric aspirate samples for Acid Fast Bacilli (AFB) microscopy by Ziehl-Neelsen method and mycobacterium culture on Egg-based media (Lowenstein-Jensen media). A definite TB case in a child was defined by either culture positive or AFB microscopy positive in two smears or a combination of both culture and AFB Microscopy in accordance with WHO recommendation.Citation16 All the children were also assessed radiologically for pulmonary TB using chest X-ray investigation and screened for HIV using ELISA method according to serial national algorithm for diagnosis of HIV following pre-test counseling (opt-in).
A questionnaire was administered to evaluate the associated risk factors of pulmonary TB and detailed information obtained regarding history of contact with adult TB source case, house-hold contact, duration of contact, house-hold size, number of people sleeping in a room, cross ventilation, BCG immunization, socio-economic, educational and HIV status of parents, ingestion of unpasteurized milk and chronic illness other than TB. The subjects were further examined for BCG scar and nutritional status.
The occupation and education of the parents of study subjects was fundamental in determining their socioeconomic status. Subsequently, classified into socioeconomic class high or upper (class I and II), middle (class III) and lower (IV and V) using the Olusanya et al.Citation17 index scoring method. Household size was determined by the number of family members in the household whereas household overcrowding was considered when an average of greater than two persons sleep in a standard room.Citation14,Citation18–Citation20 For our study contact with adult TB source case was defined as contact in general of a child 15 years or below with an adult with active TB (Open TB) irrespective of the location. House-hold contact was defined as a child 15 years or below living in the same house (dwelling under the same roof) as the adult with active TB (Open TB).
Anthropometric measurements included the weight, height or length, and mid upper arm circumference (MUAC). These were aimed at assessment of the nutritional status of the children. WHO Z-score [weight for age (WAZ) and height for age (HAZ)] was used to identify those who had severe malnutrition (Z score of <-3SD). The weight was measured in kilogram (kg) to the nearest 0.1 kg using Bassinet weighing scale in children less than 24 months and salter bathroom scale for children older than 24 months. Measurements were read twice and the average recorded. The scales were checked for accuracy with a standard 10 Kg weight after every tenth measurement. The height was measured in centimeter to the nearest 0.1 cm using stadiometer, whereas infantometer was used to measure length in children less than 24 months. The MUAC was measured with a non-stretch tape in centimeters to the nearest 0.1 cm in children 18 months to 59 months. Severe acute malnutrition was confirmed using the WHO standard of MUAC less than 11.5 cm.
2.1 Data management/ analysis
All subjects’ data in the questionnaire was entered into computer using microsoft excel and analysed using the SPSS statistical software version 17.0. Categorical variables were cross tabulated using frequencies and percentages, whereas quantitative variables were summarized using mean, standard deviations, median or range as appropriate. Student t-test was used for comparison of means of parametric variables. The chi square test was used for testing the significance of association between categorical variables on contingency tables. Binary logistic regression model was used to obtain predictors of TB in children using the obtained risk factors as independent variables and definite TB case (TB case and No TB) as dependent variable. All tests of significance were two-tailed. P-value < 0.05 was considered statistically significant difference.
3 Results
During the study period, a total of 150 subjects were enrolled with a mean age of 9.12 ± 4.66 years and median age of 10 years. There were 72 males (48%) and 78 females (52%) with male to female ratio of 0.92:1. High proportion (66.7%) of the families of study subjects belonged to the lower socio-economy class with 22.7% and 10.6% belonging to the middle and upper social classes respectively ().
Table 1 Socio-demographic characteristics of the study subjects (n = 150).
Sputum and gastric aspirates samples were collected from 110 and 40 of the study subjects respectively. Out of the sputum and gastric aspirates samples 41 and 7 respectively were diagnosed of definite TB, given a total of 48 (32%) out of the 150 children enrolled having definite TB, which is statistically significant (p = 0.022).
All the 150 study subjects were assessed radiologically for Pulmonary TB using chest X-ray investigation and the result is shown in . Among the 48 definite TB cases, normal radiographic findings were seen in 20 (41.50%), hilar opacities 12 (25.0%) and cavitary lesions 9 (18.8%). Among those without TB, peri-hilar infiltrates and nodular opacities were more common rather than cavitary lesion. These were statistically significant (p = 0.0001).
Table 2 Radiologic findings reported in children with definite TB and children with no TB.
The risk factors associated with pulmonary TB discovered amongst the study subjects include lower socioeconomic status 38(79.2%), history of contact with an adult TB case source 35(72.9%), overcrowding 35(72.9%), absence of ventilation 33(68.8%), ingestion of unpasteurized milk 22(45.8%) and severe malnutrition among children under five using MUAC parameter 6(12.5%) .
Table 3 Risk factors associated with definite TB among cases compared to cases without TB.
Also 14(29.2%) out of the 48 children with definite TB had chronic illnesses other than TB or HIV. These include Nephrotic sydrome on steroid treatment (6), Chronic kidney disease (4), Non-hodgkin lymphoma (2), Diabetes mellitus (1) and sickle cell (1).
Binary logistic regression model using definite TB case (TB case and No TB) as dependent variable and risk factors as independent variables demonstrates that socio-economic status, house hold size, overcrowding, absence of cross ventilation, contact with adult TB case, and ingestion of unpasteurized milk were the significant predictors of tuberculosis among children by Wald criterion (P < 0.05). The significant predictors with highest Expn (OR) are; no cross ventilation (OR = 3.27), contact with adult source case (OR = 2.91) and overcrowding (OR = 2.30) .
Table 4 Binary logistic regression of risk factors predictive of TB in subjects.
4 Discussion
Tuberculosis remains one of the major among the group of common infectious diseases of Children.Citation21 The TB prevalence (32%) in this study when compared with the reported 2013 Nigeria's national prevalence rate of 5.8% among children is 5.5 times higher.Citation22 This indicates how highly endemic TB is in this setting. It is therefore of prime importance to have knowledge on the associated risk factors for pulmonary TB among these infected children as they represent a large pool from which more TB cases are likely to arise in future.Citation21
Chest radiography plays a significant role in the diagnosis of childhood tuberculosis.Citation23–Citation25 In our study, we found hilar opacities and cavities to be the commonest pathologic chest radiographic findings among the children diagnosed of pulmonary TB which is consistent with similar studiesCitation24,Citation26 from South Africa. Possible explanation for these findings is based on the natural history of TB disease. Hilar opacities demonstrate the involvement and exuberant response of regional lymph nodes following primary infection majorly among the young age group in order to stop the multiplication of Mycobacterium tuberculosis at this stage. Therefore, hilar opacities are considered as the radiologic hallmark of primary TB.Citation3 Cavities are adult type disease which first appears around 8–10 years of age and becomes the predominant disease manifestation during adolescence.Citation27 This points to the fact that matured immune system in TB diseased patient plays a significant role in formation of cavities. Also, the finding of normal chest radiographs in some of our study subjects with definite TB is consistent with the studiesCitation24,Citation26 from South Africa. The reason being that they were immunocompromised (HIV infected and severely malnutrition).
The majority of the cases of definite TB in this study were amongst the 10–15 year olds (58.3%). This finding was unexpected as studies from other high endemic TB communities tended to have cases of TB in younger children. Rie et al. from South Africa in a community based study reported 25–49% of their study subjects with TB were between 0 and 4 years while 7–12% cases were of 5–14 years.Citation28 Another community based study from South Africa by Marais et al.Citation29 reported the highest risk of TB disease to be very young age (<2 years) and lowest risk was between 3 and 10 years but risk increased again above 10 years of age. Unlike the South African studies above, the current study is facility based and may not be representative of disease distribution by age in the community. The isolation of AFB or Mycobacterium tuberculosis in sputum by smear or culture is easier in adolescents who have open pulmonary TB and constitute 53.4% of the study subjects as compared to younger age groups.
TB affects mostly the poor.Citation4 This study shows that more than two-third of definite TB cases were from the low socio-economic group. This is in consonance with the work done by Aarti et al.Citation30 in India. The poor are more vulnerable to TB because they are more likely to have poor housing that are poorly ventilated and overcrowded.Citation19 Also associated with poverty and crowded shelters are commercial sex work, child abuse and neglect, malnutrition and poor immunization coverage, all documented risks for TB and HIV infections.Citation31–Citation33
Overcrowding as reflected by housing density has the potential to increase exposure of susceptible individuals to those with open TB, so that children sleeping in the same room as the index patient are more likely to get infected.Citation18 In our study we used the number of persons per room as a measure of overcrowding and found that it was a significant risk factor associated with pulmonary TB in children. This finding is consistent with the study from Bangkok.Citation18
Lack of cross ventilation and overcrowding were amongst the most significant independent predictors of TB in children seen in our study with high odds ratio Exp (B) 3.27 and 2.30 respectively. These factors are known to be associated with continuous spread of Mycobacterium tuberculosis as observed in communities with high rate of active TB because their presence multiply the risk for TB infection as shown in our study.Citation4,Citation18,Citation20,Citation28,Citation34,Citation35
Children are three times more likely to develop TB when exposed to an adult with open TB based on our study. This is consistent with findings of similar studies from Bangkok, Gambia, Pakistan, Bangladesh, Benin City and New York City.Citation18,Citation19,Citation21,Citation23,Citation36,Citation37 Our study also established that greater than half the population of children with definite TB has had contact history of more than two years with adult TB patients. This indicates that intensity of exposure to adult with TB for a prolonged period predisposes a child to developing TB.Citation18,Citation21,Citation35
Similarly, a high proportion (70.8%) of definite TB cases has a history of BCG vaccination compared to 29.2% with no such history. This differs from what Guwatudde et al.Citation14 and Boccia et al.Citation33 recorded in Uganda and Zambia respectively; where they found a strong association between non-BCG vaccination and TB infection. Our study findings can be explained by the fact that BCG vaccination does not protect from TB but may prevent severe forms of TB especially in infancy and early childhood, limiting serious disseminated TB.Citation21
Also, about half of the definite TB cases (45.8%) in this study had absent BCG scar but this was not statistically significant. Often BCG scars are considered as the marker of vaccination, however its limitations span from fading scar, immunosuppressive conditions, inappropriate immune response, lack of immunization, poor record keeping of vaccinations given and faulty technique amongst others.Citation1,Citation14,Citation19 The finding of absent BCG scar as a non-risk factor for TB in this study is consistent with given records of studies from Uganda and Zambia.Citation14,Citation33
Maternal education correlated well with definite TB cases in our study. While 50% of children with definite TB had mothers with no formal education, only 6.3% of children so infected had mothers with tertiary education. This is consistent with similar studies from around the world which shows that maternal education is integral to protecting a child against pulmonary tuberculosis.Citation19,Citation21,Citation23,Citation28 Maternal education aids female empowerment which impacts positively on child nutrition and well-being.
The association between ingestion of unpasteurized milk and TB was also statistically significant. About half the subjects with definite TB had a history of ingestion of unpasteurized milk. This is similar to the reported study by Cohn et al.Citation13 from the Dominican Republic Bateyes which shows unpasteurized milk consumption as an independent risk factor for intrathoracic TB among children aged 18 months to 18 years. Similarly, Yohanna et al.Citation38 reported the high risk for contracting zoonotic infection by the Nasarawa state populace from high prevalence (15.08%) of bovine TB found among the Fulani herdsmen in the State. The high prevalence of TB in Nasarawa State observed in the study may be due to Mycobacterium bovis; or the combination of M.bovis and M.tuberculosis rather than just M.tuberculosis infection.
On another hand, there is no statistically significant association between HIV status of either study subjects or of their parents / guardians as risk factors for TB in this study. These findings agree with the report of Nelson et al.Citation4 in Global Epidemiology of Childhood TB which indicates that several studies worldwide have failed to find an increased rate of TB in HIV-exposed or infected children. A study from Zambia also shows that the presence of multiple pathogens in a single HIV infected child was common and TB ranked fourth in order of occurrence of the pathogens.Citation39 This finding supports the fact that young children with HIV are at higher risk of morbidity and mortality from other respiratory diseases, and may succumb to these infections before being infected with TB.Citation4
A considerable number of children with chronic illnesses that are non-communicable has been noted in this study to have PTB which is comparable to the study of Shetty et al.Citation20, although the finding was not statistically significant. The leading ones found are the renal diseases (Nephrotic syndrome on steroid treatment, chronic kidney disease) followed by non-hodgkin lymphoma, sickle cell anaemia and diabetes mellitus. These illnesses are a reflection of recent major demographic and lifestyle changes in urban setting of sub-Saharan Africa, leading to rise in non-communicable diseases.Citation40 These illnesses are known immunosuppressive conditions that are associated with reactivation of latent tuberculosis.Citation40
This study also demonstrates association between malnutrition and TB as seen in other related studies from India and Pakistan.Citation11,Citation21 Severe acute malnutrition using mid upper arm circumference (MUAC) <11.5 cm amongst the under-fives was found to be statistically significant (p = 0.002). However, the Z-scores for height and weight for age are of no statistical significance (p = 0.735 and p = 0.533 respectively). The reason may be the small sample size employed for this study.
Future research questions
There is a need for a community based study to compare findings with this hospital based study. A molecular diagnosis with genomic characterization of the isolated mycobacterium species is required to determine the type of mycobacterium infection in the community.
Conclusion
Absent cross ventilation, contact with adult source case and overcrowding are the most significant predictors of pulmonary TB in children. Although ingestion of unpasteurized milk is a significant predictor and an important source of TB, it is not the major source of TB transmission when compared to contact with adult source case (Open TB).
Recommendations
Intensive advocacy towards good housing, contact tracing and, public education on the dangers of ingestion of unpasteurized cow milk are vital efforts in TB elimination among children.
Conflict of interest
The authors declared that there is no conflict of interest
Notes
Peer review under responsibility of Alexandria University Faculty of Medicine.
Available online 14 June 2018
References
- F.KristinaS.LisaTuberculosis in childrenClin Chest Med262005295312
- K.OsinusiTuberculosis in childrenJ.C.AzubuikeK.E.O.NkanginiemePaediatrics and child health in a tropical region, 2nd ed.2007African Educational Services, owerriNigeria634643
- B.J.MaraisR.P.GieH.S.SchaafN.BeyersP.R.DonaldJ.R.StarkeChildhood pulmonary tuberculosis: old wisdom and new challengesAm J Respir Crit Care Med173200610781090
- L.J.NelsonC.D.WellsGlobal epidemiology of childhood tuberculosisInt J Tuberc Lung Dis82003636647
- B.J.MaraisS.M.GrahamM.F.CottonN.BeyersDiagnostic and management challenges for childhood tuberculosis in the era of HIVJ Infect Dis1962007576585
- S.QaziS.KhanM.A.KhanEpidemiology of childhood tuberculosis in a hospital settingJ Pak Med Assoc4819989093
- T.AhmedF.SobhanA.A.M.ShamsirChildhood tuberculosis: a review of epidemiology, diagnosis and managementJ inf Dis Pak1720085260
- T.D.BrockRobert koch: a life in medicine and bacteriology1999ASM Press http://en.wikipedia.org/wiki/Special:Booksources/0910239193 [accessed August, 2010]
- L.MbalaM.MashakoM.KashongweChildhood tuberculosis in a rural tropical areaTrop Doct322002119120
- G.Q.KhanM.S.ChannarM.A.MannanTuberculosis in BCG vaccinated and non-vaccinated under 15years of agePak Ped J272003114116
- V.K.ChadhaA.BanerjeeM.IbrahimP.S.JaganathaP.KumarAnnual risk of tuberculosis infection in Zkhammam a tribe district of Andhra PradeshJ Commun Dis352003198205
- Y.MukadiS.WiktorI.CoulibalyD.CoulibalyA.MbengueA.FolquetImpact of HIV infection on the development, clinical presentation and outcome of tuberculosis among children in Abidjan, Cote d'IvoireAIDS11199711511158
- K.A.CohnR.FinalleG.O’HareJ.M.FerisJ.FernandezS.SamirRisk factors for intrathoracic tuberculosis in children from economic migrants population of two Dominican Republic BateyesPediatr Infect Dis J282009782786
- D.GuwatuddeS.ZalwangoM.R.KamyaBurden of tuberculosis in Kampala, UgandaBull World Health Organ812003799805
- A.O.KehindeR.E.OladokunO.M.IgeR.A.BakareK.OsinusiBacteriology of childhood tuberculosis in Ibadan, Nigeria: a five-year reviewTrop Med Health362008127130
- WHOGuidelines for HIV surveillance among tuberculosis patients, 2nd ed.2004WHO document WHO/HTM/TB/2004.339
- O.OlusanyaE.OkpereM.EzimokhaiThe importance of social classs in voluntary fertility control in a developing countryW Afr J Med41985205211
- T.SongpolK.JaranitF.WijitrS.UdomsakA.PasakornS.PramuanRisk factors for tuberculosis infection among household contact in Bangkok, ThailandSouth East Asian J Trop Med Public Health352004375383
- C.LienhardtK.FieldingJ.S.SillahRisk factors for tuberculosis infection in Children in contact with infectious tuberculosis cases in Gambia, West AfricaPaediatrics1112003 e608-14
- N.ShettyM.ShemkoM.VazG.D’SauzaAn epidemiological evaluation of risk factors for tuberculosis in South India: A matched case-control studyInt J Tuberc L Dis1020068086
- U.H.SamiH.MaqboolK.JaiA.SaleemRisk factors of tuberculosis in childrenAnn Pak Inst Med Sci620105054
- WHOGlobal tuberculosis control report 20132013World Health OrganizationGeneva
- R.K.MohamedA.R.MohamedA.M.ShaikhA.A.MohamedA.ShahnazRisk factors of childhood tuberculosis: a case control study from rural BangladeshWHO South-East Asia J Public Health120127684
- H.S.SchaafN.BeyersR.P.GieRespiratory tuberculosis in childhood: the diagnostic value of clinical features and special investigationsPediatr Infect Dis J141995189194
- B.J.MaraisP.MadhukarRecent advances in the diagnosis of childhood tuberculosisArch Dis Child922007446452
- H.S.SchaafB.J.MaraisA.WhitelawCulture – confirmed childhood tuberculosis in Cape Town, South Africa: A review of 596 casesBMC Infect Dis72007140
- M.P.CarlosB.J.MaraisCurrent concepts of tuberculosis in childrenN Engl J Med3672012348361
- A.V.RieN.BeyersR.P.GieM.KunnekeL.ZietsmanP.R.DonaldChildhood tuberculosis in an urban population in South Africa: Burden and risk factorsArch Dis Child801999433437
- B.J.MaraisR.P.GieH.S.SchaafA.C.HesselingC.C.ObiharaJ.R.StarkThe natural history of childhood intrathoracic tuberculosis- a critical review of the pre-chemotherapy literatureInt J Tuberc L Dis82004392402
- K.AartiR.AnjaliSocial Status makes a difference: Tuberculosis Scenario during National Family Health SurveyIndian J Tuberc5420071723
- J.G.LaahE.AyiwuluSocio-Demographic characteristics of patients diagnosed with HIV/AIDS in Nasarawa EggonAsian J Med Sci22010114120
- National Population Commission and ICF MacroNigeria Demographic and Health Survey 2008 Fact Sheet: North Central2009AbujaNigeria
- D.BocciaJ.HargreavesP.L.De StavolaThe association between Household Socioeconomic position and prevalent Tuberculosis in Zambia: A case-control studyPLoS ONE62011e20824
- J.HorsburghTuberculosis without tuberclesTuberc Lung Dis771996197198
- R.RileyTransmission and environmental control of tuberculosisL.ReichmanE.HershfieldTuberculosis1993Marcel DeckkerNew York
- M.O.IbadinO.OviaweTrend of childhood tuberculosis in Benin City, NigeriaAnn Trop Paediatric212001141145
- L.SaimanP.S.GabrielJ.SchulteM.P.VargasT.KenyonI.OnoratoRisk factors for latent tuberculosis infection among children in New York CityPediatrics10720019991003
- C.A.YohannaI.F.IjaboneS.I.B.CadmusPrevalence of bovine tuberculosis using single comparative intradermal tuberculin test (SCITT) in Fulani herds in Nasarawa state, north central NigeriaSokoto J Vet Sci720084648
- C.ChinduV.MudendaS.LucasLung diseases at necropsy in African children dying from respiratory illnesses: a descriptive necropsy studyLancet3602002985990
- B.J.MaraisK.LönnrothS.D.LawnTuberculosis comorbidity with communicable and non-communicable diseases: integrating health services and control effortsLancet Infect Dis132013436448