Abstract
Objectives:
To review our 10-year experience with uncommon testicular tumours in children (prepubertal testicular and paratesticular), to review previous reports, and to determine the appropriate management of these rare tumours, specifically the role of testicular-sparing surgery.
Patients and methods:
We retrospectively reviewed all cases of testicular tumours managed at our institution between 1999 and 2009. Boys aged <16 years were included in the study. The patients’ characteristics, presentation, the diagnostic tools, tumour markers, mode of treatment, pathological findings and outcome were assessed. We reviewed previous reports that addressed testicular and paratesticular tumours in prepubertal boys, using a Medline/PubMed search.
Results:
From 80 patients, 13 boys (median age 8.7 years) presented with testicular tumours (16%) and were included in the study. Two boys presented with precocious puberty and one with gynaecomastia. The level of α-fetoprotein was high in three boys, and the human chorionic gonadotrophin level was elevated in one, and both markers were high in one. Testicular-sparing surgery was performed in three boys. Six of the 13 tumours were malignant and seven were benign. None of the patients developed a recurrence or testicular atrophy after testicular-sparing surgery. From the review of previous reports we devised an evidence-based algorithm for managing prepubertal testicular tumours.
Conclusions:
Paediatric testicular tumours are rare but they require an inguinal approach for either orchidectomy or testicular-sparing surgery; we recommend the latter option as long as frozen sections are analysed and a safety margin is maintained.
Keywords:
Introduction
Testicular and paratesticular tumours in children are uncommon, representing 1–2% of all paediatric solid tumours and 3% of all testicular tumours. They occur with an incidence of 0.5–2 per 100,000 children [Citation1]. Historically, yolk-sac tumour has been described as the most common lesion in children, followed by teratoma [Citation2,Citation3]. However, recent studies reported that benign testicular lesions are more common in this age group [Citation4–Citation7]. Traditionally, a radical high inguinal orchidectomy is the treatment of choice, but there are studies reporting the successful management of a benign lesion with a testicular-sparing approach, and with encouraging results in the long-term follow up [Citation4,Citation6].
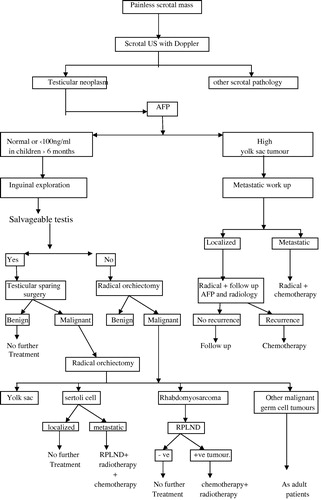
We reviewed our 10-year experience with testicular tumours in children and adolescents, and reviewed previous reports to devise an algorithm for managing prepubertal testicular tumours.
Patients and methods
After obtaining internal review board and ethics committee approval, the computerised files of patients who were treated for testicular tumours in our institute between January 1999 and December 2009 were reviewed. Only patients aged ⩽16 years were included in the study and their files were fully evaluated. The data collected were age at the time of surgery, medical history, surgical history, clinical manifestations, diagnostic tools, tumour marker levels, tumour characteristics, treatment methods, histopathological findings and the outcome. Testicular ultrasonography (US) and tumour marker levels were assessed in all patients. CT of the chest, abdomen and pelvis, and MRI, were used in patients with a suspected malignancy and associated metastasis.
Surgery
All patients were explored via an inguinal incision, with early control of the spermatic cord at the internal inguinal ring. The testis was retrieved through the incision and then the tunica vaginalis was incised. If the tumour had invaded the whole testis, a radical orchidectomy was done. If the tumour was well demarcated it was excised and sent for frozen-section analysis. If confirmed to be a benign tumour then testicular-sparing surgery was used, but otherwise a radical orchidectomy was done. All tumours excised were sent for histopathological examination after surgery.
Follow-up data were collected from the clinical visit registry. Patients were followed up by a clinical examination and US, and measurement of the serum α-fetoprotein (AFP) level. A follow-up CT and chest X-ray were assessed in patients with malignant tumours.
Previous reports in English were identified using a Medline/PubMed search that addressed testicular and/or paratesticular neoplasms in prepubertal males. Using these data and our experience, we devised an evidence-based concise algorithm for managing these uncommon tumours.
Results
Among 80 patients with testicular tumours only 13 were diagnosed in children (median age 8.7 years, range 0.33–16). The tumours affected the right and left testis in seven and six patients, respectively. A painless testicular swelling was the main presenting symptom in 10 patients, with precocious puberty as the presenting symptom in two patients with a Leydig-cell tumour. A patient with a Sertoli-cell tumour presented with gynaecomastia. Tumour markers were assessed in all patients and the results are shown in .
Table 1 The correlation between tumour marker levels and the pathology of the testicular tumour.
Scrotal US with a Doppler study was used in all patients, and detected all the testicular and paratesticular lesions (sensitivity 100%). CT of the abdomen and pelvis was used in one patient with high levels of both AFP and human chorionic gonadotrophin (HCG), and this detected retroperitoneal lymphadenopathy. MRI was used in two patients with elevated AFP levels, but no extra-testicular lesions were detected.
US showed well-circumscribed intratesticular lesions with a low blood flow on the Doppler study in two patients. They were treated by testicular-sparing surgery after frozen-section analysis, and the pathology was Leydig-cell tumour and Leydig-cell hyperplasia (). Also, a diffuse enlargement of the right testis with an intratesticular hyperechoic area was detected in a 10-year-old boy. Doppler US showed a normal blood flow. The patient was explored for any possible malignant tumour. On exploration, the right testis was large, with normal intrascrotal structures. The tunica albuginea was opened and an intratesticular small well-defined whitish mass was excised. This was confirmed to be benign macro-orchidism. No patient developed a recurrence or testicular atrophy at the last follow-up (24, 28 and 20 months, respectively).
Ten patients were treated by radical orchidectomy as the testis could not be saved, or the frozen-section analysis confirmed malignancy. Three were yolk-sac tumours, one was a seminoma, one a mixed germ-cell tumour, two were Sertoli-cell tumours, and one each a Leydig-cell tumour, embryonal rhabdomyosarcoma and capillary haemangioma ().
Table 2 The clinical characteristics and management of the various prepubertal testicular tumours.
Six of the 13 patients had malignant tumours; five had stage I tumours with no extra-testicular lesions. Only the patient with a mixed germ-cell tumour had retroperitoneal lymphadenopathy of ⩽2 cm (stage II). He received adjuvant chemotherapy and was free of disease at the last follow-up.
Patients with benign lesions were not recommended for a close follow-up. Only those patients with endocrine manifestations were referred to a special paediatric endocrinologist. Patients with malignant pathology were followed up at the outpatient clinic, and all were alive with no recurrence or metastasis at a median follow-up of 22.5 months. The levels of tumour markers returned to normal values after surgery in all cases except in the patient with a mixed germ-cell tumour, where marker levels returned to normal values after adjuvant chemotherapy.
Discussion
These rare prepubertal testicular and paratesticular tumours are distinct from those in adults. The incidence of prepubertal testicular tumours has not increased significantly over the last three decades, but the incidence has increased in postpubertal populations [Citation2]. Testicular tumours have a bimodal age distribution, occurring in young adults, and with a distinct peak in the first 3 years of life, but with a much lower incidence than in adults [Citation12].
The commonest type of prepubertal testicular tumour is the malignant yolk-sac tumour, followed by teratoma [Citation2]. Furthermore, the 30-year data from one centre in Turkey showed that yolk-sac tumour is the most common type [Citation3]. Analysis of data from four paediatric centres in the USA showed a much higher proportion of teratoma, in half of cases [Citation5]. Similar results were reported from several single institutions [Citation4,Citation6,Citation7]. Regardless of the actual distribution, yolk-sac tumours and teratomas are the most common prepubertal testicular tumours, but most postpubertal testicular tumours are malignant germ-cell tumours (seminomas). In the present series malignant tumours comprised about half and no cases of teratoma were diagnosed.
A painless scrotal swelling is the main symptom in 85–90% of cases, followed by an incidental diagnosis after trauma, or with hydrocele or hernia [Citation4]. In the present study three-quarters of patients presented with a painless mass. Consistent with other reports, scrotal US with a Doppler study distinguished intratesticular masses from extratesticular masses and other scrotal pathologies, with complete sensitivity [Citation12,Citation13].
A metastatic evaluation using CT and/or MRI of the abdomen, pelvis and chest is used only if there is a high risk of metastasis, to determine the preoperative staging and plan for therapy. It is indicated in two conditions: First, in a patient aged >6 months with high AFP levels, as this suggests a yolk-sac tumour with a high risk of metastasis to lung or retroperitoneum. The second condition is a confirmed malignant histological diagnosis [Citation14]. In the present series the metastatic evaluation was preoperative in three patients with elevated tumour marker levels, and retroperitoneal lymphadenopathy was detected in one. CT was used after surgery in patients with a confirmed embryonal rhabdomyosarcoma, and no evidence of metastasis was detected.
The tumour markers HCG and AFP are important for the diagnosis of postpubertal testicular tumours. However, HCG has no clinical significance in the prepubertal group, as choriocarcinoma and embryonal carcinoma are rare in this group [Citation15]. AFP is important in the diagnosis, staging and follow-up of prepubertal testicular tumours, as yolk-sac tumour, which is the commonest, is associated with high AFP levels in >90% of cases. Normally the AFP level is high in neonates and infants, and returns to normal levels after 6–8 months of age. In yolk-sac tumours AFP increases to a high level and does not return to normal. Teratoma can lead to an increase in AFP levels, but not to high levels (<100 ng/mL in infants aged >6 months). This finding can affect the decision as to whether a child will have testicular-preserving surgery or a radical orchidectomy [Citation16]. In the present series AFP levels increased in all cases with yolk-sac tumours and in the patient with a mixed germ-cell tumour.
Teratoma (mature and immature) and epidermoid cysts are the commonest prepubertal testicular benign germ-cell tumours [Citation17]. Being benign and not tending to recur, and as metastasis is rare, testicular-sparing surgery has become the standard of care and a detailed follow-up is not necessary [Citation6,Citation8–Citation11].
Yolk-sac tumour is the commonest tumour in the prepubertal age group. It metastasises by haematogenous spread and the incidence of retroperitoneal metastasis is only 4–6%. In contrast to postpubertal cases, radical orchidectomy is the standard of care for stage I disease, with follow-up by AFP levels and CT. Any recurrence responds well to platinum-based chemotherapy [Citation18]. Radical orchidectomy and chemotherapy is the standard management of patients with stage II and metastatic disease. A retroperitoneal lymph-node dissection (RPLND) is therefore reserved for patients in whom there is persistent retroperitoneal lymphadenopathy or a persistently high AFP level [Citation18]. The three patients with yolk-sac tumours in the present series had stage I disease and were treated by radical orchidectomy, with a return of AFP to normal levels after surgery, and with no recurrence or metastasis at a median follow-up of 12 months.
Sex-cord stromal tumours are rare at a prepubertal age. Juvenile granulosa-cell tumours and Leydig-cell tumours are always benign, and most Sertoli-cell tumours are benign, although rare cases can show malignant behaviour. In the present series there were two patients with Leydig-cell tumours and a third with Leydig-cell hyperplasia. Two patients were treated by testicular-sparing surgery. Similar results were reported by Taskinen et al. [Citation7] and Wang et al. [Citation15], with no recurrence or testicular atrophy.
Two patients with Sertoli-cell tumour were treated by a high inguinal orchidectomy and no further follow-up was required, as both had a confirmed benign histopathology. This is consistent with the reported predominance of benign Sertoli-cell tumours in children [Citation18,Citation19]. Malignant cases were reported in older children and adequate staging is required. If any metastasis is present, a radical orchidectomy followed by RPLND, chemotherapy and radiotherapy is the best treatment [Citation16,Citation18].
Paratesticular tumours are rare in prepubertal patients. Testicular-sparing surgery is the standard treatment for benign tumours [Citation15]. In the patient with a haemangioma, this was suspected during surgery and testicular-sparing surgery was deemed unsuitable. The diagnosis was confirmed by final histopathology and no further follow-up was necessary.
Rhabdomyosarcoma is the most common spermatic-cord sarcoma, and represents 5% of all testicular and paratesticular tumours. The distribution is bimodal, with peaks at 3–4 months and at 16 years [Citation18]. It is an aggressive tumour that infiltrates locally and metastasises via the lymphatic system and bloodstream. However, paratesticular rhabdomyosarcoma has a better prognosis than at other sites, with a 95% 3-year survival rate. Being a malignant tumour, radical orchidectomy followed by RPLND and chemotherapy is the recommended treatment, except in boys aged <10 years with a localised tumour [Citation20]. We reported a 10-year-old boy with an embryonal rhabdomyosarcoma, with no evidence of metastasis and who remained disease-free at a follow-up of 36 months after radical orchidectomy only. This was previously reported by Ciftci et al. [Citation21], and Wang et al. [Citation15] reported the same outcome with radical orchidectomy and adjuvant chemotherapy.
There are several limitations to the present study. The inherent criterion of a retrospective analysis is the main drawback. In addition, there were few patients, but prepubertal testicular tumours are rare, affecting only a few of the tens of millions of susceptible boys. Our results are in parallel to those of the major cancer registry data, where yolk-sac tumour is the commonest, and the results differ from those in other recent single-centre studies. Our review of previous reports helped us to design an algorithm for managing prepubertal testicular tumour in an easily applicable way ().
In conclusion, prepubertal testicular tumours are uncommon, with benign tumours more common in this age group, and testicular-sparing surgery is therefore a safe and effective treatment that should be tried in all cases. Yolk-sac tumour is the commonest prepubertal malignant testicular tumour and radical orchidectomy is sufficient for cancer control in patients with localised disease. Although teratoma was not detected in our series, it is reported to be the second most common type and should be considered.
Conflict of interest
The authors have no conflict of interest to declare.
Source of funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- R.KayPrepubertal testicular tumor registryJ Urol1501993671674
- J.H.RossL.RybickiR.KayClinical behavior and a contemporary management algorithm for prepubertal testis tumors: a summary of the prepubertal testis tumor registryJ Urol168200216751678
- Y.SugitaT.D.ClarnetteC.Cooke- YarboroughC.W.ChowK.WatersJ.M.HutsonTesticular and paratesticular tumours in children: 30 years’ experienceAust NZ J Surg691999505508
- P.D.MetcalfeH.Farivar-MohseniW.FarhatG.McLorieA.KhouryD.J.BägliPediatric testicular tumors. Contemporary incidence and efficacy of testicular preserving surgeryJ Urol170200324122415
- H.G.PohlA.R.ShuklaP.D.MetcalfB.G.CilentoA.B.RetikD.J.Bägliet alPrepubertal testis tumors. Actual prevalence rate of histological typesJ Urol172200423702372
- S.AlaneeA.ShuklaPaediatric testicular cancer. An updated review of incidence and conditional survival from the surveillance, epidemiology and end results databaseBJU Int104200912801283
- S.TaskinenR.FagerholmJ.AronniemiR.RintalaM.TaskinenTesticular tumors in children and adolescentsJ Pediatr Urol42008134137
- H.G.RushtonA.B.BelmanI.SesterhennK.PattersonF.K.MostofiTesticular sparing surgery for prepubertal teratoma of the testis: a clinical and pathological studyJ Urol1441990726730
- S.OottamasathienJ.C.ThomasM.C.AdamsR.T.DeMarcoJ.W.BrockJ.C.Popeet alTesticular tumors in children: a single-institutional experienceBJU Int99200711231126
- E.HisamatsuS.TakagiY.NakagawaY.SugitaK.YoshinoK.UeokaS.TanikazePrepubertal testicular tumors: a 20-years experience with 40 casesInt J Urol172010956959
- A.BujonsJ.C.SfulciniM.PascualO.A.FeuJ.M.GaratH.VillavicencioPrepubertal testicular tumours and efficacy of testicular preserving surgeryBJU Int107201118121816
- D.T.SchneiderG.CalaminusS.KochC.TeskeP.SchmidtR.J.Haaset alEpidemiologic analysis of 1442 children and adolescents registered in the German germ cell tumor protocolsPediatr Blood Cancer422004169175
- A.TreiyerG.BlancE.StarkB.HabenE.TreiyerJ.SteffensPrepubertal testicular tumors: frequently overlookedJ Pediatr Urol32007480483
- J.S.Vallafor the Group D’Etude en Urologie. Pédiatrique. Testis-sparing surgery for benign testicular tumors in childrenJ Urol165200122802283
- X.WangS.XuD.TangM.LiD.WuY.HuangPrepubertal testicular and paratesticular tumors in China: a single-center experience over a 10-years periodJ Pediatr Surg47201215761580
- J.H.RossR.KayPrepubertal testis tumorsRev Urol620041118
- R.KhemakhemY.B.AhmedS.JlidiF.NouiraF.FdhilaA.Charieget alTesticular tumours in prepubertal children: about eight casesAfr J Paediatr Surg102013176179
- P.C.RogersT.A.OlsonJ.W.CullenD.F.BillmireN.MarinaF.Rescorlaet alTreatment of children and adolescents with stage II testicular and stages I and II ovarian malignant germ cell tumors: a pediatric intergroup study – pediatric oncology group 9048 and children’s cancer group 8891J Clin Oncol22200435633569
- B.BurguO.AydogduO.TelliD.KankayaT.SoygurS.Baltaciet alAn unusual cause of infantile gynecomastia: Sertoli cell tumorJ Pediatr Hematol Oncol332011238240
- R.B.RaneyJ.R.AndersonF.G.BarrS.S.DonaldsonA.S.PappoS.J.Qualmanet alRhabdomyosarcoma and undifferentiated sarcoma in the first two decades of life: a selective review of intergroup rhabdomyosarcoma study group experience and rationale for intergroup rhabdomyosarcoma study VJ Pediatr Hematol Oncol232001215220
- A.O.CiftciM.Bingöl-KologluM.E.SenocakF.C.TanyelM.BüyükpamukçuN.BüyükpamukçuTesticular tumors in childrenJ Pediatr Surg36200117961801