Abstract
Objectives:
To develop a new and inexpensive model for training in fluoroscopic puncture into the pelvicalyceal system, and to use this model to compare the learning curve of two fluoroscopic techniques, the ‘eye of the needle’ (EN) and triangulation techniques.
Materials and methods:
For the trial we used a commercial plastic model (a shop-window mannequin) in which a bovine kidney, embedded in sponge with a spatial orientation similar to the human, was inserted into the model. The ureter of the animal kidney was connected to contrast fluid. Ten residents and interns were randomised into two groups; group A started the puncture using the EN technique, each member making five attempts, and then five attempts using the triangulation technique, and group B started with triangulation and then used the EN technique.
Results:
There was no statistically significant difference between the techniques for the mean (SD) number of trials to make a correct puncture, at 2.68 (1.00) in the EN technique and 2.86 (1.05) in the triangulation technique, or for the duration of each trial, at 523 (189) s for the EN technique and 578 (175) s for the triangulation technique. The fluoroscopy time was less in the EN technique, at 113.9 (48.9) s than for the triangulation method, at 135.8 (42.4) (P < 0.005).
Conclusions:
The model was easy to construct and feasible for training. Both techniques had a similar learning curve, with higher fluoroscopy exposure for the triangulation technique.
Introduction
The role of percutaneous renal procedures in urology is expanding to cover several domains. Percutaneous nephrolithotomy (PCNL) is the method of choice for stones of > 2 cm, and percutaneous access is also used for endopyelotomy and the management of renal TCC [Citation1,Citation2]. Overall there is increasing use of PCNL, especially for complex stones, staghorn and lower-pole stones [Citation3,Citation4].
Making a puncture is the first step in PCNL and can be described as the key step for any percutaneous procedure. Complications associated with a faulty puncture include failure to complete the procedure, obtaining less than optimal access (making the procedure more difficult), bleeding, and injury to the surrounding structures [Citation5].
The puncture can be done either by a urologist or by a radiologist, with similar complications and stone-free rates, but when urologists alone make the access they tend to manage more complex stones and use several and supracostal punctures more often than do radiologists [Citation6].
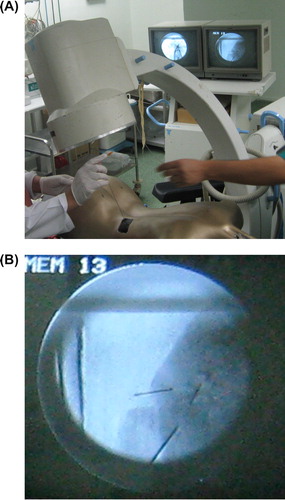
Two techniques are commonly used to insert the puncture needle into the collecting system, i.e. the ‘eye of the needle’ (EN) technique and the triangulation technique. In the latter ( and ), the targeted calyx is identified, a C-arm is positioned parallel to the line of the puncture (position A) then the C-arm is turned obliquely (cephalo-caudal) 30° to this line (position B). In position A the needle is adjusted mediolaterally, and in position B adjustments are made up and down, with careful monitoring to ensure the same orientation as the mediolateral position of the needle [Citation7].
Figure 1 (A) An anteroposterior puncture in the triangulation technique, with the C-arm in position B; (B) a fluoroscopic image showing two syringe tips marking the targeted calyx, with the C-arm in position A and B, with the puncture seen in the horizontal plane.
The EN technique () entails aligning the desired calyx, the tip of the needle, the hub of the needle and the axis of the X-ray beam. This gives a ‘bull’s eye’ effect. The needle is then advanced and the depth is controlled using a lateral C-arm view [Citation7].
The learning curve for PCNL is not yet clearly defined; Two reports of a single-surgeon experience suggested that proficiency in PCNL is obtained after 60 cases [Citation8,Citation9]. A survey from the USA showed that a urologist trained on PCNL during their residency undertook more PCNLs after that residency and was more comfortable doing PCNL. The authors suggested that residents should perform >24 PCNLs during their residency [Citation10].
Despite the steep learning curve of PCNL and potentially grave complications for such a procedure there is a paucity of training models and simulators [Citation11]. The devised models can be generally categorised into three types: (1) Computer-based virtual environments like the inanimate and virtual-reality simulators [Citation12]; (2) Biologically based models like an infused porcine kidney in a chicken carcass [Citation13]; and (3) using a thin-slice CT image to create a patient-specific three-dimensional model of the kidney, and then using a rapid prototyping machine to produce a silicon model for the kidney [Citation14].
McDougall et al. [Citation15] proposed several definitions (face validity, content validity, construct validity and criterion validity) to allow objective judgements of surgical training models. In brief, ‘face validity’ is a measure of the opinion of non-experts about the simulator, ‘content validity’ the opinion of experts about the simulator, ‘construct validity’ is the ability of the simulator to distinguish between different levels of experience, measured within one trainee over time or between groups of trainees. The criterion validity is the predictive validity correlation of trainees’ performance on the model with operating-room performance.
In the present study we aimed to develop a new and inexpensive model for training in fluoroscopic puncture into the pelvicalyceal system, then to use the model to compare the learning curve of two fluoroscopic techniques of pelvicalyceal puncture (EN and triangulation).
Materials and methods
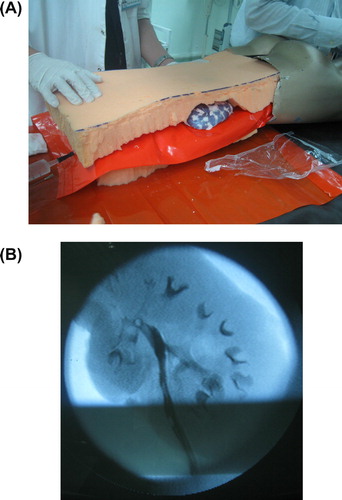
The study was approved by the ethics committee of our hospital. We started with a commercial model (a mannequin) of the kind used in clothing-shop windows. We chose one with dimensions and curves similar to the average person, into which was placed a kidney from a freshly slaughtered cow. The ureter, renal artery and vein were identified, and the kidney was flushed with cold normal saline until the efflux from the renal vein was clear (). We then used two sheets of sponge to cover the kidney and placed it inside the mannequin, keeping it as close as possible to the normal kidney orientation and position. A window was created in the model where the needle puncture should start and part of an aubergine (eggplant, Solanum melongena) was used to mimic the human cuticle. The model was then checked under fluoroscopy for the integrity of the pelvicalyceal system, and the correct position of the whole kidney was ascertained ( and ).
A group of five residents and five interns volunteered to participate in the study. They had no experience of PCNL (none of them had participated in PCNL or made a fluoroscopy-guided puncture). The 10 participants were randomised into two groups, A and B, by selecting a folded paper from a container of 10 folded papers with five marked group A and five group B.
After a detailed presentation of both techniques by two of the authors who had extensive experience of PCNL, one of them using the triangulation technique primarily and the other the EN method primarily. Each presented his method and stayed as a guide and mentor during the study.
Group A started by using the triangulation technique, with each member making five punctures of the pelvicalyceal system, and then five punctures using the EN technique. Then group B started by making five punctures to the pelvicalyceal system using the EN technique, followed by five with the triangulation technique. The two groups were not together during the study. We measured the number of trials until there was a correct puncture, and the total fluoroscopy time and total time for each trial.
After finishing the two training sessions the participants answered a simple questionnaire developed by the authors, the questions being: (1) Do you feel this training session is useful?; (2) Does it improve your understanding of fluoroscopically guided puncture?; (3) Do you think this session will be reflected in your training on PCNL? The only answers allowed were ‘yes’ or ‘no’.
After accumulating data from the two techniques from both groups, the Kruskal–Wallis test and Spearman’s correlation were used to assess the results, with P < 0.05 taken to indicate significant differences.
Results
Overall the model was easy to construct, inexpensive and allowed trainees to practice the two methods of PCNL puncture. Each cow’s kidney allowed a mean of 20 punctures in different calyces. All the trainees reported satisfaction in the anonymous questionnaire completed after the trial.
The performance of the two groups was compared after combining the results of the trials in both techniques; there were no statistically significant difference between the groups for all three measurements ().
Table 1 The comparison between the groups and between the techniques.
To compare the EN and triangulation techniques we combined measurements from the two groups. There was no statistically significant difference between the techniques for either the number of punctures needed for correct access to the targeted calyx or the total time (). The mean fluoroscopy time was shorter for the EN technique (P = 0.01).
To show the effect of gaining experience in one technique when using the other we compared the three measurements for each of the techniques between the two groups. There were no statistically significant differences in the three measurements in the triangulation technique (), but comparing the two groups for the EN technique, group A (which started with triangulation) had shorter mean total and fluoroscopy times for each puncture than had group B (). There was an improvement in the three measurements with repeated trials in the two techniques. Spearman’s correlation test for the correlation between the number of trials and the study measurements is also shown in . The questionnaire showed that all participants answered the three questions with ‘Yes’.
Discussion
The ideal training model should resemble the actual procedure in almost every aspect, be able to show the progress of trainees during training, and facilitate translation of the skills as improved performance in real cases.
Construction of the present model was simple, as the fresh cow kidneys are inexpensive and the pelvicalyceal system is similar to that of the human to a great extent.
This model fulfilled face validity, but the content validity, construct validity and criterion validity could not be confirmed for this model [Citation15].
The use of the eggplant cuticle gives the texture of human skin, and the use of shop-window mannequin allowed the kidney to be orientated in the space similar to that in the human. The orientation was better than that used by Earp [Citation16], where a sheet of foam was used to resemble the human body. The catheter attached to the ureter allowed the kidneys to be flushed with contrast material, to facilitate fluoroscopy. The advantage of the fresh cow kidney was that it allowed many punctures with no extravasation of the dye. This model is easy to construct and reassemble. It can be used to simulate both supine and prone PCNL.
The use of a biological model has advantages over computer-based models in that it provides a feedback sensation of different tissue resistance [Citation12]. Our model was better than that of Hacker et al. [Citation13], who used a porcine kidney in a chicken carcass, as it provided a greater appreciation of the kidney position in relation to the human body.
In the present study the mean fluoroscopy time was shorter in the EN technique, but there was no statistically significant difference between the techniques for either the number of punctures or the total time. However, in a clinical setting, Tepeler et al. [Citation17], comparing 40 patients undergoing PCNL for a simple renal stone using the EN technique with 40 using triangulation, found no statistically significant difference in fluoroscopy time and operative duration between the techniques.
We acknowledge that this model has several limitations. It was not designed to allow a complete PCNL procedure, including dilatation and stone extraction. The complications of PCNL cannot be reproduced, e.g., bleeding, or injury to adjacent organs. Also, this model allowed only fluoroscopically guided but not ultrasonically guided puncture. The study had relatively few participants which increased the α error. We hope that further studies can have more participants with better designed models.
In conclusion, the present model was inexpensive, easy to construct, and had face validity. Both the EN and triangulation techniques can be done easily in the model, with improved performance while training. When comparing both methods, there were no differences in total time and the number of punctures, but the EN technique was associated with a shorter fluoroscopy time.
Conflict of interest
None.
Funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- B.E.KnudsenA.J.CookJ.D.WattersonD.T.BeikoL.NottH.Razviet alPercutaneous antegrade endopyelotomy: long-term results from one institutionUrology632004230234
- R.H.ThompsonA.E.KrambeckC.M.LohseD.S.ElliottD.E.PattersonM.L.BluteEndoscopic management of upper tract transitional cell carcinoma in patients with normal contralateral kidneysUrology712008713717
- A.R.El-NahasI.ErakyA.A.Shokeiret alPercutaneous nephrolithotomy for treating staghorn stones: 10 years of experience of a tertiary-care centreArab J Urol102012324329
- D.S.MorrisD.A.TaubJ.T.WeiR.L.DunnJ.S.WolfJr.B.K.HollenbeckRegionalization of percutaneous nephrolithotomy: evidence for the increasing burden of care on tertiary centersJ Urol1762006242246
- M.S.MichelL.TrojanJ.J.RassweilerComplications in percutaneous nephrolithotomyEur Urol512007899906
- A.M.El-AssmyA.A.ShokeirT.MohsenN.El-TabeyA.R.El-NahasA.M.Shomaet alRenal access by urologist or radiologist for percutaneous nephrolithotomy–is it still an issue?J Urol1782007916920
- N.L.MillerB.R.MatlagaJ.E.LingemanTechniques for fluoroscopic percutaneous renal accessJ Urol17820071523
- D.AllenT.O’BrienR.TiptaftJ.GlassDefining the learning curve for percutaneous nephrolithotomyJ Endourol192005279282
- O.TanriverdiU.BoyluM.KendirciM.KadihasanogluK.HorasanliC.MirogluThe learning curve in the training of percutaneous nephrolithotomyEur Urol522007206211
- C.L.LeeJ.K.AndersonM.MongaResidency training in percutaneous renal access: does it affect urological practice?J Urol1712004592595
- J.J.de la RosetteM.P.LagunaJ.J.RassweilerP.ConortTraining in percutaneous nephrolithotomy – a critical reviewEur Urol5420089941001
- M.P.LagunaM.HatzingerJ.RassweilerSimulators and endourological trainingCurr Opin Urol122002209215
- A.HackerG.Wendt-NordahlP.HoneckM.S.MichelP.AlkenT.KnollA biological model to teach percutaneous nephrolithotomy technique with ultrasound- and fluoroscopy-guided accessJ Endourol212007545550
- F.BruyereC.LerouxL.BrunereauP.LermusiauxRapid prototyping model for percutaneous nephrolithotomy trainingJ Endourol2220089196
- E.M.McDougallValidation of surgical simulatorsJ Endourol212007244247
- P.P.EarpPercutaneous renal surgery – new model for learning and trainingInt Braz J Urol292003151154
- A.TepelerA.ArmaganT.AkmanE.C.PolatC.ErsözR.Topaktaset alImpact of percutaneous renal access technique on outcomes of percutaneous nephrolithotomyJ Endourol262004828833