Abstract
Objective: To evaluate the effect of magnified bilateral varicocele ligation on the semen quality and natural paternity rate in subfertile men, based on the sum of varicocele grading.
Patients and methods: In a prospective longitudinal study, 78 patients (mean age 36.5 years, range 21–56) with a total of 156 varicoceles underwent bilateral varicocele ligation. Patients included had bilateral, primary and clinically palpable varicoceles, with a normal hormonal profile and abnormal semen; patients excluded had unilateral varicocele, or were recurrent cases, had infraclinical varicocele or had a genetic abnormality. Patients were classified into five groups (A–E), based on the findings of a physical examination; A included 13 patients with grade sum II (I + I), B included 21 with grade sum III (II + I), C included 25 with grade sum IV (II + II) or (III + I), D included 11 with grade sum V (III + II) and E included eight with grade sum VI (III + III). The follow-up was scheduled at 3, 6 and 12 months to assess semen variables and the natural paternity rate; 16 patients continued to a 36-month follow-up. Data were analysed statistically using a paired t-test to compare the mean sperm variables before and after surgery, with P<0.05 considered to indicate significant differences.
Results: Of the 78 patients, 74 completed the follow-up at 3 months and only seven missed the 6-month follow-up. Overall, the mean sperm density, total sperm motility and sperm morphology increased from 13.44 to 26.48 · 106/mL, 27.4% to 53% and 41.4% to 65.0%, respectively; the differences were statistically significant for all variables (P < 0.001). For each group separately there were significant improvements for both sperm density and motility, but for sperm morphology there were significant improvements in all groups except E, where the improvement was not correlated with those in the other groups. The paternity rate (by natural pregnancy) at 2 years was 26.9%, and this increased to 41% within 3 years.
Conclusion: Magnified bilateral varicocele ligation based on the sum of varicocele grading significantly improved semen quality and the natural paternity rate in subfertile men.
Abbreviation:
Introduction
In 2009 Cayan et al. [Citation1] reported that varicocele (dilated testicular veins) is the most common contributing factor to male infertility, and that varicocele ligation for a clinically palpable varicocele has a confirmed positive effect on the fertility and pregnancy rate. In 1970 Dubin and Amelar [Citation2] confirmed that varicocele in infertile men is associated with bilateral spermatogenic abnormalities and Leydig cell dysfunction. The histopathology of the testis in men with infertility due to a male factor is variable, but most studies reported reduced spermatogenesis (hypospermatogenesis).
In 2002 Lue et al. [Citation3] ascribed the increase in germ cell apoptosis to hyperthermia and a decreased level of total serum testosterone within the testicle. The level of serum testosterone is lower in patients aged >30 years than in younger men with varicocele, a trend which is not seen in men without varicocele, and suggests a progressive adverse effect of varicocele on Leydig cell function [Citation4]. Varicocele ligation is the most common operation for male infertility. It is reported that 35–40% of infertile men have clinically palpable varicoceles. In 1998 Matthews and Goldstein reported a 15% incidence of varicoceles in the general male population [Citation5].
In 1995 Goldstein et al. [Citation6] reported that ≈75% of patients with varicoceles were capable of paternity despite varicoceles being associated with impaired male fertility. Gorelick and Goldstein showed that the relationship between male infertility and varicoceles has not been conclusively established [Citation7]. In the same year Steckel et al. [Citation8] showed that the postoperative effect of varicocele ligation on male fertility was controversial. In a large series of patients with varicoceles, ligation (either unilateral or bilateral) leads to significant improvements in semen quality but it also improved the hormonal function of Leydig cells.
In recent years there have been many novel procedures for varicocele ligation, including microscopic subinguinal (either unilateral and/or bilateral), percutaneous with radiographic embolisation of the internal spermatic vein, and laparoscopic with an artery- and lymphatic-sparing technique [Citation9]. Steckel et al. [Citation10] reported that the grade of the varicocele might have a significant effect on the outcome of varicocele ligation, in that patients with a large varicocele (high grade) have a greater improvement in semen quality after surgery than those with a small varicocele (low grade). However, patients with a smaller varicocele usually have more normal baseline semen values, and therefore the postoperative changes are less significant. Ghanem et al. [Citation11] reported the advantages of the microsurgical subinguinal technique, as there was a very low incidence of recurrence and a lower postoperative complication rate than with non-microsurgical techniques. The microscopic subinguinal varicocele ligation is also associated with less operative and postoperative pain than inguinal approaches. However, this technique is more challenging because of the difficulty in dealing with the large and increased numbers of small arteries and minute veins in the cord at this anatomical site [Citation14]. The most common postoperative complications after varicocele ligation are secondary vaginal hydrocele (lymphoceles) and recurrence of varicoceles secondary to missed ligation of one or more of the three groups of veins comprising the varicocele.
Currently, testicular artery ligation using high-quality operating microscopes, magnification loupes and fine microsurgical instruments allows adequate artery- and lymphatic-sparing techniques, with reliable identification of the three groups of veins that contribute to varicocele formation, and the venous collaterals, together with easier identification of vessel groups. The use of intraoperative duplex ultrasonography (US) and of intraoperative vasoactive agents has facilitated the identification of the testicular artery or arteries, so that the incidence of these complications can be reduced significantly. In addition, men with larger varicoceles have poorer preoperative semen quality, but the repair of large varicoceles results in a greater improvement (128% increase in motile sperm) than the repair of small varicoceles (27% increase in motile sperm) [Citation12].
Thus the aim of the present study was to evaluate the effect of magnified bilateral varicocele ligation on the semen quality and natural paternity rate in subfertile men, based on the sum of varicocele grading.
Patients and methods
Seventy-eight patients presented with infertility and bilateral clinically palpable varicoceles; they underwent bilateral subinguinal microscopic varicocele ligation at the author’s institution between August 2007 and October 2010. The mean (range) age of the patients was 36.5 (21–56) years. Patients included in the study had bilateral clinically palpable primary varicoceles, a normal hormonal profile in those presenting with severe oligospermia of <5 million/mL (FSH, LH and total serum testosterone levels) and abnormal semen values in at least two semen analyses in two different laboratory tests. Patients excluded had unilateral varicoceles, previous surgery, secondary varicoceles, those with a genetic abnormality, infraclinical varicoceles (diagnosed by Doppler US) and those who did not provide two postoperative semen analyses at 3 and 6 months after surgery. Finally, we excluded all patients in whom the primary aim of surgery was for lesions associated with the pathology of the varicocele. All patients with varicoceles were consented and operated for primary or secondary infertility. The main outcome measures were sperm concentration, total sperm motility and sperm morphology. The follow-up for office evaluation was scheduled at 3, 6 and 12 months after surgery, and some patients had 36 months of follow-up to report any paternity by natural pregnancy. The assessment also included the total surgical time, mean duration of hospital stay and any significant postoperative complications reported either by patients themselves or detected during the follow-up. The spontaneous (natural) pregnancy rate over at least a year of follow-up was also ascertained. The mean (range) follow-up was 12 (6–36) months. All patients in this prospective study had a complete history taken to determine the duration and type of infertility (either primary or secondary) and grade of varicocele on physical examination both while supine and standing; the testicular volume before and after surgery and/or biopsies were not assessed.
We classified patients on the basis of the findings of the physical examination (grade of varicoceles). Patients were classified into five groups (A–E), with a grade sum as left + right; A included 13 with bilateral grade I (I + I), B included 21 with II + I, C included 25 with grade sum IV (II + II or III + I), D included 11 with grade sum V (III + II), and E included eight with grade sum VI (III + III).
Of the 78 patients, 28 presented with primary infertility and 50 with secondary infertility of variable duration. Ten patients had primary infertility of 14 months’ duration, 23 of 24 months, 15 of 36 months and remainder had infertility for >60 months.
Surgical procedure
An oblique skin incision was made distal to the external inguinal ring, and the scrotum invaginated using an index finger into the external ring. The incision was enlarged to 3 cm on the index finger of the left hand with the proximal extension of incision at the tip of the index finger which was used to lift the ring slightly above and lateral. The incision was deepened through Camper’s and Scarpa’s fasciae and the spermatic cord was then grasped with a Babcock clamp, delivered and placed over a vessel loop or sometimes a large Penrose drain. The ring was not opened but was supported on two small arterial clamps to visualise the floor of the canal. All layers covering the cord were opened, the internal and external spermatic fasciae were incised and the cord structures were examined using a ×3 magnification loupe. The first step was to identify and isolate both gonadal and vasal arteries, and to separate them from the rest of the cord under direct vision. Both the vas and vasal vein were identified easily, sometimes using an intraoperative duplex US with a 7-Hz probe (grey scale) and/or application of local papaverine on the spermatic cord if there was difficulty in identifying the gonadal artery, or when there was more than one artery, and where there was absence of arterial pulsation. All lymph vessels in the cord were separated and preserved during the whole operation. The dilated veins were ligated using a 3/0 silk suture. After isolation and ligation of all dilated veins within the cord, the floor of the canal was examined on both sides of the cord (lateral and medial). The testicle was delivered out of the wound and the gubernacular veins and external spermatic perforators were isolated and divided. All patients had a lymphatic-sparing technique in addition to the standard arterial-sparing surgery. The mean operative time for the total procedure was 98.7 min. Patients returned home on the day of surgery immediately after recovery from their original anaesthesia, and they were able to resume daily activities within 24 h of surgery, regaining their full activities within 5 days after surgery, with only one dressing changed once weekly at outpatient regular visits.
Results
Of the 78 patients, 74 completed the follow-up of 3 months, only seven failed to attend the 6-month follow-up and 16 continued to the 36-month follow-up; 11 of the latter presented to report paternity. The overall mean sperm density, total sperm motility and sperm morphology increased from 13.44 to 26.48 million/mL, from 27.4% to 53% and from 41.4% to 65.0%, respectively (). The differences were statistically significant for all variables P < 0.001).
Table 1 The mean values of semen variables before and at 3 or 6 months after surgery in all patients.
For each group separately the changes in the three variables from before to after surgery were significant for both sperm density and sperm motility in each group (A,B and ), but for sperm morphology there were significant improvements in all groups except E (C and ).
Figure 1 The degree of improvement in (A) sperm density, (B) total sperm motility and (C) sperm morphology in each group.
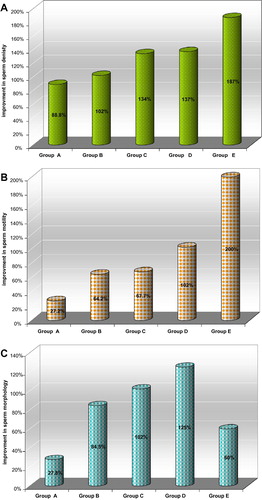
Table 2 The mean values of sperm density, motility and morphology before, and 3 or 6 months after surgery in each group according to the grade of varicocele.
The paternity rate up to 24 months of follow-up was 21 of 78 (26.9%), which increased to 32 men (41%) who reported paternity by natural pregnancy within 36 months of follow-up. Most of these patients presented with high-grade varicoceles (six of eight from group E, six of 11 in group D, 10 of 25 in group C, six of 12 in group B and four of 13 in group A) and the differences were statistically significant.
During the follow-up none of the patients developed a hydrocele and/or lymphocele; only one young man developed a recurrence of a left varicocele within the first year of follow-up. Three patients developed bilateral testicular pain in the first 3–6 months, in whom scrotal duplex US showed thrombotic gonadal veins at the testicular site but with no refluxing vessels seen (no flow). Two patients developed a cord-like swelling on the dorsal aspect of the penis immediately after surgery, diagnosed by duplex US as thrombotic dorsal veins of the penis; this resolved completely with local penile anti-inflammatory and anti-oedema medication, in addition to analgesics. In these two patients many veins in the floor of the canal were ligated, in addition to the standard surgery.
Discussion
Varicocele is the most common treatable condition in men with infertility. Although varicocele is also detected in the general population it is more common in infertile men and treatment can be of benefit for some infertile couples [Citation13]. Steckel et al. [Citation10] reported that the grade of varicocele had a significant effect on the outcome of varicocele ligation, either unilateral or bilateral. Men with a large varicocele grade had a greater improvement in semen quality after surgery than men with a small low-grade varicocele. However, patients with a smaller varicocele usually have more normal baseline semen values and therefore the postoperative changes are less significant [Citation14]. Using subinguinal microsurgical varicocele ligation [Citation15] in 1500 men, the paternity was 43% after 1 year and 69% after 2 years, compared to 16% in couples with men who declined surgery and had hormone treatment or used insemination. Cayan et al. [Citation1] reported final data after using subinguinal microscopic ligation in 540 infertile men with clinically palpable varicocele; 84% of candidates for in vitro fertilisation before surgery became candidates for intrauterine insemination or natural conception after surgery. Most studies report a natural pregnancy rate after microscopic varicocele ligation of 20–40%. In the present study the natural pregnancy rate was 24.5% within the first 2 years of follow-up and this increased 32 men (41%) who reported paternity by natural pregnancy within 3 years, a result similar to that obtained by others and that could be explained by the high rate of bilateral subinguinal varicocele ligation in the study of Cayan et al. (73%) and the longer follow-up [Citation1].
In the present study bilateral microscopic subinguinal varicocele ligation increased the sperm count, total sperm motility and sperm morphology by about half the preoperative value (). Hussein [Citation16] reported a good outcome (an improvement of >50%) in sperm concentration, forward progressive motility and sperm morphology in 58.7% 27.9% and 17.3% of patients. Another study [Citation17] reported a good outcome for sperm count and sperm motility in 36.6% and 53.7% of patients. These results are consistent with the present results. Al-Said et al. [Citation18] included 298 infertile patients (446 varicoceles) who were randomised to varicocele ligation using three different methods, and the authors found that early postoperative complications were comparable in the three groups. At the follow-up none of the patients in the microsurgical group had hydrocele, while four of 143 (2.8%) in the open group and eight of 148 (5.4%) in the laparoscopy group (a significance difference in favour of microsurgery). The incidence of recurrent varicocele was significantly lower in the microsurgical group than in the open and laparoscopy groups (four of 155 patients, 2.6%, vs 16 of 143, 11%, and 25 of 148, 17%, respectively). They also compared the semen values before the three surgical procedures with those after surgery, reporting a statistically significant improvement in sperm concentration, motility and morphology. They also reported that the incidence of patients with an improved sperm count and motility was significantly higher in the microsurgical than in the other two groups, and the incidence of pregnancy within a year was not significantly different among the three groups. A limitation in the present series was that there was no direct comparison with other surgical techniques.
The most surprising outcome of the present series was that the five patients who had more veins ligated in the floor and in the medial aspect of the inguinal canal had significant subjective improvements in their erectile quality than present, as assessed using the Sexual Health Inventory for Men before and after surgery, but there we have no explanation of these improvements. The patients might have had a previous venous leak or possibly improved testicular function with a subsequent increase in serum testosterone levels after surgery, or some other cause. Further study is needed to explain this issue, and in future penile duplex US will be used in all patients with erectile dysfunction in an upcoming prospective study. In the present series there was only one patient with a recurrent varicocele (left side) in whom an additional surgical technique (visual internal urethrotomy) was used at the same surgery.
The main limitation of the present series was the relatively few patients in each group, and that patients were classified according to findings of the physical examination, and not according to the WHO classification. This might have had effects on the objective findings, differing among physicians. In addition the fertility potential of the female partner was not assessed and there was no direct comparison with other surgical techniques. Preoperative testicular volumes and/or biopsies were not assessed in this series and only natural pregnancies were reported.
In conclusion, magnified bilateral varicocele ligation, based on the sum of varicocele grading, significantly improved semen quality and the paternity rate by natural pregnancy in subfertile men.
Conflict of interest
None declared.
Source of funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- S.S.CayanShavakhabovA.KadiogluTreatment of palpable varicocele in infertile men: a meta-analysis to define the best techniqueJ Androl3020093340
- L.DubinR.D.AmelarVaricocele size and results of varicocelectomy in selected subfertile men with varicoceleFertil Steril211970606609
- Y.H.LueB.L.LasleyL.S.LaughlinR.S.SwerdloffA.P.HikimA.LeungetalMild testicular hyperthermia induces profound transitional spermatogenic suppression through increased germ cell apoptosis in adult cynomolgus monkeys (Macaca fascicularis)J Androl232002799805
- World Health OrganizationThe influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinicsFertil Steril57199212891292
- E.D.MatthewsM.GoldsteinInduction of spermatogenesis and achievement of pregnancy after microsurgical varicocelectomy in men with azoospermia and severe oligoasthenospermiaFertil Steril7019987175
- M.GoldsteinSurgery of Male Infertility1995WB Saunders CompanyPhiladelphia
- P.GonteroG.PrettiF.FontanaA.ZitellaG.MarchioroB.FreaInguinal versus subinguinal varicocele vein ligation using magnifying loupe under local anesthesia which technique is preferable in clinical practiceUrology66200510751079
- J.SteckelA.P.DickerM.GoldsteinInfluence of varicocele size in response to microsurgical ligation of spermatic veinsJ Urol1491993769771
- M.GoldsteinB.R.GilbertA.P.DickerJ.DwoshC.GneccoMicrosurgical inguinal varicocelectomy with delivery of the testis: An artery and lymphatic sparing techniqueJ Urol148199218081811
- J.SteckelA.P.DickerM.GoldsteinRelationship between varicocele size and response to varicocelectomyJ Urol1491993769771
- H.GhanemT.AnisA.El-NasharR.ShamloulSubinguinal microvaricocelectomy versus retroperitoneal varicocelectomy comparative study of complications and surgical outcomeUrology64200410051009
- A.M.Al-KandariH.ShabaanH.M.IbrahimY.H.ElshebinyA.A.ShokeirComparison of outcomes of different varicocelectomy techniques open inguinal, laparoscopic, and subinguinal microscopic varicocelectomy: a randomized clinical trialUrology692007417420
- C.V.HoppsM.L.LemerP.N.SchlegelM.GoldsteinIntraoperative varicocele anatomy: a microscopic study of the inguinal versus subinguinal approachJ Urol170200323662370
- M.H.SchlesingerI.F.WiletsH.M.NaglerTreatment outcome after varicocelectomy: a critical analysisUrol Clin North Am211994517529
- J.I.GorelickM.GoldsteinLoss of fertility in men with varicoceleFertil Steril591993613616
- A.F.HusseinThe role of color Doppler ultrasound in prediction of the outcome of microsurgical subinguinal varicocelectomyJ Urol176200621412145
- A.F.Abdel-MaguidI.OthmanMicrosurgical and non magnified subinguinal varicocelectomy for infertile men: a comparative studyFertil Steril57199212891292
- S.Al-SaidA.Al-NaimiA.Al-AnsariN.YounisA.ShamsodiniK.A-sadiqetalVaricocelectomy for male infertility. A comparative study of open, laparoscopic and microsurgery approachesUrology1802008266270