Abstract
Objective: To present our recent experience in the management of penile fracture.
Patients and methods: We present 21 cases of penile fracture managed at the two Federal-owned tertiary hospitals in two neighbouring states in south-west Nigeria between 2001 and 2011. The diagnosis was based mainly on a clinical evaluation. The treatment was surgical in patients who presented within 2 weeks of the fracture. The emphasis during the follow-up was on erectile function and micturition.
Results: .Seventeen patients presented within 48 h, two presented after a week, while two reported months later with penile deviation. The mean age of the patients was 26.4 years. The cause of fracture was sexual intercourse in 11 (52%) patients and forceful manipulation of the erect penis in 10 (48%). Thirteen (62%) of all injuries occurred in the last 2 years of the study, of which eight men were injured during rear entry with the woman on top (reverse coital) position. Six of the patients with reverse coital injuries reported trying the position after watching it on the Internet, specifically on their cellular phones. Eighteen patients had surgical treatment, with a satisfactory outcome. Two of the other three patients had penile deviation during erection.
Conclusions: The incidence and causes of penile fracture appear to have changed drastically over the last 2 years in our environment. The rapid demographic changes in south-west Nigeria are probably responsible. There appears to be a relationship between the cause of fracture and the use of the Internet, although that might be coincidental. Surgical repair, irrespective of the delay before intervention, usually offers a satisfactory outcome.
Introduction
Fracture of the penis is an unusual urological emergency, and is generally defined as a rupture of the corpus cavernosum as a result of blunt trauma to an erect penis [[Citation1–Citation3] . Although it was first reported by an Arab physician, Abul Kazeem, over 1000 years ago, its description has often been credited to Malis in 1925 [Citation3, Citation4] . Between 1935 and 2004 only about 1642 cases had been reported, with most occurring in the Mediterranean Muslim region [Citation2, Citation3, Citation5] . The incidence is said to be low in Nigeria, where only 11 cases had been reported by 2002 in a country of >150 million people. The true incidence of penile fracture (PF) is probably unknown because many patients might avoid seeking medical attention because of the embarrassing clinical situation.
In western societies PF is often caused by sexual intercourse [Citation1, Citation3, Citation5] , while in the Middle East forceful bending of the erect penis to achieve detumescence accounts for most cases [Citation3, Citation5, Citation6] . Other reported causes include masturbation, rolling over while in bed, and falling off a bed with an erect penis [Citation3]. While the clinical diagnosis of PF has always been straightforward there have been controversies about evaluation and management of these patients [Citation1, Citation4, Citation7] .
Because it is rare, reports on PF in Sub-Saharan Africa have consisted only of case reports [Citation3,Citation8–Citation10] , but an increasing incidence of PF has long been reported in the authors’ environment [Citation3]. Here we report our experience in the management of PF, and to our knowledge this is the largest single series in sub-Saharan Africa.
Patients and methods
Patients
The records of all patients with a diagnosis of PF, seen at the Lagos University Teaching Hospital and the Federal Medical Centre Abeokuta (both in south-west Nigeria) from 2001 to 2011, were reviewed. Information extracted included the cause of fracture, clinical presentation, physical findings, treatment and its outcome. Whenever it was possible, the patients were also interviewed on their sources of sexual information, with the emphasis on coital position. The diagnosis was based on the clinical findings.
Surgical procedures
All operated patients received preoperative antibiotic therapy. After preliminary urethral catheterisation the penis was explored via a circular subcoronal incision with degloving of the penis. The defect in the tunica was repaired with 3/0 polyglactin interrupted sutures. Any urethral injury when present was repaired with 5/0 polyglactin sutures. The urethral catheter was removed after 24 h or left for 21 days if there was a urethral injury.
Follow-up
All operated patients had postoperative antibiotic cover and were advised at discharge to abstain from sexual activity for 3 months. The emphasis during the follow-up was on the quality of erection and on micturition.
Results
The preoperative diagnosis was correct in all cases. All patients gave a history of a cracking noise during manipulation of the erect penis or sexual intercourse, followed by acute pain, penile detumescence and swelling. In all, 21 patients were seen (mean age 26.4 years), with 17 presenting within 48 h, and two each at 8 and 9 days after injury, respectively ( and ), while two presented at 5 and 6 months after injury with an abnormal penile angulation during erection.
Forceful manipulation of the erect penis was responsible for 10 cases (eight by the patient and two by the partners), while sexual intercourse was responsible for 11. Eight (38%) of all the cases occurred between 2001 and 2009, while 13 (62%) occurred in 2010–2011.
Eight men were injured during rear entry with the woman on top (the reverse coital, RC, position), all of which occurred between 2010 and 2011. Ten patients were interviewed on the source of sexual information. Six patients with RC injury claimed to have started RC after watching it on the Internet, even though two of them had previously seen it in magazines.
Two patients who presented to the authors’ institutions at 5 and 6 months after the injury had consulted General Practitioners in private hospitals within 48 h of their initial injury, where they received conservative management. They had no urinary symptoms. They were referred later because they had an abnormal penile deviation during erection. Examination showed the presence of a palpable plaque in both patients.
All 19 patients who presented within 2 weeks were offered early surgical intervention, with 18 consenting. The patient who refused surgery was managed conservatively with analgesics, ice-packs, antibiotics and bed rest, and reported satisfactory erections and micturition during the follow-up. In the 18 patients who had surgery (11, five and two from sexual intercourse, self-manipulation and manipulation by sexual partners, respectively) the injury was on the left in 11 and right in seven. One patient had a urethral injury. All injuries except three occurred at the base of the penis. The mean hospital stay was 5 days. All patients who had surgery had an uneventful postoperative period, with satisfactory erections and micturition at the follow-up. The mean (range) follow-up was 10 (6–23) months.
Discussion
PF is regarded as uncommon, particularly in sub-Saharan Africa, where only 12 cases had been reported by 2002 [Citation3]. In the present study 21 cases were reported within 11 years, with an 11-fold increase in 2011 alone. While earlier cases were caused mainly by digital manipulation, sexual intercourse (mainly in the RC position) was responsible for three-quarters of the last 13 cases.
PF is an unusual injury with a straightforward clinical diagnosis. It is regarded as uncommon, but it is likely that the incidence is much higher due to under-reporting [Citation3, Citation5] . In Western societies vaginal intercourse is the main cause of PF and is more likely to occur when the woman is in the superior position, when her entire weight lies on the erect penis, or in the so-called RC position, when the penis slips out of the vagina and is thrust against the perineum or pubic symphysis [Citation3, Citation6] . In Mediterranean and West African societies [Citation3] digital manipulation has been reported to account for most cases of PF. The differences have been attributed to the more liberal attitude toward sex in the West [Citation3].
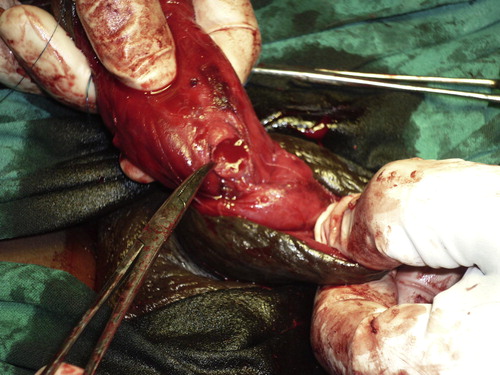
In the present review of cases seen over an 11-year period, only eight (38%) were seen within the first 9 years, while the remaining 13 (62%) were seen over the last 2 years, with 2011 accounting for nine (43%) of all cases. From a mean of 0.8 cases per year during last decade there was a four-fold increase in 2010 and an 11-fold increase in 2011. Overall, although forceful digital manipulation and sexual intercourse accounted for a similar number of cases, there was a striking difference in the pattern of distribution. Between 2000 and 2009, forceful digital manipulation of the erect penis was responsible for seven of eight cases, while in 2010–2011 sexual intercourse was responsible for 10 of 13 cases. All cases of PF during manipulation were self-inflicted except in two patients. In one the fracture occurred during a disagreement with his partner during oral sex, with the injury said to be caused by a combination of the partner’s mouth and hands. The main findings consisted of a distal tear in the tunica albuginea and some unclear skin indentations (). The second case occurred in a patient with stuttering priapism while being assisted by the partner to achieve detumescence. However, in eight of the 10 cases of PF from sexual intercourse, between 2010 and 2011, the injury occurred during coitus in the RC position. This is consistent with reports that describe an increased risk with the RC position [Citation3]. Does this indicate a change in sexual practice among Nigerian couples? This is almost impossible to prove in an environment where the open discussion of sex is still a taboo. At present we can only speculate. The rapidly changing demography of south-west Nigeria could be the key factor underlying this increase in cases of PF. With a population growth rate 10 times faster than New York and Los Angeles (arising mainly from immigration), the United Nations estimates that Lagos will become the third largest city in the world (after Bombay and Tokyo) by 2015 [Citation11]. The rapid increase in population and the increase in the cosmopolitan nature of the society are more likely to increase the number of sexual encounters, increase more liberal attitudes toward sex, and the reporting of sex-related medical problems.
What is the role of the Internet? Six of the patients with RC injuries claimed to have started RC only after watching it on the Internet, specifically on their mobile phones, even though two of them had previously seen it before in magazines. Due to the rapid growth of the global systems for mobile (GSM) communication services in Nigeria, there has been a rapid increase in the availability of almost free Internet access over the last few years. With triple-digit growth rates in subscription to GSM services, Nigeria has the largest and fastest growing number of subscribers in Africa, with Lagos alone (despite occupying only 0.4% of the surface land of Nigeria) accounting for 65% of all the commercial activities in the country [Citation12, Citation13] . While there appears to be strict regulation of the electronic and print-based media by the Nigerian Censors Board, explicit Internet content appears to be completely unregulated.
However, the relationship between PF and explicit media is more likely to be ‘casual’ rather than ‘causal’, as this increase has not been reported in other countries with similar rapid increases in Internet use.
A confident diagnosis of PF can be made based on the history and physical findings alone. A history of penile erection, application of force on the penis, cracking sound, pain, swelling and detumescence is virtually diagnostic of PF. All the present patients had these findings. Even though isolated cases of false PF have been reported we encountered none in the present study, probably because there were few patients in the present series [Citation14, Citation15] . Investigations like cavernosography, MRI and ultrasonography have also been advocated by others [Citation3, Citation16] . Only two patients in the present study were assessed with cavernosography. In one patient it gave a false-negative result. Other known limitations of cavernosography include its invasiveness, risk of priapism, allergy and penile fibrosis [Citation3]. We have abandoned its use, as it adds little to the management. Although MRI has been reported to be accurate, especially in eliminating false fractures [Citation14, Citation16] , it is very expensive, especially in a low-resource economy where patients are entirely responsible for the cost of their investigations, while ultrasonography can be unreliable in the presence of significant haematoma [Citation5].
The incidence of concomitant urethral injury has been reported to be ≈ 20%, from 0–3% in Asia and the Middle East, to 38% in Europe and North America [Citation3,Citation5,Citation17] . This discrepancy has been attributed to the greater force usually involved in post-coital injuries (PCIs) [Citation18]. However, despite the relatively large number of PCIs in the present series, there was only one case (5%) of confirmed urethral injury, in a 31-year-old man with PCI. Tan et al. [Citation19], in China, also reported a similar low incidence of urethral injury despite PCI being responsible for two-thirds of their cases. It is therefore not completely clear what predisposes the patient to urethral injury. Many authors have advocated routine urethrography, especially in patients with bleeding at the tip of the external meatus [Citation5]. However, false-negative results are not uncommon [Citation17]. The present urethral injury was discovered during exploration; the patient had no bleeding at the external meatus. We routinely did not use urethrography in any of our patients. All patients were catheterised during surgery by the urologist and there were no adverse effects.
Current evidence supports the superiority of early surgical intervention over conservative management [Citation1,Citation4,Citation5,Citation7,Citation18] . All patients (except one) who presented within 2 weeks had surgery, and they all had a satisfactory outcome. The patient who refused surgical intervention also had satisfactory erections at the follow-up assessment. While the presentation of two patients with an abnormal angulation of the erect penis at 5 and 6 months after their injuries does not conclusively confirm that surgery is better, it re-emphasises the risks associated with conservative management. Although many authors have emphasised immediate surgical repair, with reports suggesting poorer outcomes for patients operated after 36 h [Citation5], we do not stress the use of immediate surgery but operate at the first convenient moment. Most of the present patients were operated at 36–72 h after PF. Longer delays were either due to late presentation or more commonly when a patient managed conservatively after declining surgery changed his mind 1 or 2 days later. This factor, and the need to keep some patients who had travelled long distances, were the main factors responsible for the relatively long mean hospital stay. There was no difference in outcome between patients operated before 36 h or later, as they all had the same outcome. The two patients who presented at 8 and 9 days after injury also had surgical evacuation of the haematoma and tunical repair, with the same satisfactory outcome. Some other authors have also recommended the so-called ‘delayed repair’, where selected patients who present after 24 h are initially managed conservatively, to be operated 7–12 days later under local anaesthesia [Citation20].
Several incisions have been used in the management of PF, including the circumcising degloving, direct longitudinal and inguinoscrotal incisions [Citation2,Citation3,Citation5] . Each has its advantages, but we used the degloving incision because it gives unparalleled access to the three corpora. Problems reported with this incision include the patients’ dislike of the resulting penile scar, technical difficulties in the presence of severe oedema, and penile skin necrosis [Citation17]. We did not have these problems with any of the present patients. The practice of routine infantile circumcision in West Africa could be responsible for minimising both the technical difficulties associated with severe oedema and the significance of the subcoronal scar. Despite being practised by some [Citation18], we did not use drains at the operation site even in the presence of urethral injury, and neither did we use anti-erection medications to prevent disruption of the repair, as erection soon after surgery in some of the patients did not adversely affect the final outcome.
While different patterns of PF have traditionally been associated with specific geographical locations, to our knowledge this is the first study to show a clear change from one pattern to another in the same environment, highlighting the possible association between PF and rapid social changes in the society.
The present study has some limitations. There were only 21 patients, and the study was retrospective so there were no controls. The mean follow-up was also only 10 months. Difficulties with infrastructure, like effective transport, poverty and our patients’ attitudes toward follow-up, will continue to make a long-term follow-up a challenge for research in our environment.
In conclusion, with four- and 11-fold increases in the number of cases seen in 2010 and 2011, respectively, the incidence of PF appears to have rapidly increased in the authors’ environment. While earlier cases were mainly caused by forceful digital manipulation, sexual intercourse in the RC position now appears to be the predominant cause. This change has also coincided with the rapid demographic changes in Nigeria. The role of the Internet in Nigeria needs to be evaluated. Surgical intervention should be offered to patients even if there is delayed presentation.
Conflict of Interest
None.
Source of Funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- M.MuentenerS.SuterD.HauriT.SulserLong-term experience with surgical and conservative treatment of penile fractureJ Urol1722004576579
- E.M.MazarisK.LivadasD.ChalikopoulosA.BisasC.DeliveliotisA.SkolarikosPenile fractures: immediate surgical approach with a midline ventral incisionBJU Int1042009520523
- N.EkeFracture of the penisBr J Surg892002555565
- C.V.HorstF.J.PortilloA.BannowskyC.SelfK.P.JuenemannPenile fractures: controversy over surgical or conservative treatmentBJU Int922003349350
- A.F.MoreyM.J.MetroK.J.CarneyK.S.MillerK.W.McAninchConsensus on genitourinary trauma: external genitaliaBJU Int942004507515
- J.ZargooshiPenile fracture in Kermanshah, Iran. Report of 172 casesJ Urol 2000; 164: 364–366.
- W.M.GamalM.M.OsmanA.HammedyZ.M.AldahshouryM.M.HusseinM.SaleemPenile fracture: long-term results of surgical and conservative managementJ Trauma712011492493
- T.A.BadmusA.R.K.AdesunkanmiA.O.OgunrombiPenile fracture in a patient with stuttering priapismWAJM232004270273
- J.E.MensahB.MortonM.KyeiEarly surgical repair of penile fracturesGhan Med J442010119122
- G.O.SandaC.F.HeynsA.SoumanaS.RachidPenile fracture – a review of managementNiger J Surg Res82006116118
- Official website of the Lagos State Government. Available at htpp://www.lagosstate.gov.ng. Accessed 10 April 2012.
- Africa Telecommunication News. Available at http://www.africantelecomsnews.com. Accessed 3 April 2012.
- Nigeria Communication Commission. Available at http://www.ncc.ng.com. Accessed 3 April 2012.
- W.FekiA.DerouicheK.BelhajA.OuniS.Ben MouelhiM. R.Ben Slamaetal.False penile fracture. Report 16 casesInt J Impot Res 2007; 19: 471-473.
- A.El-AssmyH.S.El-TholothM.E.Abou-El-GharT.MohsenE.I.IbrahiemFalse penile fracture. The value of different diagnostic approaches and the long-term outcome of conservative surgical managementUrology75201013531357
- A.AhmadE.A.AlaaM.A.AtefA.B.MedhatM.K.I.HishamThe management of penile fracture based on clinical and magnetic resonance imaging findingsBr J Urol722005373377
- C.KamdarU.M.MooppanH.KimF.A.GulmiPenile fracture. Preoperative evaluation and surgical technique for optimal patient outcomeBJU Int102200816401644
- R.El AtatM.SfaxiM.R.BenslamaD.AmineM.AyedS.B.MouellietalFracture of the penis: management and long-term results of surgical treatment. Experience in 300 casesJ Trauma642008121125
- L.TanC.ChiangC.HuangY.ChouC.WangTraumatic rupture of the corpus cavernosumBr J Urol681991626628
- T.Abdel NasserT.MostafaDelayed surgical repair of penile fracture under local anesthesiaJ Sex Med5200824642469