Abstract
Objectives: To review previous reports and discuss current trends in extracorporeal shockwave lithotripsy (ESWL), percutaneous nephrolithotomy (PCNL) and ureterorenoscopy (URS). ESWL was recommended as the first-line treatment for small and intermediate-sized stones in the lower pole, while it is the standard treatment for large stones. However, the stone clearance rate after ESWL seems to be lower than that of stones in other locations. This seems to result from a lower rate of fragment passage, due to anatomical factors.
Methods: Reports on urinary stone disease were reviewed, assessing only publications in peer-reviewed, Medline-listed journals in the English language (publication years 1990–2011).
Results: Recent experience with flexible URS (fURS) for intrarenal stones showed that excellent stone-free rates can be achieved. With increasing experience and technically improved equipment, fURS has become an alternative to ESWL for small and intermediate-sized renal stones. Furthermore, several authors reported successful retrograde treatment for large renal stones, proposing fURS as an alternative to PCNL. However, the major drawbacks are long operating times and commonly, staged procedures, which is why PCNL remains the method of choice for such stones.
Conclusions: Considering the currents trends and evidence, the 2012 update of the European Association of Urology Guidelines on Urolithiasis has upgraded the endourological treatment of kidney stones. Individual factors such as body habitus, renal anatomy, costs and patient preference must be considered.
Introduction
Since its introduction in the early 1980s, ESWL became the method of choice for treating most upper urinary tract calculi, and replaced open and percutaneous procedures [Citation1–Citation3]. To date, guidelines have confirmed ESWL as the method of first choice for small and mid-sized urinary calculi. However, currently urologists and patients are more critical about ESWL when considering the best treatment for a stone. The limited results of ESWL, even after repeated treatment sessions for stones e.g., in the lower pole, or for difficult stone compositions like calcium oxalate monohydrate, brushite or cystine, might explain this development. At the same time endourological techniques and skills, especially for flexible ureterorenoscopy (fURS) have been improved significantly, making fURS both very efficient and safe [Citation4–Citation6].
Percutaneous nephrolithotomy (PCNL), established in the 1970s, has replaced open surgery for large stones. As the morbidity has decreased with improving experience it is increasingly used even for mid-sized stones in the lower pole. Various other factors also have to be considered when making the choice of an optimum treatment, e.g. body habitus, renal anatomy, treatment costs, patient preference, and local infrastructure in terms of expertise and equipment [Citation7]. In this review we aim to give an overview of current techniques and results, discussing the advantages and disadvantages of each procedure, and future trends.
ESWL
Traditionally, ESWL was the preferred first-line treatment for small to intermediate-sized renal stones. However, its limitations are most apparent in the treatment of stones within the lower pole, where the compromise is on a reduced stone-free rate (SFR) of 25–84%, depending on the experience of the operator and the machine used. Therefore, ESWL has been considered for lower-pole stones of up to 1.5 cm. There is a widespread consensus within the urological community that larger stones in the lower pole of the kidney should be approached using PCNL.
Factors for successful ESWL in the lower pole
The gravity-dependant position of the lower pole calyces is considered as the main factor for impeded fragment clearance after ESWL [Citation8], whereas others have reported that stone size is the most important factor in the lower pole [Citation9]. From the late 1990s several authors postulated a negative effect of renal anatomical factors on the clearance of lower-pole fragments after ESWL (Box 1) [Citation10–Citation14]. However, more recent studies could not confirm these findings in either adults [Citation15] or in children [Citation16]. The skin-to-stone distance has likewise been postulated as a determining factor, but this has not found widespread acceptance to date [Citation17]. Further anatomical variables cannot be established yet. The value of supportive measures, e.g. inversion, vibration or hydration, remains under discussion [Citation10,Citation18]. Thus, many factors have been implicated in impeding fragment clearance from the lower pole, but discussion continues and the topic remains controversial.
Box 1 Factors that make successful ESWL less likely.
Shockwave-resistant stones (calcium oxalate monohydrate, brushite, cystine)
Steep infundibular-pelvic angle, of <45°,
Infundibular length of <30 mm
infundibular width of <5 mm
Long lower pole (>10 mm)
Despite being minimally invasive, shock waves induce transient damage to the renal parenchyma [Citation19,Citation20]. Recently, new treatment strategies have been established which reduce tissue trauma by using a low-energy shockwave pretreatment, followed by the usual high-energy therapeutic treatment. This induces parenchymal vasoconstriction during ESWL, rather than afterwards, as is the case with no pretreatment [Citation21]. Reducing the shock-wave rate to 60/min improves stone disintegration and reduces tissue damage [Citation22]. This might make ESWL less minimally invasive and more attractive even in situations where a better clearance rate might be achieved by more aggressive approaches, such as in small lower-pole calyceal stones.
Efficacy
When assessing the SFR after ESWL of lower pole stones most authors give the stone-free status at 3 months after treatment. Most authors differentiate between stones of <10 mm, 10–20 mm, and >20 mm. The SFR in these groups is 64–84%, 38–66%, and 25–49%, respectively () [Citation11,Citation23–Citation25]. Lingeman et al. [Citation26] published a meta-analysis in 1994 comparing ESWL and PCNL for treating lower-pole stones. PCNL was associated with a significantly higher SFR of 90%, vs. 59% for ESWL. Stone size was a negative factor for the outcome of ESWL but not for PCNL. The Lower Pole Study Group reported a randomised controlled trial comparing ESWL with PCNL [Citation27]. Again, at 3 months, PCNL was associated with an excellent SFR of 97%, compared to only 37% after ESWL. When stratifying for stone size, the SFR after ESWL for stones of <10 mm was 63% and decreased to 21% for stones of 10–20 mm and 14% for those of >20 mm. The length of hospital stay was shorter for ESWL. In summary, our experience and available reports suggest that ESWL remains an acceptable approach for lower-pole stones of <10 mm, but for larger stones the endourological techniques seem to offer a higher efficacy.
Table 1 Treatment options for lower-pole stones.
fURS
The lower pole can be accessed in almost all cases by using the latest generation of flexible endoscopes. Technical developments have increased the number of URS procedures for stones within the upper urinary tract. To date, fURS has been recommended as a second-line treatment for calculi of <1 cm, or as the third choice for stones of 1–2 cm, by the Guidelines of the European Association of Urology (EAU). fURS was not recommended for stones of >2 cm [Citation28]. This has changed with the 2012 update of the EAU [Citation29]. While fURS is still considered as a second choice for small stones it has now been upgraded as an alternative to PCNL for stones of intermediate size (1–2 cm). ESWL has been downgraded to the second choice for such stones.
Factors for successful fURS in the lower pole
Technological advances have been responsible for the development of fURS, especially for improved deflection mechanisms that facilitate intrarenal manoeuvrability [Citation30]. Modern endoscopes with outer diameters of <9 F allow direct access to the upper urinary tract without dilatation of the ureteric orifice in almost all cases [Citation5,Citation6,Citation31–Citation33]. The use of access sheaths further facilitates the procedure and seems to improve the outcome [Citation34,Citation35]. Furthermore, the latest generation of flexible endoscopes seems to have overcome the problem of constant technical defects and led to a wider use of fURS [Citation36–Citation39]. As a result, the lower pole is accessible with the latest endoscopes in almost all cases. A further advance to a better quality of fURS is the introduction of digital endoscopes; these eliminate the need for fragile low-resolution fibre-optics, and the tips of these instruments contain digital camera chips (complementary metal-oxide semiconductors or charge-coupled devices) which produce superior image resolution. The tips also have light-emitting-diode-driven carriers, which provide a substitute for an external light source. Initial experience with digital ureteroscopes has given a marked improvement in image quality, leading to faster procedures [Citation40].
Efficacy
The Lower Pole Study Group conducted a second randomised controlled trial, published in 2005, comparing fURS with ESWL for small lower-pole stones [Citation41]. At 3 months of follow-up fURS did not produce a statistically significantly better outcome than ESWL (SFR 50% vs. 35%, fURS vs. ESWL, respectively). Interestingly the complication rates, length of hospital stay and the need for secondary procedures were comparable. Although this study did not show what most urologists expected (that fURS was better than ESWL) its limitations must be considered. There were relatively few patients, and 19 centres recruiting patients had a different caseload and equipment. However, the role of fURS for the lower pole remains poorly defined because there are no high-quality studies.
In recent years several authors reported the feasibility of retrograde stone removal even for larger stones, which are usually treated by PCNL [Citation24–Citation27]. In our series, fURS achieved a high SFR after 4 weeks, which was close to that reached by PCNL [Citation42], but half of all patients required two procedures, with significantly longer operating times and consequently a longer treatment period. These results were in accordance to other series on fURS for large calculi [Citation43,Citation44]. Although pre-stenting is usually not a necessary requirement for fURS, it seems to have advantages for patients with a large stone burden. However, the high rate of preoperative JJ placement is a significant disadvantage for fURS in this series, because of the potential discomfort and morbidity to the patient.
PCNL
PCNL was established as a minimally invasive treatment option for kidney stone removal in the 1970s and was further developed over the following years [Citation45]. It has a confirmed efficacy for managing lower-pole renal calculi, with a constantly high SFR independent of stone size [Citation26]. The Lower Pole I Study showed SFRs of 100%, 93% and 86% for stones of <1 cm, 1–2 cm and larger stones, respectively [Citation27]. Other studies have confirmed these excellent results [Citation46,Citation47].
The introduction of so-called mini-PCNL has further contributed to a wider use of percutaneous techniques, even for stones of <2 cm [Citation48–Citation50]. The term mini-PCNL is not exactly defined but is usually used for smaller diameter sheaths (mostly 18 F compared to 24–30 F in conventional PCNL). The potential advantages are lower morbidity due to less bleeding, and reduced pain. However, its value is still under discussion [Citation51]. The treatment time is prolonged while the SFR seems to decrease with larger stones. Furthermore, in experienced hands the complications of conventional PCNL are rare [Citation49,Citation52,Citation53]. Lahme et al. [Citation49,Citation54] raised the question of whether mini-PCNL leads to an extension of the indications for percutaneous treatments. Nagele et al. [Citation55] reported the successful and safe use of mini-PCNL even for smaller stones of 8–15 mm. Further studies are needed to assess the value of extending the indications for PCNL treatment and the effect of instrument size.
Discussion
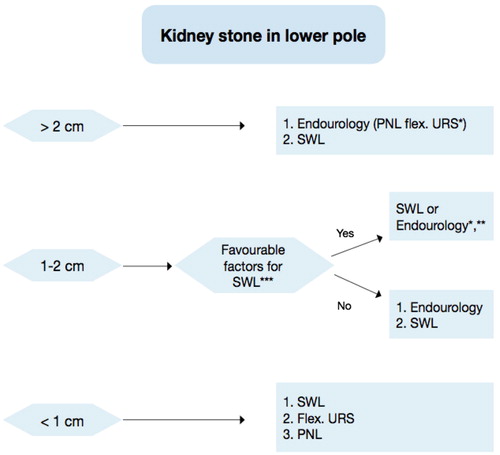
ESWL, especially in an anaesthesia-free outpatient setting, remains the first-line treatment option for small lower-pole stones [Citation56]. It offers an acceptable SFR, few complications and a low recurrence rate [Citation11,Citation24]. According to the updated EAU Guidelines () [Citation29] the treatment outcome for stones of 1–2 cm depends on the predictive factors (Box 1). If the success of ESWL is unlikely the recommended approach is endourology, either retrograde fURS or PCNL. This is a paradigm shift for the value of fURS. While earlier reports failed to show the superiority of fURS over ESWL, the new guideline now considers that current experience gives a different impression [Citation7,Citation57]. In experienced hands fURS is an excellent option to completely remove stones after one session. Furthermore, there are situations where ESWL is either contraindicated or has limited efficacy, e.g. uncorrected bleeding diathesis (although ESWL with low-dose salicylate might be safe [Citation58]), obesity, or complicated anatomy [Citation59]. PCNL is recommended for larger stones of >1.5 cm [Citation23]. It is the most effective treatment but also the most invasive, with a need for general anaesthesia, few but possibly severe complications, and a potentially longer convalescence than after ESWL and fURS [Citation57]. The lower pole is the ideal indication for PCNL because of the easy access and a low complication rate.
Figure 1 A proposed treatment algorithm for lower-pole stones according to the 2012 update of the EAU Guideline on Urolithiasis [Citation29].
In 2009 Srisubat et al. [Citation57] reported a Cochrane analysis of ESWL vs. URS vs. PCNL for treating renal calculi. Based on these data, ESWL had the lowest efficacy while PCNL and URS did not differ significantly. The hospital stay was shorter with ESWL. All three treatments seemed to offer a good chance of rendering the patient stone-free in one session [Citation24]. The authors criticised the low data quality of the available studies; only three studies could be included in the meta-analysis.
Based on current reports, fURS cannot be recommended as a first-line therapy for renal stones of >1.5 cm, although some expert centres have reported such approaches to be effective and safe. The many different staged fURS procedures underline the superiority of PCNL. In special situations a combined approach (PCNL + fURS) might be an option in specialised centres. Despite such developments there can be no doubt that fURS will probably never achieve the same results as PCNL.
However, increasingly many patients cannot be treated by PCNL. The higher incidence of cardiovascular diseases has led to the wide use of anticoagulants. While bleeding disorders are seen as contraindications for both ESWL and PCNL, fURS has shown excellent safety in such patients [Citation60]. Furthermore, insufficient physical activity and poor nutrition lead to increasing numbers of obese and morbidly obese patients. Because of high skin-to-kidney distance the efficacy of ESWL is then limited and PCNL can be practically impossible if the puncture needle cannot reach the kidney, whereas fURS can be used without limiting the outcomes [Citation61].
Conclusions
Renal stones of <10 mm are usually treated successfully with ESWL; larger stones, especially within the lower pole, are more efficiently treated by PCNL [Citation3,Citation27,Citation62]. fURS is recommended as a second-line treatment for smaller lower-pole stones and an as alternative for stones of moderate size if there are negative predictors for the success of ESWL. Despite this recommendation, fURS is already used as the method of choice for such stones by many urologists, but individual factors and preferences must be considered ().
Conflict of interest
None declared.
Funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- C.ChaussyE.SchmiedtD.JochamW.BrendelB.ForssmannV.WaltherFirst clinical experience with extracorporeally induced destruction of kidney stones by shock wavesJ Urol1271982417420
- G.M.PremingerH.G.TiseliusD.G.AssimosP.AlkenA.C.BuckM.Gallucietal2007 Guideline for the management of ureteral calculiEur Urol52200716101631
- H.G.TiseliusD.AckermannP.AlkenC.BuckP.ConortM.GallucciGuidelines on urolithiasisEur Urol402001362371
- C.G.MarguetW.P.SpringhartB.K.AugeG.M.PremingerAdvances in the surgical management of nephrolithiasisMinerva Urol Nefrol5620043348
- Y.H.TanG.M.PremingerAdvances in video and imaging in ureteroscopyUrol Clin North Am3120043342
- G.K.ChowD.E.PattersonM.L.BluteJ.W.SeguraUreteroscopy. Effect of technology and technique on clinical practiceJ Urol170200399102
- J.D.RamanM.S.PearleManagement options for lower pole renal calculiCurr Opin Urol182008214219
- F.J.SampaioRenal anatomy. Endourologic considerationsUrol Clin North Am272000585607
- A.SrivastavaW.ZamanV.SinghA.MandhaniA.KumarU.SinghEfficacy of extracorporeal shock wave lithotripsy for solitary lower calyceal stone: a statistical modelBJU Int932004364368
- S.AlbanisH.M.AtherA.G.PapatsorisJ.MasoodD.StaiosT.SheikhetalInversion, hydration and diuresis during extracorporeal shock wave lithotripsy: does it improve the stone-free rate for lower pole stone clearance?Urol Int832009211216
- Y.S.JuanS.M.ChuangW.J.WuJ.T.ShenC.J.WangC.H.HuangImpact of lower pole anatomy on stone clearance after shock wave lithotripsyKaohsiung J Med Sci212005358364
- L.RuggeraP.BeltramiR.BallarioS.CavalleriL.CazzolettiW.ArtibaniImpact of anatomical pyelocaliceal topography in the treatment of renal lower calyces stones with extracorporeal shock wave lithotripsyInt J Urol122005525532
- A.M.ElbahnasyA.L.ShalhavD.M.HoenigO.M.ElashryD.S.SmithE.M.McDougalletalLower caliceal stone clearance after shock wave lithotripsy or ureteroscopy. the impact of lower pole radiographic anatomyJ Urol1591998676682
- F.J.SampaioM.A.Pereira-SampaioL.A.FavoritoThe pig kidney as an endourologic model: anatomic contributionJ Endourol1219984550
- T.SahinkanatH.EkerbicerB.OnalN.TansuS.ResimS.CitgezetalEvaluation of the effects of relationships between main spatial lower pole calyceal anatomic factors on the success of shock-wave lithotripsy in patients with lower pole kidney stonesUrology712008801805
- B.OnalO.DemirkesenN.TansuM.KalkanR.AltintasV.YalcinThe impact of caliceal pelvic anatomy on stone clearance after shock wave lithotripsy for pediatric lower pole stonesJ Urol172200410821086
- G.PareekS.P.HedicanF.T.LeeJrS.Y.NakadaShock wave lithotripsy success determined by skin-to-stone distance on computed tomographyUrology662005941944
- A.KosarA.OzturkT.A.SerelS.AkkusO.S.UnalEffect of vibration massage therapy after extracorporeal shockwave lithotripsy in patients with lower caliceal stonesJ Endourol131999705707
- J.A.McAteerA.P.EvanJ.C.WilliamsJrJ.E.LingemanTreatment protocols to reduce renal injury during shock wave lithotripsyCurr Opin Urol192009192195
- B.R.MatlagaJ.A.McAteerB.A.ConnorsR.K.HandaA.P.EvanJ.C.WilliamsetalPotential for cavitation-mediated tissue damage in shockwave lithotripsyJ Endourol222008121126
- R.K.HandaM.R.BaileyM.PaunS.GaoB.A.ConnorsL.R.WillisetalPretreatment with low-energy shock waves induces renal vasoconstriction during standard shock wave lithotripsy (SWL): a treatment protocol known to reduce SWL-induced renal injuryBJU Int103200912701274
- J.J.RassweilerT.KnollK.U.KohrmannJ.A.McAteerJ.E.LingemanR.O.ClevelandetalShock wave technology and application: an updateEur Urol592011784796
- K.NovakTreatment of the lower pole nephrolithiasisCas Lek Cesk144Suppl. 220054547
- I.RiedlerH.TrummerP.HebelG.HubmerOutcome and safety of extracorporeal shock wave lithotripsy as first-line therapy of lower pole nephrolithiasisUrol Int712003350354
- C.ObekB.OnalK.KantayM.KalkanV.YalcinA.OneretalThe efficacy of extracorporeal shock wave lithotripsy for isolated lower pole calculi compared with isolated middle and upper caliceal calculiJ Urol166200120812084
- J.E.LingemanY.I.SiegelB.SteeleA.W.NyhuisJ.R.WoodsG.J.FuchsManagement of lower pole nephrolithiasis: a critical analysisJ Urol1511994663669
- D.M.AlbalaD.G.AssimosR.V.ClaymanJ.D.DenstedtM.GrassoJ.Gutierrez-AcevesetalLower pole I. A prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial resultsJ Urol166200120722080
- T.KnollS2 guidelines on diagnostic, therapy and metaphylaxis of urolithiasis. Part 1: diagnostic therapyUrologe A482009917924
- Türk C, Knoll T, Petrik A, Sarica K, Straub M, SeitzC. Guidelines on urolithiasis. <http://www.uroweb.org/gls/pdf/20_Urolithiasis_LR%20March%2013%202012.pdf>. [accessed June 2012].
- G.Wendt-NordahlT.MutP.KrombachM.S.MichelT.KnollDo new generation flexible ureterorenoscopes offer a higher treatment success than their predecessors?Urol Res39June2011185188
- T.KnollG.Wendt-NordahlL.TrojanA.WenkeN.RoederP.AlkenCurrent aspects of stone therapyAktuelle Urol3620054754
- M.T.GettmanJ.W.SeguraCurrent evaluation and management of renal and ureteral stonesSaudi Med J222001306314
- S.PierreG.M.PremingerHolmium laser for stone managementWorld J Urol252007235239
- J.KourambasR.R.ByrneG.M.PremingerDoes a ureteral access sheath facilitate ureteroscopy?J Urol1652001789793
- J.O.L’EsperanceW.O.EkeruoC.D.ScalesJrC.G.MarguetW.P.SpringhartM.E.MaloneyetalEffect of ureteral access sheath on stone-free rates in patients undergoing ureteroscopic management of renal calculiUrology662005252255
- D.H.BagleyR.L.KuoI.S.ZeltserAn update on ureteroscopic instrumentation for the treatment of urolithiasisCurr Opin Urol14200499106
- K.Y.ChiuY.CaiR.MarcovichA.D.SmithB.R.LeeAre new-generation flexible ureteroscopes better than their predecessors?BJU Int932004115119
- O.ShvartsK.T.PerryB.GoffP.G.SchulamImproved functional deflection with a dual-deflection flexible ureteroscopeJ Endourol182004141144
- A.J.TroyT.AnagnostouD.A.TolleyFlexible upper tract endoscopyBJU Int932004671679
- M.BinbayE.YurukT.AkmanF.OzgorM.SeyrekU.OzkuvancietalIs there a difference in outcomes between digital and fiberoptic flexible ureterorenoscopy procedures?J Endourol24201019291934
- M.S.PearleJ.E.LingemanR.LeveilleeR.KuoG.M.PremingerR.B.NadleretalProspective, randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or lessJ Urol173200520052009
- T.KnollJ.P.JessenP.HoneckG.Wendt-NordahlFlexible ureterorenoscopy versus miniaturized PNL for solitary renal calculi of 10–30 mm sizeWorld J Urol292011755759
- A.BredaO.OgunyemiJ.T.LeppertJ.S.LamP.G.SchulamFlexible ureteroscopy and laser lithotripsy for single intrarenal stones 2 cm or greater – is this the new frontier?J Urol1792008981984
- E.S.HyamsR.MunverV.G.BirdJ.UberoiO.ShahFlexible ureterorenoscopy and holmium laser lithotripsy for the management of renal stone burdens that measure 2–3 cm: a multi-institutional experienceJ Endourol24201015831588
- P.AlkenG.HutschenreiterR.GuntherM.MarbergerPercutaneous stone manipulationJ Urol1251981463
- J.de la RosetteD.AssimosM.DesaiJ.GutierrezJ.LingemanR.ScarpaetalThe clinical research office of the endourological society percutaneous nephrolithotomy global study: indications, complications, and outcomes in 5803 patientsJ Endourol2520111117
- T.KnollF.WezelM.S.MichelP.HoneckG.Wendt-NordahlDo patients benefit from miniaturized tubeless percutaneous nephrolithotomy? A comparative prospective studyJ Endourol24201010751079
- U.NageleM.HorstmannK.D.SievertM.A.KuczykU.WalcherJ.HennenlotteretalA newly designed amplatz sheath decreases intrapelvic irrigation pressure during mini-percutaneous nephrolitholapaxy. an in vitro pressure-measurement and microscopic studyJ Endourol21200711131116
- S.LahmeK.H.BichlerW.L.StrohmaierT.GotzMinimally invasive PCNL in patients with renal pelvic and calyceal stonesEur Urol402001619624
- M.MongaS.OglevieMinipercutaneous nephrolithotomyJ Endourol142000419421
- G.GiustiA.PiccinelliG.TavernaA.BenettiL.PasiniM.CorintietalMiniperc? No, thank you!Eur Urol512007810815
- S.V.JackmanS.P.HedicanC.A.PetersS.G.DocimoPercutaneous nephrolithotomy in infants and preschool age children: experience with a new techniqueUrology521998697701
- T.KnollK.HegerA.HaeckerM.OsmanP.AlkenK.U.KohrmannetalPercutaneous nephrolithotomy: experience from 348 proceduresEur Urol (Suppl)3200442
- S.LahmeV.ZimmermannsA.HochmuthP.LiskeStones of the upper urinary tract. Update on minimal-invasive endourological treatmentArch Ital Urol Androl8020081317
- U.NageleD.SchillingK.D.SievertA.StenzlM.KuczykManagement of lower-pole stones of 0.8–1.5 cm maximal diameter by the minimally invasive percutaneous approachJ Endourol22200818511853
- A.N.ArgyropoulosD.A.TolleyOptimizing shock wave lithotripsy in the 21st centuryEur Urol522007344352
- A.SrisubatS.PotisatB.LojanapiwatV.SetthawongM.LaopaiboonExtracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stonesCochrane Database Sys Rev2009CD007044
- G.ZanettiI.Kartalas-GoumasE.MontanariA.B.FedericiA.TrinchieriF.RoveraetalExtracorporeal shockwave lithotripsy in patients treated with antithrombotic agentsJ Endourol152001237241
- G.M.PremingerManagement of lower pole renal calculi: shock wave lithotripsy versus percutaneous nephrolithotomy versus flexible ureteroscopyUrol Res342006108111
- J.D.WattersonA.R.GirvanA.J.CookD.T.BeikoL.NottB.K.AugeetalSafety and efficacy of holmium: YAG laser lithotripsy in patients with bleeding diathesesJ Urol1682002442445
- A.DashT.G.SchusterB.K.HollenbeckG.J.FaerberJ.S.WolfJr.Ureteroscopic treatment of renal calculi in morbidly obese patients: a stone-matched comparisonUrology602002393397
- J.W.SeguraG.M.PremingerD.G.AssimosS.P.DretlerR.I.KahnJ.E.LingemannetalNephrolithiasis clinical guidelines panel summary report on the management of staghorn calculi. The American Urological Association Nephrolithiasis Clinical Guidelines PanelJ Urol151199416481651