Abstract
Introduction: The goal of percutaneous nephrolithotomy (PCNL) is to ensure complete stone clearance with minimal morbidity. The key to complete clearance is accurate technique, expertise and instrumentation.
Methods: We systematically reviewed available reports that were identified using a PubMed/Medline search. The keywords used were ‘PCNL’ and ‘advances in PCNL’. The findings were reviewed under the topics of newer developments in imaging, techniques and a review of outcomes with an emphasis on stone clearance and complications.
Conclusion: The newer developments in imaging methods, such as cone-beam computed tomography and staghorn morphometry, help the surgeon to plan the procedure for a safe and better outcome. The highlight of these newer developments is the miniaturisation of instruments. This has translated into developing newer techniques such as the ‘microperc’ and ‘miniperc’. The data-collection initiative by the Clinical Research Office of the Endourological Society has helped in obtaining a high level of evidence.
Introduction
The goal of percutaneous nephrolithotomy (PCNL) is to ensure complete stone clearance with minimal morbidity. The key to complete clearance is an accurate technique, and appropriate expertise and instrumentation. The technique of PCNL has developed over several years, the highlights of which were the miniaturisation of instruments and optics. This led to the development and refinement of percutaneous renal-access techniques. The newer developments include those in imaging, technique and instrumentation. The debate continues over the use of the prone or supine positions for PCNL (‘miniperc’ or standard PCNL) and tube or tubeless PCNL. Here we review the newer developments in preoperative imaging, instrumentation and access techniques related to PCNL.
Method
We systematically reviewed available reports identified using a PubMed/Medline search, using the keywords ‘PCNL’ and ‘advances in PCNL’. The articles were reviewed under the topics of newer developments in imaging, techniques and a review of the outcomes, with emphasis on stone clearance and complications.
Advances in preoperative imaging
Traditionally, conventional IVU has been the mainstay for imaging before PCNL, but recently a few studies reported the advantages of using CT as an imaging method before PCNL. Information such as the anatomy of the pelvicalyceal system and relation of the stone to the pelvicalyceal system, and insights into the three-dimensional anatomy of the renal unit, can be obtained with CT [Citation1]. A few studies showed the advantages of CT angiography for managing and treating bleeding after PCNL [Citation2].
Staghorn morphometry
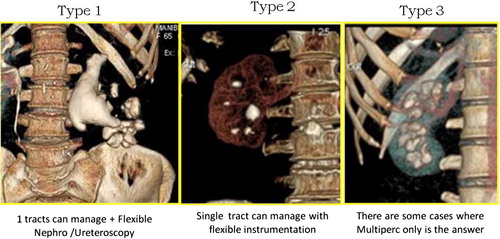
Staghorn calculi sometimes require several renal access procedures to obtain complete clearance. The stone should be cleared without increasing the morbidity. Staghorn morphometry is a new prognostic tool to predict the position of the tracts and stages for PCNL monotherapy for staghorn calculi. Staghorn morphometry requires three-dimensional CT urography assessment, obtained using volume-rendering software. The authors of a recent report [Citation3] proposed a new classification for managing staghorn calculi, which categorised staghorn calculi into three types depending on the volume of distribution of the calculus and the surface area. Type 1 staghorn stones have a total stone volume of <5000 mm3 with <5% of unfavourable calyceal stone percentile volume, whereas type 3 staghorn stones have a total volume of >20,000 mm3 with >10% of unfavourable calyceal stone percentile volume. The type 2 staghorn stone is midway between type 1 and 3 (). Based on statistical models these authors found that for achieving clearance by PCNL monotherapy, a type 1 staghorn stone would require one access tract and stage, type 2 stones would require one tract and one or more stages, or multiple tracts and one stage, and type 3 stones would require multiple tracts and stages. This study is important as it helps the surgeon to plan the treatment and to counsel the patient before surgery.
Figure 1 The three types of staghorn stone, adapted from [Citation3].
Cone-beam CT (CBCT)
CBCT has been used in neurosurgical cases and the application has been extended to percutaneous surgery. CBCT helps to assess the preoperative plan of a percutaneous procedure and simultaneously to assess the postoperative clearance. CBCT uses an imaging head similar to that of a conventional C-arm to provide high-resolution, three-dimensional, CT-like images. Roy et al. [Citation4] concluded that CBCT might provide the advantages of improved preoperative imaging, which could result in better percutaneous access and improved postoperative imaging, which allows surgeons to have ‘real-time’ access to CT-quality images.
Preoperative CT in patients at risk of colonic injury
Authors of a recent study [Citation5] suggested that patients at risk of colonic injury during PCNL should be assessed using prone CT before the procedure, as this helps in planning access sites and avoiding injury during access.
The role of CT attenuation values in determining the success of PCNL
There are many reports suggesting that stones with higher CT attenuation values (Hounsfield units) produce poor results with ESWL. In a recent retrospective study [Citation6] the authors described the outcome of PCNL, comparing it with HU as a variable. They conclude that HU values of <678 are associated with a poor outcome with PCNL. However, the study has limitations, as it had a small sample size and was retrospective.
Advances in instrumentation
Energy source
Stonebreaker
The Stonebreaker (Laryngeal Mask Airway Co., Switzerland; distributed by Cook Medical, Bloomington, IN, USA), is a hand-held pneumatic lithotripter. The device is powered by a self-contained compressed carbon-dioxide cartridge. The device is also activated by a hand switch rather than a foot switch, which further eliminates trailing cords in the operating theatre. The Stonebreaker delivers 3.1 MPa to the stone via the treatment probe, compared with 0.3 MPa from pneumatic lithotripters. In a study comparing the Stonebreaker with the Swiss Lithoclast, the authors found that the Stonebreaker is easier to set up and is user-friendly, and provides faster stone fragmentation than the Swiss Lithoclast [Citation7].
Cyberwand
This new tool by Gyrus ACMI (Southborough, MA, USA, now part of the Olympus Corp., Japan) is a dual ultrasonic lithotripter. As the two probes vibrate at different rates it produces a synergistic effect. The inner probe vibrates at a frequency of 21,000 Hz while the outer probe vibrates at 1000 Hz. The inner probe protrudes beyond the outer probe, and both are controlled with a single foot pedal. There are few reports describing the clinical outcome of this device [Citation8].
Access methods
Previously, various methods, such as robotic percutaneous access to the kidney (‘PAKY’), have been devised to gain accurate access to the kidney. A recent report [Citation9] described a ‘locator’, a device for gaining accurate percutaneous access. The device stabilises the needle for PCNL puncture, relying on an adjustable and lockable multidirectional head that is securely fixed to the operating table. The radiolucent head holds a 10 F metal guide that allows puncture of the renal collecting system. The needle system uses the traditional fluoroscopic ‘bull’s-eye sign’ to achieve precise and fixed alignment. An objective assessment was obtained by in vitro testing using a simulated PCNL puncture with and without using the locator. The time to successful puncture and the fluoroscopy screening time were assessed. The Locator is a simple, cheap and novel ‘assistant’ for achieving successful PCNL puncture. Preliminary in vitro testing suggests that the device might reduce fluoroscopy exposure and be quicker.
New techniques
Micro PCNL (‘microperc’)
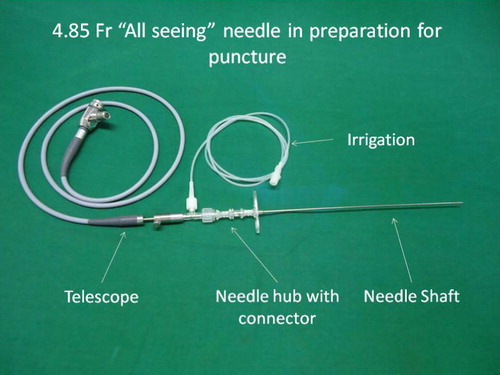
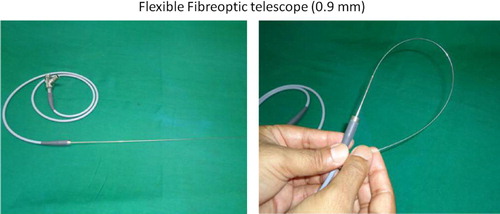
A major aim of development and innovation is to reduce the tract size, as this decreases the morbidity, as confirmed by several studies [Citation10,Citation11]. Bader et al. [Citation12] reported their experience with a micro-optical system inserted through a specific puncture needle to confirm the location of the chosen access before dilatation of the operating tract. The basis for developing this system was that a suboptimal access hampers or can even lead to abandoning the procedure. Micro-optics of 0.9 and 0.6 mm in diameter were used. The micro-optic with an integrated light head was inserted through the working sheath of the puncture needle. The modified needle had a 1.6-mm (4.85 F) outer diameter. The optical fibre was connected via a zoom ocular and light adapter to a standard endoscopic camera system. Adequate vision was ensured with an irrigation system. The optical assessment included measurements of the distortion, resolution, angle and field of view. The authors concluded that the optical puncture needle for PCNL appears to be helpful for confirming percutaneous access before dilatation of the nephrostomy tract, thus potentially increasing the safety margin. Desai et al. [Citation13] further developed this concept and completed the procedure through the ‘all seeing needle’. The working hypothesis of the ‘all-seeing needle’ is that if the initial tract is perfect then the tract-related morbidity could be reduced. The optical needle helps to avoid visceral injury and confirms the access using visual cues. The other advantage of the microperc is that it is a single-step renal access procedure, resulting in a shorter insertion-to-lithotripsy time. The assembly and instrumentation for the microperc procedure is as shown in and .
If ultrasonography is selected to direct the access, the microneedle assembly is engaged in the puncture guide; in this technique the surgeon, apart from having a real-time trajectory of the needle on the electronic ‘dotted line’, can also assess the path of the needle as it passes through the subcutaneous tissue, thoracolumbar fascia and into the desired calyx. The key to successfully completing the procedure is that the access should not deviate from the desired calyx, as the manoeuvrability of the needle is limited.
Desai et al. [Citation13] investigated the feasibility of the microperc technique The mean stone size was 14.3 mm, and of the 10 patients, two were children, and each one had an ectopic pelvic kidney, chronic kidney disease and obesity. The microperc was feasible in all patients, with a mean (SD) haemoglobin decrease of 1.4 (1.0) g/dL and a hospital stay of 2.3 (1.2) days. Nine patients were stone-free at 1 month. In one patient intraoperative bleeding obscured vision and this required conversion to a mini-PCNL (‘miniperc’). There were no postoperative complications and no auxiliary procedures were required.
Endoscopically guided PCNL
Previously the Lawson retrograde access system was used for gaining retrograde percutaneous access. In this way the percutaneous tract was created ‘through and through’ (urethra–ureter–kidney–skin). The original technique and its subsequent modifications were reported to have a success rate of 89–100%. The limitations of this method of gaining access included the inability to bypass an impacted stone and the creation of a long percutaneous tract which was not straight. The natural extension of this technique is the use of a flexible ureteroscope to assist in gaining access.
Endoscopy-assisted percutaneous renal access was first successfully reported as a salvage procedure by Grasso et al. [Citation14]. They used this technique as a method of gaining access in a few patients in which other methods failed. The University of Irvine group developed this technique as a primary access method for all cases. The insertion of the nephrostomy needle into the collecting system is monitored under both fluoroscopy and direct ureteroscopic vision. The guidewire can be passed into the access sheath, where it can then be delivered via the urethral end of the access sheath [Citation15]. As proper access is the key to successfully completing the procedure, the direct visual confirmation of the access ensures that the needle and guidewire are in the correct position.
iPad-guided percutaneous renal access
In iPad-assisted navigation, three-dimensional ‘augmented virtual reality’ can display all the relevant anatomical details. The advantage is that there is no limited vision, as with ultrasonography (shadows caused by ribs). The easy freehand needle placement without holding the ultrasound probe is helpful. It is important that the iPad displays images of the operation site, so the surgeon can see his or her hands. The iPad is used as a camera to take a picture of the patient’s skin, and with compressed capture of the data this data is transferred to a wireless local area network (e.g., WiFi) to a server located in a control room. The server runs the algorithm to identify the position and orientation of the navigation, and to overlay it accordingly with preoperative segmented CT images, which are sent back to the iPad. The exact overlay of real and virtual markers allows a ‘virtual insight’ into the patient and thus gain access [Citation16].
Literature review on PCNL
Clinical Research Office of the Endourological Society (CROES) is instrumental in acquiring and analysing worldwide data for PCNL. Thus it provides a platform for analysing the trends in indications, technique and outcomes of PCNL in many high-volume centres [Citation17]. Reports have been diverse with regard to the indications, treatment outcome and complication rates for PCNL worldwide. CROES collected prospective data for consecutive patients who were treated with PCNL at centres around the world for 1 year. Between November 2007 and December 2009, 5803 patients were treated at 96 centres in Europe, Asia, North America, South America and Australia. Staghorn calculi were present in 1466 (27.5%) patients, and 940, 956 and 2603 patients had stones in the upper, interpolar and lower pole calyces, respectively. Most procedures (85.5%) were uneventful. Major procedure-related complications included significant bleeding (7.8%), renal pelvic perforation (3.4%), and hydrothorax (1.8%). A blood transfusion was administered in 328 (5.7%) patients, and a fever of >38.5C occurred in 10.5% of the patients. The distribution of scores in modified Clavien grades was: no complication (79.5%), I (11.1%), II (5.3%), IIIa (2.3%), IIIb (1.3%), IVa (0.3%), IVb (0.2%), or V (0.03%). At the follow-up the 30-day stone-free rate was 75.7%, and 84.5% of the patients needed no additional treatment [Citation17].
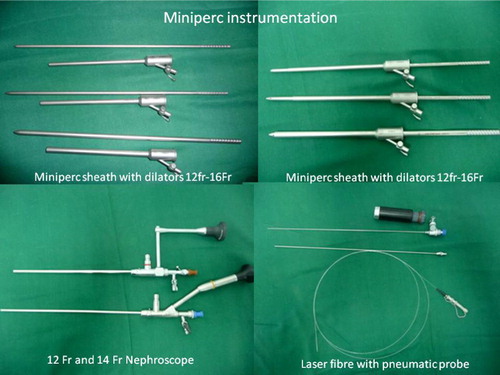
Miniperc and standard PCNL
The miniperc can be defined as a percutaneous procedure with a tract size of <18 F. Recent minipercs are performed with a nephroscope sheath of 12–16 F, with a metal dilator (). The indications for a miniperc, retrograde intrarenal surgery (RIRS) and ESWL overlap. RIRS is commonly used for treating non-bulky renal urolithiasis. Both RIRS and the miniperc are invasive and are associated with inherent complications. Similarly, opinions on the utility of the miniperc compared with standard PCNL are divided. A retrospective study [Citation18] failed to show significant advantages of the Miniperc technique, but two randomised controlled trials [Citation19,Citation20] comparing miniperc with RIRS and the other comparing miniperc with standard PCNL showed that the miniperc has a role. Both RIRS and the miniperc were effective in rendering patients stone-free with minimal complications [Citation19]. The immediate stone-free rate was higher with the miniperc but comparable in both methods at 1 month. RIRS was associated with favourable pain scores and a lower decrease in haemoglobin levels. The miniperc and RIRS had stone clearance rates of 100% and 96.9%, respectively. The patients’ pain and visual analogue scale scores (each P < 0.001) at 6, 24 and 48 h, and the analgesic requirement (P < 0.003), were all lower in the RIRS group.
In another study by the same group [Citation20] they evaluated the results of miniperc vs standard PCNL for stones of 1–2 cm. The authors showed that the miniperc might be a reasonable procedure in patients with non-bulky urolithiasis, offering a similar outcome to standard PCNL, with the advantage of reduced morbidity. This study showed significant advantages of the miniperc in terms of reduced bleeding, leading to a tubeless procedure and reduced hospital stay. The stone-free rates and the complications were similar in both groups [Citation20].
Patient positioning
Traditional PCNL is performed with the patient prone, but recently several reports have described the utility of various alternative positions for PCNL. The various positions described include the Valdivia, modified Valdivia, flank position and completely supine position. The incidence of complications decreases if the patient position is optimised [Citation21].
In a recent review by Kumar et al. [Citation22] various modifications of the supine position were assessed and the advantages and disadvantages of each discussed. The obvious advantages of a supine position are that there is no need to change the position of the patient, the ability to perform simultaneous ureteroscopy, the ease of airway control for the anaesthetist, easier evacuation of fragmented stones because of the position of the Amplatz sheath, a lower chance of colonic injury, and finally it is more suitable for obese patients and those with respiratory and cardiac compromise alike [Citation23]. Falhatkar et al. [Citation24] recently reported the utility of a completely supine position. The authors stated that the potential advantages of this position are less patient handling, easier access of the urethra, an easier change to general or spinal anaesthesia, and a better control of the airway. A group from Iran described a flank position [Citation25]; in a comparative study of the prone, supine and flank positions, 150 patients were randomised into either group. The comparison showed that the supine and flank positions were as safe and effective as the prone position in experienced hands. They also concluded that the preference of the surgeon and proper case selection are the ‘key’ to success.
Conclusion
The newer developments in imaging methods, such as CBCT and staghorn morphometry, can help the surgeon to plan the procedure for safer and better outcomes. The highlight of these newer developments is the miniaturisation of instruments. This has translated into the development of newer techniques such as the microperc and miniperc. The data collection initiative by CROES has helped to obtain a high level of evidence.
Conflict of interest
There is no conflict of interest.
Source of funding
No source of funding.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- K.R.GhaniU.PatelK.AnsonComputed tomography for percutaneous renal accessJ Endourol23200916331639
- S.SivanandumM.GearogeS.BhatEmerging role of multi-detector computed tomography in the diagnosis of hematuria following percutaneous nephrolithotomy: a case scenarioIndian J Urol252009392394
- S.MishraR.B.SabnisDesai MR percutaneous nephrolithotomy monotherapy for staghorn: paradigm shift for ‘staghorn morphometry’ based clinical classificationCurr Opin Urol222012148153
- O.P.RoyJ.F.AngleA.D.JenkinsN.S.SchenkmanCone beam computed tomography for percutaneous nephrolithotomy: initial evaluation of a new technologyJ Endourol262012814818
- V.ChalasaniD.BissoonA.K.BhuvanagirA.MizziI.B.DunnShould PCNL patients have a CT in the prone position preoperatively?Can J Urol17201050825086
- A.GücükU.UyetürkU.OztürkE.KemahliM.YildizA.MetinDoes the Hounsfield unit value determined by computed tomography predict the outcome of percutaneous nephrolithotomy?J Endourol262012792796
- B.H.ChewO.ArsovskaD.LangeJ.E.WrightD.T.BeikoD.GhiculeteetalThe Canadian StoneBreaker trial. A randomized, multicenter trial comparing the LMA StoneBreaker™ and the Swiss LithoClast® during percutaneous nephrolithotripsyJ Endourol25201114151419
- Joseph W.PughBenjamin K.CanalesNew instrumentation in percutaneous nephrolithotomyIndian J Urol262010389394
- J.LazarusJ.WilliamsThe locator: novel percutaneous nephrolithotomy apparatus to aid collecting system puncture–a preliminary reportJ Endourol252011747750
- R.KukrejaM.DesaiS.PatelS.BapatM.DesaiFactors affecting blood loss during percutaneous nephrolithotomy: prospective studyJ Endourol182004715722
- M.R.DesaiP.JainA.P.GanpuleR.SabnisS.PatelP.ShrivastavDevelopments in technique and technology: the effect on the results of percutaneous nephrolithotomy for staghorn calculiBJU Int1042009542548
- M.J.BaderC.GratzkeM.SeitzR.SharmaC.G.StiefM.DesaiThe ‘all-seeing needle’. Initial results of an optical puncture system confirming access in percutaneous nephrolithotomyEur Urol59201110541059
- M.R.DesaiR.SharmaS.MishraR.B.SabnisC.StiefM.BaderSingle-step percutaneous nephrolithotomy (microperc): the initial clinical reportJ Urol1862011140145
- M.GrassoG.LangF.C.TaylorFlexible ureteroscopically assisted percutaneous renal accessTech Urol119953943
- P.G.SountoulidesO.G.KaufmannM.K.LouieS.BeckN.JainA.KaplanetalEndoscopy-guided percutaneous nephrostolithotomy. Benefits of ureteroscopic access and therapyJ Endourol23200916491654
- J.RassweillerM.MullerM.FangereauJ.KleinA.S.GoezenP.PereiraetalIPad-assisted percutaneous access to the kidney using marker-based navigationEur Urol62012e13e22
- J.de la RosetteD.AssimosM.DesaiJ.GutierrezJ.LingemanR.ScarpaetalCROES PCNL study group. The clinical research office of the endourological society percutaneous nephrolithotomy global study. Indications, complications, and outcomes in 5803 patientsJ Endourol2520111117
- G.GiustiA.PiccinelliG.TavernaA.BenettiL.PasiniM.CorintietalMiniperc? No, thank you!Eur Urol512007810814
- R.B.SabnisJ.JagtapS.MishraM.DesaiTreating renal calculi 1–2 cm in diameter with minipercutaneous or retrograde intrarenal surgery: a prospective comparative studyBJU Int2012 [Epub ahead of pub]
- S.MishraR.SharmaC.GargA.KurienR.SabnisM.DesaiProspective comparative study of miniperc and standard PNL for treatment of 1–2 cm size renal stoneBJU Int1082011896899
- A.PapatsorisJ.MasoodT.El-HusseinyZ.MaanP.SaundersN.P.BuchholzImproving patient positioning to reduce complications in prone percutaneous nephrolithotomyJ Endourol232009831832
- P.KumarC.BachS.KachrilasG.AthanasiosN.Papatsoris BuchholzJ.MasoodSupine percutaneous nephrolithotomy (PCNL). ‘In vogue’ but in which position?BJU Int2012 [Epub ahead of pub]
- S.FalahatkarA.AllahkhahS.SoltanipourSupine percutaneous nephrolithotomy: proUrol J82011257264
- S.FalhatkarM.M.AsliS.A.EmadiA.EnshaeiH.PourhadiA.AllahkhahComplete supine percutaneous nephrolithotomy in patients with and without a history of stone surgery: safety and effectiveness of complete supine PCNLUrol Res392011295301
- H.KaramiR.MohammadiB.LotfiA study on comparative outcomes of percutaneous nephrolithotomy in pprone, supine and flank positionsWorld J Urol2012 [Epub ahead of print]