Abstract
Objectives: To assess the value of percentage free prostate-specific antigen (%fPSA) in the detection of prostate cancer among Nigerian men with an intermediate total PSA level (4–10 ng/mL), and to show if the optimum threshold for biopsy is different from Caucasian values when the widely used (six-core, digitally directed) prostate biopsy protocol in Nigerians is applied.
Patients and methods: The study included 105 patients aged >50 years, with a palpably benign prostate gland and intermediate levels of total PSA (4–10 ng/mL). These patients had a free PSA assay and a transrectal digitally directed six-core biopsy of the prostate. The %fPSA was calculated and the optimum threshold value for detecting prostate cancer was determined.
Results: The mean (SD) age of the patients was 64.4 (6.6) years and their mean (SD) total PSA level was 6.6 (1.7) ng/mL. Of these men 14 (13.3%) had cancer of the prostate detected by the prostate biopsy. The %fPSA level related directly to sensitivity values but inversely to the specificity and the positive predictive values. The best threshold of %fPSA for detecting cancer in these men was <40%, with a sensitivity of 100%, specificity of 93.4% and a positive predictive value of 70% (P<0.05).
Conclusions: In evaluating Nigerian patients with a palpably benign prostate gland and within the intermediate total PSA range, when digitally directed biopsy protocol is adopted, a %fPSA threshold of <40% will detect significant percentage of those with prostate cancer, with a minimal number of unnecessary biopsies. This value differs from that reported in western studies in which transrectal ultrasonography-directed biopsy was used.
Introduction
Prostate cancer is the fourth most common cancer in men worldwide [Citation1], with incidence and mortality rates that vary markedly among and within different countries. A study by Osegbe [Citation2] among Nigerian men in 1997 revealed an incidence rate of 127/100,000 men. Eke and Sappira [Citation3], in a study of a similar population, reported an incidence rate of 114/100,000 men. It is believed to be the commonest cancer among Nigerian men [Citation4].
The PSA level in the serum is widely used as a screening test for the early detection of prostate cancer [Citation5]. The lack of specificity of PSA within the intermediate range (4.0–10.0 ng/mL), a diagnostic ‘grey zone’ in which cancer is present in 25% of patients with a palpably enlarged benign prostate gland [Citation6], is one of the limitations of its use. This lack of specificity of PSA in the grey zone is clinically important, considering that ≈30% of patients with prostate cancer in this range already have locally advanced or metastatic disease at the time of a definitive pathological assessment [Citation5, Citation7] .
Early disease is mostly found in patients with a total PSA (tPSA) level of <10.0 ng/mL, whereas more than half of patients with tPSA levels of >10.0 ng/mL have advanced disease [Citation5]. Thus the detection of prostate cancer in its potentially curable stage requires the use of low tPSA threshold values for screening, which leads to many unnecessary biopsies.
PSA isoforms found in the serum include free unbound PSA and complexed PSA which is bound to protease inhibitors [Citation4, Citation9] . Assaying the various isoforms of PSA in serum helps to discriminate between prostate cancer and benign prostatic pathologies [Citation10, Citation11] . The percentage free PSA (%fPSA) has been found to be lower in the serum of patients with prostate cancer than in those with a normal or enlarged benign prostate gland [Citation12, Citation13] . Lower values of %fPSA are associated with an aggressive form of prostate cancer [Citation14–Citation16] .
The use of %fPSA in evaluating patients for prostate cancer within the intermediate tPSA range is well established, but the optimum threshold values reported previously vary among authors. The commonly used value is that reported by Catalona et al. [Citation6], who documented a 95% sensitivity at a threshold of <25% fPSA. In that study the risk of cancer was highest (55–56%) at 0–10% fPSA, but decreased to 5–9% when the %fPSA was >25%. In other studies with a smaller sample, Matsuyama et al. [Citation17] found a 91% sensitivity at the 17% fPSA level, while Kuriyama et al. [Citation18] documented an optimum %fPSA value of <15.5% at 85% sensitivity.
The values of tPSA has been shown to differ across races. Men of African descent in the USA have higher tPSA values than white men [Citation19]. However, opinion is divided among authors on the racial variation of %fPSA between American black and white men. While Catalona et al. [Citation20] reported no difference between the populations, Fowler et al. [Citation21], in their study of 222 black and 298 white men with tPSA values of 2.5–9.9 ng/mL, showed racial differences in the relationship between %fPSA and not the incidence but the cut-off for prostate cancer. In that study, when the sensitivity of %fPSA was set at 95%, the optimum %fPSA was 35.2% in black men and 29.2% in white men. They subsequently concluded that the clinical application of the commonly used %fPSA threshold of <25% to determine the advisability of a prostate biopsy might lead to an under-diagnosis of early stage cancer, especially in black men, who are at a greater risk of morbidity and mortality from this disease than white men.
In Nigeria, the tPSA assay has been fully established but that for fPSA is gradually being introduced. In most centres in the country prostate biopsy is indicated when the tPSA level is >10 ng/mL, thereby presumably missing cancers that exist in men with an intermediate tPSA value. This practice of taking a biopsy only in patients with a tPSA of >10 ng/mL is an attempt to avoid unnecessary biopsies in men with a tPSA level in the grey zone. The commonly used technique of biopsy in most centres is digitally directed six-core biopsy, as the facility for TRUS guidance is lacking.
Considering the challenges of managing the Nigerian African patient with prostate cancer, i.e. a high disease burden and limited facilities for diagnosis, in this study we aimed to assess the value of %fPSA for detecting cancer in men with an intermediate tPSA level, and to show if the optimum threshold for this black population differed from values in Caucasians when a six-core, digitally directed prostate biopsy protocol was applied. This should aid in the decision for prostate biopsy in the grey zone of tPSA among this population until the use of more appropriate diagnostic tools becomes widespread.
Patients and method
Ethical approval for the study was obtained from the research and ethics committee of Lagos University Teaching Hospital. This was a prospective observational study to assess the value of %fPSA in all patients aged ⩾50 years seen in the Urology clinic of the hospital between January 2010 and December 2010. All the selected patients had an intermediate tPSA level (4–10 ng/mL) and a palpably benign prostate gland. Patients who had abnormal findings of the prostate on a DRE, or a UTI or prostatitis, and those with any history of treatment for prostate cancer or of previous prostate surgery, were excluded from the study.
All the selected patients who gave consent after appropriate counselling had a comprehensive clinical evaluation, which included any relevant history, a focused physical examination, which included a DRE of the prostate gland, urine analysis, urine microscopy, culture and sensitivity, transabdominal ultrasonography of the prostate, and total, free and %fPSA levels were analysed.
Serum sample collection, storage and assays
Blood samples were obtained from all 125 patients initially seen in the clinic and who had a tPSA level in the intermediate range. The samples were separated and refrigerated at −70 °C within 2 h of collection until analysed. Assays for repeat tPSA and fPSA were then conducted in three batches for all the samples using an ELISA kit (TECO Inc, California, USA). The result was read using a microtitre-well reader. Immunoassay quality control sera (Biorad, Hercules, CA, USA) were used to monitor the precision of the results. The final 105 patients had their repeat tPSA level within the intermediate range and were included in the study.
Prostate biopsy
All patients subsequently had a six-core transrectal digitally guided biopsy of the prostate after an adequate bowel preparation. Intravenous broad-spectrum prophylactic antibiotics with anaerobic cover were administered 30 min before the procedure and continued for 5 days afterwards. An intrarectal anaesthetic gel, intravenous analgesic and sedatives were also used, depending on the pain threshold of the patient. Prostate specimens were procured with the patient in left lateral position using a spring-loaded 16-G Trucut needle and transrectal digital guidance. The specimen was stored in 10% formalin and examined histopathologically using haematoxylin-eosin staining.
The data were analysed using a multipurpose computer statistical programme. The %fPSA was calculated as the ratio of fPSA to tPSA multiplied by 100. Results were expressed using tables and charts. Fisher’s exact or a t-test was used where appropriate, with P < 0.05 taken to indicate significant differences. Receiver-operating characteristic (ROC) curves were generated for %fPSA by plotting sensitivity vs. (1 – specificity) using Analyse–it for Microsoft Excel (version 2.2) software. The collected data were also analysed for Gleason scores in relation to the %fPSA values of the patients.
Results
Of the 125 patients assessed, 105 were finally enrolled into the study after the repeat PSA test; 20 had a repeat tPSA level of >10 ng/mL and were excluded. The mean (SD, range) age of the patients was 64.4 (6.6, 50–80) years. One of three patients with a family history of prostate cancer had a positive biopsy report for prostate cancer. The mean (SD, range) prostate volume was 87.7 (57.1, 63–276) mL. The mean values of tPSA, fPSA and %fPSA are shown in . The histological reports of the prostatic biopsy specimens showed malignancy in 14 (13%) of the men, most of whom (11) were aged 61–70 years.
Table 1 The values of PSA and its derivatives.
shows that all of the patients with prostate cancer had a %fPSA of < 40% while most (85, 93%) of the patients with BPH had a %fPSA of >40%. Most of the patients with cancer (eight) had a %fPSA of 11–20%, while only one each had a value of 0–10% or 31–40%. The %fPSA related directly to sensitivity, but inversely to specificity and positive predictive value (PPV).
Table 2 The %fPSA and histological diagnosis.
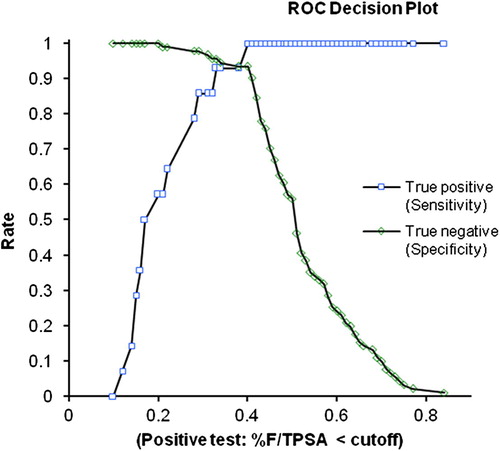
The sensitivity and 1 – specificity were used to construct the ROC curve (), which is important in assessing the validity of the test (%fPSA). The ROC curve increased rapidly to the top left of the plot, suggesting a strong association. The area under the curve (AUC) was 0.99 and was significant at P < 0.001. From the decision plot () the point at which the sensitivity and the specificity curves crossed was at <40% fPSA. This signifies the best threshold level where the maximum numbers of cases are correctly diagnosed as either positive or negative for cancer.
Figure 1 The ROC curve showing the sensitivity (true-positive rate) against (1 – specificity) (false-positive rate) for %fPSA levels. The AUC was 0.99, and P < 0.001.
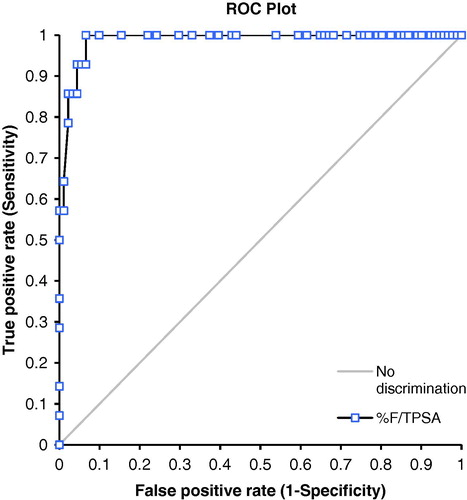
Figure 2 A decision plot showings the sensitivity (true-positive rate) and specificity (true-negative rate) curves of %fPSA levels. The point where the lines cross is the optimum threshold level. From the plot the decision level for %fPSA that optimally identified all the patients with cancer of the prostate (true positive) or nodular hyperplasia (true negatives) was <40%.
The sensitivity, specificity and PPVs at various values of %fPSA are summarised in . The number of patients with BPH who would be biopsied unnecessarily at a threshold %fPSA of <25% was two (2.4%), while missing three patients with cancer, with a sensitivity of 78.6%. When the %fPSA threshold was increased to <40% the sensitivity increased to 100% with a minimal loss in specificity (93.4%) and PPV (70%). Only six patients (7%) with BPH would be biopsied unnecessarily at this level, while no patient with cancer would be missed. The risk of prostate cancer was highest (100%) at a %fPSA of 0–10%, while it was lowest (25%) at 30–40%.
Table 3 The sensitivity, specificity and PPVs at various thresholds of %fPSA.
When the performance of %fPSA was assessed against the tPSA threshold at >4 ng/mL the percentage of unnecessary biopsies that would be taken if a tPSA level of >4 ng/mL was used as the sole criteria was 87%. This was much higher than the value obtained (5.7%) when patients for biopsy were selected using a %fPSA of <40% as the threshold.
For the degree of cellular differentiation, 10 of the 14 patients with cancer had moderately differentiated tumour (Gleason score 5–7), three had tumours that were well differentiated (Gleason score 2–4), while one had high-grade tumour (Gleason score 8–10). There was an inverse relationship between the score and the %fPSA (). Patients with the lowest score (2) had a %fPSA of <38% while the patient with the highest score (9) had a %fPSA of 10% ().
Table 4 Gleason scores and %fPSA values of the 14 patients with prostate cancer.
Discussion
Prostate cancer is the commonest malignancy among adult Nigerian men [Citation2]; in the USA it is the leading cancer diagnosis and the second most common cause of cancer death among men [Citation16]. Screening for prostate cancer is controversial, partly because of concerns about specificity but also because there are no long-term studies evaluating the outcome of treatment. The prevalence rate of prostate cancer was 22% in men with an intermediate tPSA level in the study by Catalona et al. [Citation22]. The %fPSA has also been shown by various studies to have a high sensitivity and specificity for prostate cancer in the intermediate tPSA range [Citation6, Citation13] . However, opinion is divided among authors on whether the choice of an optimum threshold is affected by racial differences in the study population; this controversy is highlighted by the various optimum thresholds that have been recorded in studies among populations of different races ().
Table 5 The variation in the optimum %fPSA based on race.
The evaluation of patients with an intermediate tPSA level and normal findings of the prostate on a DRE is not widely practised in centres in Nigeria. Reports on the prevalence and management of prostate cancer in this group of patients are lacking. Most centres only take a prostate biopsy for this category of patients when the prostate is suspicious on a DRE or when the clinical features are not in keeping with benign disease. The technique of biopsy used for most of these patients is a six-core digitally directed biopsy of the prostate, due to the unavailability of facilities for TRUS-guided biopsy.
The 105 patients in the present study had a mean age range of 64.4 years and a mean tPSA level of 6.6 ng/mL, which is a little higher than that documented by Laguna et al. [Citation23] (6.39 ng/mL) in a study involving mainly Caucasian population. The higher value in the present study might be related to the fact that black men have been shown to have a high tPSA level [Citation24]. The mean (SD, range) prostate volume of the present patients was 87.7 (57.1, 63–276) mL. These high volumes suggest that Nigerian Africans have a higher prostate volume and this might be contributory to the high mean tPSA level in this study, as prostate volume correlates well with tPSA level [Citation25].
The histological report of the present patients showed that 13% of them had prostate cancer. This is lower than the value obtained (25%) in a previous similar study [Citation6]. The reason for this low yield is possibly related to the use of digital guidance for the biopsy, as against TRUS-guided biopsy used in the earlier study. However, the tPSA levels for black men has been shown to be higher than that of Caucasians, as noted earlier [Citation24], and thus when they develop prostate cancer they are likely to have a value above the grey zone, considering that the basal level is already high, and hence most are above the range studied.
When the patients were categorized according to the %fPSA levels, all 14 with prostate cancer had a %fPSA of <40%, while 85 (93%) of those with BPH had a value of >40%. This result is in keeping with a report [Citation17] that patients with prostate cancer have a lower %fPSA than those with benign disease of the prostate. The risk of cancer was highest in the 0–10% fPSA range and lowest in the 30–40% range. Hence the risk increased with a decrease in %fPSA, which is in keeping with an earlier documented trend [Citation6]. This is of clinical importance in that patients in the high-risk range (0–20% fPSA) might not be required to meet any other criteria before proceeding to biopsy, as the probability of cancer is high (88.9–100%) in this range. Those in the 21–40% range with a cancer risk of 25–66.7% might require further evaluation with other analytical assessments like PSA density and age-related PSA levels before progressing to biopsy.
From the decision plot () the threshold that optimally discriminated between patients who had cancer and those who did not was <40%. Considering the need for cancer-detecting tests to have high sensitivity and specificity values, a higher %fPSA threshold (40%) that has excellent sensitivity and specificity would be beneficial to the population, as there were few unnecessary biopsies at this level (six patients).
The ROC curve () for the data increased rapidly towards the top left of the plot, implying that the test (%fPSA) correctly identified men with cancer, as most stayed on the left side of the diagonal grey line (a guideline for a test that is unable to correctly identify cases). The AUC was 0.99, which is higher than the non-discriminatory line (0.5), thus indicating that the diagnosis of the disease (cancer) by the test (%fPSA) was not by chance (P < 0.001).
Considering that a %fPSA of <25% is the widely used threshold below which a prostate biopsy is considered for patients in the intermediate tPSA range, the present study showed that at a threshold of <25% the sensitivity was 78.6% (P < 0.005), the specificity 97.8% and the PPV 84.6%. This sensitivity value is lower than that (95%) documented by Catalona et al. [Citation6] at a threshold %fPSA of 25%, and that by Matsuyama et al. [Citation17] who found a sensitivity of 91% at a threshold of <17% fPSA, and therefore probably not the best for the present study population. The optimum threshold of <40% fPSA found in the present study is similar to that reported by Fowler et al. [Citation21] (<35.2% fPSA) in a study involving a significant population of black men, in which they concluded that the lower commonly used %fPSA threshold might not be suitable for a black population, where the burden of prostate cancer is high.
The Gleason score was related inversely to the %fPSA (), implying that less-aggressive cancers were found among those with a high %fPSA and more aggressive disease among those with a low %fPSA. This is of prognostic importance, as patients with a lower %fPSA are likely to have a worse outcome than those with higher values. This is consistent with various reports [Citation14, Citation16] . The Gleason scores of the 14 patients with prostate cancer were also categorised based on the degree of differentiation; 10 were moderately differentiated, while one was poorly differentiated; the remaining three were well differentiated. Although there was a predominance of moderately differentiated cancers in the intermediate tPSA range studied, the one patient who had a poorly differentiated pattern emphasises that a poor prognostic tissue pattern can be found in men with a tPSA level in the grey zone (4–10 ng/mL). This further strengthens the argument for this category of patients to be evaluated for a prostate biopsy using the %fPSA assay, which has been shown to be sensitive in this range.
The limitation of this study is that digital rather than TRUS guidance was used for the prostate biopsy. However, the findings are very relevant in an environment where the mode of biopsy is predominantly digitally guided, as is still used in some African countries. This study is the first to report on the value of %fPSA in the intermediate tPSA range among Nigerian patients with normal DRE findings of the prostate. A larger study incorporating TRUS-guided biopsy is required to augment the results of the present study.
In conclusion, the use of a %fPSA threshold of <40% in evaluating Nigerian patients with a palpably benign prostate gland and an intermediate tPSA range, when six-core digitally directed biopsy is taken, will detect a significant percentage of prostate cancers with no significant increase in the number of unnecessary biopsies. This optimum threshold differs from the <25% value derived from Western studies involving TRUS-guided biopsy.
Source of funding
This research did not receive any grant or fund from any organisation. It was funded solely by the authors.
Conflict of interest
None declared.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- D.M.ParkinP.PisaniJ.FerlayEstimates of the worldwide incidence of 25 major cancers in 1990Int J Cancer801999827
- D.N.OsegbeProstate cancer in Nigerians. Facts and nonfactsJ Urol157199713401343
- N.EkeM.K.SapiraProstate cancer in Port Harcourt, Nigeria: Features and outcomesNig J Surg Res420023444
- J.O.OgunbiyiO.B.ShittuIncreased incidence of prostate cancer in NigeriansJ Natl Med Assoc91999159164
- W.J.CatalonaJ.P.RichieF.R.AhmannM.A.HudsonP.T.ScardinoR.C.FlaniganetalComparison of digital rectal examination and serum prostate-specific antigen in the early detection of prostate cancer: results of a multicenter clinical trial of 6,630 menJ Urol151199412831290
- W.J.CatalonaA.W.PartinK.M.SlawinM.K.BrawerR.C.FlaniganA.PateletalUse of the percentage of free prostate-specific antigen to enhance differentiation of prostate cancer from benign prostatic disease: a prospective multicenter clinical trialJAMA279199815421547
- W.J.CatalonaD.S.SmithT.L.RatliffJ.W.BaslerDetection of organ-confined prostate cancer is increased through prostate-specific antigen-based screeningJAMA2701993948954
- A.ChristenssonC.B.LaurellH.LiljaEnzymatic activity of prostate-specific antigen and its reactions with extracellular serine proteinase inhibitorsEur J Biochem1941990755757
- H.LiljaA.ChristenssonU.DahlénM.T.MatikainenO.NilssonK.PetterssonetalProstate-specific antigen in human serum occurs predominantly in complex with alpha1-antichymotrypsinClin Chem37199116181620
- U.H.StenmanJ.LeinonenH.AlfthanS.RannikkoK.TuhkanenO.AlfthanA complex between prostate-specific antigen and alpha-1-antichymotrypsin is the major form of prostate-specific antigen in serum of patients with prostatic cancer assay of the complex improves clinical sensitivity for cancerCancer Res511991222226
- A.ChristenssonT.BjorkO.NilssonU.DahlénM.T.MatikainenA.T.CockettetalSerum prostate-specific antigen complexed to alpha-1-antichymotrypsin as an indicator of prostate cancerJ Urol1501993100105
- J.E.OesterlingS.J.JacobsenG.G.KleeK.PetterssonT.PiironenP.A.AbrahamssonetalFree, complexed and total serum prostate-specific antigen: the establishment of appropriate reference ranges for their concentrations and ratiosJ Urol154199510901095
- H.TanakaS.MurakamiT.IgarashiT.AbeK.SuzukiN.SekitaetalFree/total PSA ratio of prostate-specific antigen (PSA) for prostate cancer detection in patients with gray zone PSA levelHinyokika Kiyo431997855860
- C.G.ArcangeliD.L.ShepherdD.S.SmithP.A.HumphreyD.W.KeetchW.J.CatalonaCorrelation of percent free PSA and pathologic features of prostatic carcinomasJ Urol155Suppl.1996415
- H.B.CarterA.W.PartinA.A.LudererE.J.MetterP.LandisD.W.ChanetalPercentage of free prostate-specific antigen in sera predicts aggressiveness of prostate cancer a decade before diagnosisUrology491997379384
- J.PannekH.G.RittenhouseD.W.ChanJ.I.EpsteinP.C.WalshA.W.PartinThe use of percent free PSA for staging of men with clinically localized prostate cancerJ Urol159199812381242
- H.MatsuyamaY.BabaG.YamakawaN.YamamotoK.NaitoDiagnostic value of prostate-specific antigen-related parameters in discriminating prostate cancerInt J Urol72000409414
- M.KuriyamaY.KawadaY.AraiH.MaedaS.EgawaK.KoshibaetalSignificance of free to total PSA ratio in men with slightly elevated serum PSA Levels: a Cooperative StudyJ Clin Oncol281998661665
- T.O.MorganS.J.JacobsenW.F.McCarthyD.G.JacobsonD.G.McLeodJ.W.MoulAge-specific reference ranges for serum prostate-specific antigen in black menN Engl J Med3351996304310
- W.J.CatalonaA.W.PartinK.M.SlawinC.K.NaughtonM.K.BrawerR.C.FlaniganetalPercentage of free PSA in black versus white men for detection and staging of prostate cancer: a prospective multicenter clinical trialUrology552000372376
- J.E.FowlerJr.J.SandersS.A.BiglerJ.RigdonN.K.KilambiS.A.LandPercent free prostate specific antigen and cancer detection in black and white men with total prostate specific antigen 2.5-9.9 ng./mlJ Urol163200014671470
- W.J.CatalonaD.S.SmithT.L.RatliffK.M.DoddsD.E.CoplenJ.J.YuanetalMeasurement of prostate-specific antigen in serum as a screening test for prostate cancerN Engl J Med324199111561161
- M.P.Laguna PesC.Guinda SevillanoA.Zazo RomojaroJ.DomínguezA.García LuzónJ.Borrego HernandoetalClinical usefulness of free PSA/total PSA ratio in the early diagnosis of prostatic cancerArch Esp Urol532000333341
- R.SawyerJ.J.BermanA.BorkowskiG.W.MooreProstate-specific antigen in black menLancet34719961329
- F.M.AbbiyesukuO.B.ShittuO.O.OduwoleB.O.OsotimehinProstate specific antigen in the Nigerian AfricanAfr J Med Med Sci29200097100