Abstract
Purpose: Currently there is an increase in the incidental diagnosis of renal cell carcinoma (RCC). Our aim was to assess the survival of patients with incidental and symptomatic renal tumours who had undergone nephrectomy.
Patients and methods: We retrospectively assessed 604 patients who underwent renal surgery for RCC between 1983 and 2005. Patients were divided in two groups; group 1 had incidental and group 2 had symptomatic tumours. The median follow-up was 4 and 3.3 years for groups 1 and 2, respectively. All patients had surgery in the form of radical or partial nephrectomy. Sex, age, tumour size, type of surgery, pathological characteristics and patient survival in both groups were evaluated. The statistical analysis included the log-rank, Kaplan–Meier and Cox regression tests.
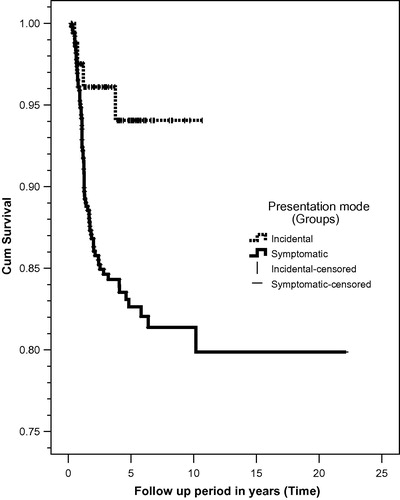
Results: There were 85 patients (14%) in group 1 (mean age 49.6 years) and 519 (86%) in group 2 (mean age 50 years). The mean (SEM, range) tumour size was 7.4 (0.4, 1.5–20) cm in group 1 and 9.7 (0.2, 2–38) cm in group 2 (P <0.001). The most common stage was T1 (52%) and T2 (44%) in groups 1 and 2, respectively, with a predominance of G2 grade and the conventional type histology in both the groups. There was a significant difference in cancer-specific survival (CSS) between the groups (log-rank, P = 0.017). The 5– and 10–year CSS was 94% and 94% for group 1, and 82.5% and 79.5% for group 2. Cox regression analysis showed that in group 1, only the tumour mid-zonal location (P = 0.093), tumour stage pT (P <0.001), grade 1 (P = 0.03), grade 2 (P = 0.01), grade 4 (P =0.01) and the papillary histological type (P =0.019) had significant effects on CSS. In group 2, only tumour size (P = 0.022) and stage pN (P = 0.003) had significant effects on CSS. The tumour recurrence rate was 18% and 29% for groups 1 and 2, respectively.
Conclusions: This large study supports the findings of other smaller studies published previously, confirming that at presentation incidental renal tumours are smaller and their diagnosis provides a better prognosis and longer CSS.
Keywords:
Abbreviation:
Introduction
The incidence of RCC and the diagnosis of localised tumours are both increasing [Citation1]. The 5-year survival rate for symptomatic tumours is 30–83%, while for incidental tumours it is 83–95% [Citation2]. In the current era of increased frequency and sophistication of radiological imaging, the rate of incidental findings of renal cortical tumours has steadily increased. As a result, the apparent incidence of RCC is increasing, as is the trend towards diagnosis at an earlier stage. The greatest incidence of asymptomatic small renal masses occurs in patients aged >70 years [Citation3], in whom multiple comorbidities can increase the risks of surgery [Citation4]. Incidentally diagnosed tumours have been linked to better survival, because the tumours are at an earlier stage than for symptomatic RCC. However, investigators have disagreed about the implications of these incidentally detected tumours on survival and mortality [Citation5,Citation6], because of possible stage migration and lead-time bias (the apparent increased survival time resulting from an earlier, more timely, diagnosis). Although some studies have identified incidental diagnosis as a significant independent positive prognostic factor for death from RCC, as these tumours are less aggressive biologically [Citation7,Citation8], others have shown that incidental detection was not an independent prognostic factor for death, indicating that these tumours are of a similar biological nature to symptomatic RCCs, only diagnosed earlier [Citation9]. The aim of the present study was to assess the survival of patients with incidental (group 1) and symptomatic (group 2) renal tumours who had undergone nephrectomy.
Patients and methods
We retrospectively collected data from 829 patients who had renal surgery for RCC between 1983 and 2005 in the Mansoura Urology and Nephrology Center, Egypt. There were 604 patients included in the study, after excluding 225 (either missed follow-up or with metastasis at presentation). The patients were divided into groups 1 and 2 according to the diagnosis of the primary tumour; in group 1, patients were diagnosed with a renal lesion during radiological examination because of complaints unrelated to RCC, and in group 2 they presented with symptoms related to RCC. The radiological investigations used were ultrasonography, excretory urography, CT and MRI. The patients were followed up for periods of 0.2–22 years, with a median of 4 years in group 1 and 3.3 years in group 2. The endpoint of follow-up was either death or December 2008. The 2002 TNM classification, Fuhrman’s classification and WHO histological classification were used for the stage, grade and histological types of RCC, respectively. The cancer-specific survival (CSS) was calculated using Kaplan–Meier curves, and the log-rank test was used to compare differences in the survival of both groups. Cox regression analysis was used to evaluate the effects of different factors on the survival. Hazard ratios are presented, with their 95% CI. The chi-squared test was used to test associations between the groups. The statistical significance level was set at P < 0.05.
Results
In all, 604 patients were assessed, 85 (14%) in group 1 and 519 (86%) in group 2. The patient and pathological characteristics of both groups are presented in . The patients’ age and sex were comparable in both groups. The male-to-female ratios were, respectively, 2:1 in group 1 and 1.5:1 in group 2. There was a significant difference in tumour size between the groups (P < 0.001; ). There was no preference for the right or left kidney in both groups (P = 0.193). The most common tumour location was the upper pole, followed by the lower pole of the kidney, at 34% and 24.7% in group 1, and 25% and 23% in group 2, respectively.
Table 1 Patient and tumour characteristics for the two groups.
The tumour stage (P = 0.001) and grade (P = 0.001) had significant associations with patient presentation in both groups. In group 1, T1 (52%) was the most common stage and in group 2, T2 (44%) was the most common stage. More patients in group 2 had nodal involvement (8%) than in group 1 (3.6%). The histological grade G2 predominated in both groups, at 55.6% and 52%, respectively. The most common histological tumour type in group 1 was conventional (53%), followed by chromophobe (30.5%), and in group 2 was also conventional (44.5%) followed by chromophobe (29%).
There was a significant difference in CSS between the groups (log-rank, P = 0.017). The 5- and 10-year CSS was 94% and 94% for group 1, and 82.5% and 79.5% for group 2 (). Cox regression analysis was used to evaluate the effects of tumour location, size, stage, grade and histology on CSS in both groups. In group 2, only the tumour mid-zonal location (P = 0.039); tumour stage pT (P < 0.001); grade 1 (P = 0.03); grade 2 (P = 0.01); grade 4 (P = 0.01) and the papillary histological type (P = 0.019) had significant effects on CSS (). In group 1, only tumour size (P = 0.022) and stage pN (P = 0.003) had significant effects on CSS (). The tumour recurrence rate was 18% and 29% for groups 1 and 2, respectively. Local and distant recurrence was 4% and 28% for group 1, and 4.6% and 33% for group 2. In group 1, 50% of the recurrences occurred in the first year and in group 2, 86% occurred in the first year. Five (5.8%) patients died in group 1 and 107 (20.6%) died in group 2.
Table 2 Cox multivariate regression analysis of the two groups.
Discussion
The present large study of incidental renal tumours show that they present when smaller and that their diagnosis offers a better prognosis and longer CSS than for symptomatic patients with RCC; these findings support smaller studies reported previously [Citation10,Citation11]. The 5-year CSS of 94% for group 1 and 82.5% for group 2 in the present study are comparable with the 5-year survival rate of 83–95% for incidental tumours and 30–83% for symptomatic renal tumours reported previously [Citation2]. The diagnosis of incidental renal tumours was reported by Dall’Oglio [Citation10] to have a better prognosis and longer disease-free survival. In their study of 115 patients, Dall’Oglio [Citation10] found that 59 (51%) patients had an incidental diagnosis and 56 (49%) were symptomatic. In the incidental group only one patient had tumour progression and there were no deaths, while in the symptomatic group there were five progressions and 10 deaths. The 5-year CSS was 100% in the incidental and 80% in the symptomatic group (P = 0.001), while the disease-free rate was 98% in the incidental and 62% in the symptomatic group (P < 0.001). Kawata et al. [Citation11], in a study of 252 patients who were divided according to presentation into three groups defined as S1 (incidental tumour), S2 (localised symptoms) and S3 (systemic symptoms), found that the 5-year CSS rates were 93.1%, 71.0% and 20.2% for S1 (144 patients), S2 (80 patients) and S3 (28 patients), respectively (P < 0.001).
The real survival benefit of an incidental diagnosis of RCC has been debated [Citation5,Citation3]. This is because of possible ‘lead-time’ bias and ‘stage migration’, with tumours discovered earlier being less invasive and of a lower malignant potential, and therefore leading to better survival. In the present study the most common stage was T1 in group 1 and T2 in group 2. In a Swedish study, RCC was present in 2.1% of autopsies, but the malignancy was only detected before death in a third of these cases, with 80% of patients dying with, but not from, their RCC [Citation12]. This finding supports the idea that tumours detected incidentally might be of a biologically different nature than symptomatic RCC. On the other hand, it was reported that incidental detection was not an independent prognostic factor for death, indicating that these tumours are of a similar biological nature as symptomatic RCCs, only diagnosed earlier [Citation9]. However, the incidentally diagnosed tumours were 2.3 cm smaller on average and at a lower stage and grade than symptomatic tumours, with significantly better patient survival than those with symptomatic tumours, on univariate analysis (76% vs. 44% 5-year disease-specific survival) [Citation9].
Several authors suggested a potential survival advantage for those in whom RCC was detected early [Citation13]. Indeed, it was noted that the median 5-year survival rate is higher among patients whose renal lesions are discovered incidentally than among those who are present with symptoms [Citation14]. Thus there is an argument to be made for RCC screening based on the prognosis and survival of patients with incidental RCC. However, it has been argued that the improvements in survival for incidentally detected RCC compared to symptomatically detected RCC are attributable to lead-time bias [Citation15], thus one would expect a decreased mortality from kidney cancer with early detection and intervention of RCC; however, it was reported that the kidney cancer mortality rate has increased [Citation1]. Currently, the screening of high-risk populations, especially for those undergoing dialysis or with von Hippel–Lindau disease, and for those aged >50 years, is advised [Citation16]. However, other groups reject this approach in the belief that the cost/benefit relationship of such screening is not well defined [Citation17], although rapid routine examination of the kidneys during ultrasonography of other organs is also defended [Citation17].
In conclusion, currently there are many reports on the treatment of incidentally discovered renal tumours, and minimally invasive techniques are preferable, especially in the elderly who are unfit for surgery; this suggests that more studies are needed to fully understand the behaviour of incidentally discovered tumours and the best methods for their treatment. Incidental renal tumours are smaller at presentation and their diagnosis offers a better prognosis and longer CSS. The only factors that have significant effects on CSS in the symptomatic group are tumour stage, grade, histological type and tumour location, whereas in the incidental group only tumour size and nodal stage have effects on survival.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- W.H.ChowS.S.DevesaJ.L.WarrenJ.F.FraumeniJrRising incidence of renal cell cancer in the United StatesJama28199916281631
- K.H.TsuiO.ShvartsR.B.SmithR.FiglinJ.B.de KernionA.BelldegrunRenal cell carcinoma: prognostic significance of incidentally detected tumorsJ Urol1632000426430
- E.KoubaA.SmithD.McrackanE.M.WallenR.S.PruthiWatchful waiting for solid renal masses. Insight into the natural history and results of delayed interventionJ Urol1772007466470
- D.A.KunkleB.L.EglestonR.G.UzzoExcise, ablate or observe: the small renal mass dilemma – A meta-analysis and reviewJ Urol179200812271233
- R.A.MevorachA.J.SegalM.E.TersegnoI.N.FrankRenal cell carcinoma: incidental diagnosis and natural history: review of 235 casesUrology391992519522
- T.GudbjartssonG.V.EinarssonJ.MagnussonA population-based analysis of survival and incidental diagnosing of renal cell carcinoma patients in Iceland, 1971–90Scand J Urol Nephrol301996451455
- D.BretheauE.LechevallierC.EghazarianV.GrisoniC.CoulangePrognostic significance of incidental renal cell carcinomaEur Urol271995319323
- J.J.PatardA.RodriguezN.Rioux-LeclercqF.GuilleB.LobelPrognostic significance of the mode of detection in renal tumoursBJU Int902002358363
- T.GudbjartssonA.ThoroddsenV.PetursdottirS.HardarsonJ.MagnussonG.V.EinarssonEffect of incidental detection for survival of patients with renal cell carcinoma: results of population-based study of 701 patientsUrology66200511861191
- M.F.Dall’OglioIncidental and symptomatic renal tumors: impact on patient survivalSao Paulo Med J1202002165169
- N.KawataY.NaganeK.YamaguchiT.IchinoseH.HirakataS.TakahashiHow do symptoms have an impact on the prognosis of renal cell carcinoma?Int J Urol152008299303
- S.HellstenJ.JohnsenT.BergeF.LinellClinically unrecognized renal cell carcinoma. Diagnostic and pathological aspectsEur Urol18Suppl. 2199023
- I.M.ThompsonM.PeekImprovement in survival of patients with renal cell carcinoma–the role of the serendipitously detected tumorJ Urol1401988487490
- A.J.PantuckA.ZismanM.K.RauchA.BelldegrunIncidental renal tumorsUrology562000190196
- J.K.ParsonsM.S.SchoenbergH.B.CarterIncidental renal tumors: casting doubt on the efficacy of early interventionUrology57200110131015
- M.JaysonH.SandersIncreased incidence of serendipitously discovered renal cell carcinomaUrology511998203205
- Y.AsoY.HommaA survey on incidental renal cell carcinoma in JapanJ Urol1471992340343