Abstract
Objectives:
To assess the feasibility, operative morbidity and oncological outcome of laparoendoscopic single-site (LESS) radical cystectomy.
Patients and methods:
Ten patients with clinical stage T1–T2 bladder cancer underwent a LESS radical cystectomy. The mean (SD) age of the patients was 64.8 (8.6) years and their mean body mass index was 25.9 (2.7) kg/m2. The procedure was done via a single-incision laparoscopic surgery port using a rigid 5-mm 30° long-shaft laparoscope in addition to the two working instruments. A 7-cm Pfannenstiel incision was made to remove the specimens and to allow the creation of an ileal neobladder with hand assistance.
Results:
In eight patients the LESS radical cystectomy was completed as scheduled, with the other two requiring a conversion, one to an open procedure due to locally advanced disease, and the other to conventional laparoscopy due to gas leakage. The mean (SD) operative duration was 236 (49) min, with a mean estimated blood loss of 575 (113) mL, and a mean hospital stay of 5.5 (0.7) days. No postoperative analgesic medications were prescribed and patients returned to normal activity after a mean (SD) of 17.6 (2.6) days. The pathological examination showed negative surgical margins for the bladder specimens, with a mean (SD) of 14 (1.9) lymph nodes retrieved. Seven patients were cancer-free within a mean (SD, range) follow-up of 37 (6, 29–44) months.
Conclusions:
LESS radical cystectomy is technically feasible, with a favourable course and convalescence, and it has an acceptable oncological outcome.
Keywords:
Introduction
Radical cystectomy (RC) is the standard surgical procedure for patients with muscle-invasive urothelial carcinoma and for those with high-risk recurrent non-invasive disease [Citation1]. Laparoscopic and robotic RC have been developed as a minimally invasive alternative to open RC in an attempt to reduce its perioperative morbidity. Comparative studies between laparoscopic, robotic and the open approach have shown an improved overall morbidity in favour of those minimally invasive approaches, in terms of decreased blood loss, shorter hospital stay, and rapid convalescence [Citation2–Citation4]. In both laparoscopic and robotic RC the procedure requires five or six ports for the RC. Laparoendoscopic single-site surgery (LESS) is a further development of minimally invasive surgery that avoids the requirement for additional ports outside the umbilicus. Currently, LESS has been tried for several urological procedures, both reconstructive and ablative [Citation5]. Here we present our initial experience with LESS-RC and its long-term follow-up.
Patients and methods
Between February 2010 and April 2011 10 patients underwent LESS-RC via a multichannel single-incision laparoscopic surgical (SILS) port placed through a 3-cm transumbilical incision. The criteria for selecting patients included those with clinical stage T1–T2 bladder cancer, a body mass index (BMI) of <30 kg/m2, a good performance status with an American Society of Anesthesiologists (ASA) score of 1–2, and no previous pelvic surgery. Based on such selection criteria, all selected patients were clinically T1 or T2, with a mean (SD) age of 64.8 (8.6) years and a BMI of 25.9 (2.7) kg/m2. None of the patients needed neoadjuvant chemotherapy before RC. All patients consented to the LESS-RC approach and the possibility of ancillary incisions/ports or open conversion if necessary during the procedure, in accordance to the rules of the hospital ethics committee. Follow-up evaluations consisted of abdominal ultrasonography every 3 months during the first year and then biannually, abdominal CT every 6 months, and a bone scan scheduled annually.
Surgical procedure
After inducing general anaesthesia the patient was placed supine with a slight abduction of both legs. A 3-cm transumbilical incision was made to place a SILS port (Covidien, Japan), and then pneumoperitoneum was achieved. The patient was placed in the exaggerated Trendelenburg position to facilitate intestinal retraction. A rigid 5-mm 30° long-shaft laparoscope (Karl Storz, Germany) was used to keep the assistant’s hand away from the operator’s hands, hence minimising any potential collision of the working instruments. Two working instruments were used by the operator to carry out the surgery; the right hand was used for the main operating instruments such as scissors, bipolar coagulator, vessel sealing system (LigaSure V, Covidien, USA), and clipping devices, all of which were straight. The left hand was used for an articulated grasper, which was used to support the work of the main instrument and aid in dissection.
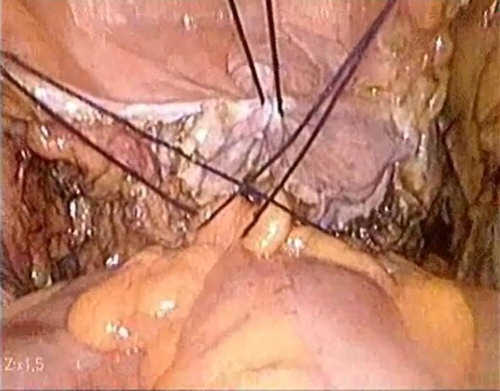
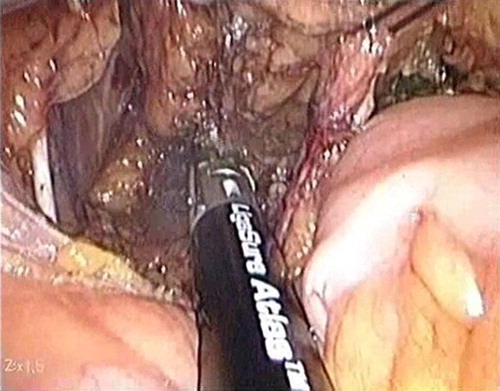
The peritoneum was incised along the right and left obliterated umbilical ligament, and both vasa deferentia were identified and transected. The right and left ureters were identified and dissected down to the urinary bladder. Next, the peritoneum was incised posterior to the urinary bladder. Posterior dissection of the urinary bladder was aided by retracting the dissected ureters and the dome of the bladder towards the anterior abdominal wall, which was done by placing three 2–0 silk percutaneous sutures (). Using a vessel-sealing instrument (LigaSure V) the urinary bladder pedicles were secured on both sides down to the level of Denonvilliers’ fascia (). Dissection anterior to the urinary bladder was done to the level of the endopelvic fascia, which was incised on both sides, and the prostate was dissected from the lateral pelvic wall. The puboprostatic ligaments were transected using scissors. The dorsal vein complex was controlled using an EndoGIA stapler. Scissors were used for the apical dissection and transection of the urethra. The lymph-node dissection template was within the boundaries of the genitofemoral nerve laterally, Cloquet’s node distally, and up to the aortic bifurcation proximally. Specimens (urinary bladder and lymph nodes) were removed through a 7-cm Pfannenstiel incision (), which was also used for extracorporeal reconstruction of an ileal neobladder (Y-shaped pouch) and urethro-ileal anastomosis. Internal JJ ureteric stents were used to support the uretero-ileal anastomosis and were sutured to a 22-F Foley catheter to allow withdrawal of the JJ stent with the removal of the Foley catheter. At the end of the procedure, tube drains (16-F) were placed, one through the umbilical incision and another at the Pfannenstiel incisions.
After surgery bupivacaine hydrochloride was injected subcutaneously at the umbilical and Pfannenstiel incisions. Pain was documented, starting 1 day after surgery, by an analogue pain scale (1–10, minimal pain as 1 and the worst possible pain as 10). Additional analgesic medication was given as demanded by the patient and was recorded.
The drains were removed after 48 h with no discharge, whilst the urethral catheter was left for 14 days. Before removing the catheter a control cystogram was taken to ensure that there was no leakage.
Results
In eight patients the LESS RC was completed successfully as scheduled, with the other two requiring a conversion, one to open surgery due to locally advanced disease (patient 7), which was confirmed to be pT3bN1 on histopathological examination, and the other to conventional laparoscopic surgery due to gas leakage and failure to maintain adequate pneumoperitoneum in a relatively obese patient (patient 10). These two patients had minor postoperative complications, i.e., a low-grade fever (grade II, Clavien system) and mild ileus (grade I, Clavien system). No additional ports were required in the remaining patients, and there were no reported postoperative complications in any of them.
In the eight patients in whom LESS RC was completed, the mean (SD) operative duration was 236 (49) min, comprising 157 (30) min for the RC and 77 (21) min for the diversion, with a mean (SD) estimated blood loss of 575 (113) mL. The mean (SD) duration of hospital stay was 5.5 (0.7) days, and the patients were ambulant on the first day after surgery. No postoperative analgesic medications were prescribed, with a pain score of 2–3 in these eight patients, with a mean (SD) duration for a return to normal activity of 17.6 (2.6) days. The patients’ demographic and perioperative data are shown in .
Table 1 Patient demography and operative data in the 10 patients.
The pathological examination of the urinary bladder specimens showed negative surgical margins in all 10 patients. The histopathological examination showed pT1N0M0 in one case, pT2bN0M0 in four, pT3aN0M0 in four, and pT3bN1M0 in one. The mean (SD, range) number of lymph nodes retrieved was 14 (1.9, 11–17), and they were negative for all patients except one, in whom the RC was converted to open surgery. Within a mean (SD, range) follow-up of 37 (6, 29–44) months, seven patients remained free of cancer. One patient developed liver and bone metastases at 11 months (patient 7), one was missing from the follow-up after 18 months (patient 10), and another patient (No. 2) died in a traffic accident after 13 months.
Discussion
LESS surgery is being developed in urology [Citation6], and although LESS-RC seemed to be more technically challenging and longer than conventional laparoscopy, it still provides the advantages of laparoscopy, with fewer transcutaneous incisions. Accordingly, it would be expected to result in less postoperative pain, a better convalescence and a better cosmetic outcome than laparoscopic RC.
Kaouk et al. [Citation7] reported their first three cases of LESS-RC with an ileal conduit diversion, with a mean (SD) operative duration of 315 (40) min, a mean blood loss of 217 (29) mL and a mean hospital stay of 6 (1) days. In the present series, the operative duration, blood loss and hospital stay were comparable with those reported by Kaouk et al., despite the complexity of the method of diversion used in our series (all the patients had an orthotopic urinary diversion). More recently, Ma et al. [Citation8] reported a series of LESS-RC in five patients, using a home-made single-port device, with a mean operative duration of 208.2 min, a mean blood loss of 270 mL, and a mean postoperative hospital stay of 19.5 days. Similarly, the present results are comparable for operative duration and blood loss, despite the simplicity of the method of urinary diversion that MA et al. used in their five cases. Technically, LESS-RC is difficult to learn, involving co-ordination between the surgeon and the camera holder, navigating the instruments within a limited range of motion, and counterintuitive movements. The most remarkable finding in the present study is the smooth postoperative course. The visual-analogue pain score in all patients was <3. We did not use analgesics, apart from a subcutaneous injection of bupivacaine hydrochloride at the edges of the skin incision. All the patients were ambulant on the first day after surgery, with no difficulties, and the mean (SD) time to return to normal activity was 17.6 (2.6) days.
The oncological safety of any form of RC is evaluated by assessing negative surgical margins and the tumour-free survival rate. In bladder cancer, pelvic lymphadenectomy is an important prognostic factor [Citation9]. An extended pelvic lymphadenectomy might have a therapeutic role [Citation10], but the optimum number of nodes and extent of lymphadenectomy are subjects for debate [Citation11]. In the present series, the lymphadenectomy was within the boundaries described above, and we did not try an extended approach as we are still developing our initial experience. The mean (SD) number of lymph nodes retrieved was 14 (1.9), and all were negative for malignancy in the eight patients in whom the LESS-RC was completed scheduled. This is in accordance with the mean number of lymph nodes retrieved by Kaouk et al. [Citation7], which was 16 (3). In the report by Volkmer et al. [Citation12], of tumour recurrence after RC in 1270 patients, the estimated recurrence rate was 48.6% and the mean time of first recurrence was 20 months for asymptomatic patients and 17.5 months for symptomatic patients. In the present series the follow-up was maintained for a mean (SD) of 37 (6) months, which to our knowledge is the longest follow-up reported for LESS-RC and far exceeds the mean time for a first recurrence after RC as reported by Volkmer et al. [Citation12]. The relatively high 70% tumour-free survival rate estimated in the present series is most probably attributable to the criteria for selecting patients, who were clinically T1–T2.
A Pfannenstiel incision was chosen for specimen retrieval rather than extending the transumbilical incision. It also served as the port for reconstructing an ileal neobladder and the urethro-ileal anastomosis. This retains the superior cosmetic appearance of LESS surgery, and is an excellent and comfortable approach for reconstructing the ileal neobladder, a good access for ileo-urethral anastomosis, and allows the extraction of a large specimen. The JJ internal ureteric stents were used to support the uretero-ileal anastomosis and thus to reduce the hospital stay [Citation13]. The stents were sutured to the urethral catheter, to be removed with it after 2 weeks, and this caused no problems.
We are aware that our series might have a selection bias of patients (who had a good performance status, a BMI of <30 kg/m2, and relatively small confined bladder masses), but we did not want to jeopardise either operative safety or tumour control during the procedure. The postoperative course was smooth, no patient required postoperative analgesics, and the visual-analogue pain score was <3. However, it is too early to confirm that LESS-RC is better than laparoscopy alone in terms of postoperative pain, as this would require clinical trials comparing LESS-RC with the laparoscopic and open approaches.
In conclusion, LESS-RC is technically feasible, with a favourable postoperative course and rapid convalescence. The surgical margins of the bladder specimens were free of tumour and an acceptable number of lymph nodes were retrieved. The preliminary results showed a 70% tumour-specific free survival after 3 years of follow-up.
Conflict of interest
None.
Source of funding
None.
Notes
✰ This journal is partially supported by Karl Storz GmbH. That support had no influence on the peer-review of this paper, which was entirely independent of Karl Storz.
Peer review under responsibility of Arab Association of Urology.
References
- G.J.HuangJ.P.SteinOpen radical cystectomy with lymphadenectomy remains the treatment of choice for invasive bladder cancerCurr Opin Urol172007369375
- J.B.BasilloteC.AbdelshehidT.E.AhleringA.M.ShanbergLaparoscopic assisted radical cystectomy with ileal neobladder: a comparison with the open approachJ Urol1722004489493
- G.P.HaberS.CrouzetI.S.GillLaparoscopic and robotic assisted radical cystectomy for bladder cancer: a critical analysisEur Urol5420085462
- R.M.CowardA.SmithM.RaynorM.NielsenE.M.WallenR.S.PruthiFeasibility and outcomes of robotic-assisted laparoscopic radical cystectomy for bladder cancer in older patientsUrology77201111111114
- W.M.WhiteG.P.HaberR.K.GoelS.CrouzetR.J.SteinJ.H.KaoukSingle-port urological surgery: single-center experience with the first 100 casesUrology742009801804
- D.CanesM.M.DesaiM.AronG.P.HaberR.K.GoelR.J.Steinet alTransumbilical single port surgery: evolution and current statusEur Urol4200810201029
- J.H.KaoukR.K.GoelM.A.WhiteW.M.WhiteR.AutorinoG.P.Haberet alLaparoendoscopic single-port radical cystectomy and pelvic lymph node dissection: initial experience and 2-year follow-upUrology762010857861
- L.L.MaH.BiX.F.HouY.HuangG.L.WangL.Zhaoet alLaparoendoscopic single-site radical cystectomy and urinary diversion: initial experience in China using a homemade single-port deviceJ Endourol262012355359
- E.BrunocillaR.PernettiG.MartoranaThe role of pelvic lymph node dissection during radical cystectomy for bladder cancerAnticancer Res312011271275
- A.KarlP.R.CarrollJ.E.GschwendR.KnüchelF.MontorsiC.G.Stiefet alThe impact of lymphadenectomy and lymph node metastasis on the outcomes of radical cystectomy for bladder cancerEur Urol552009826835
- T.M.KoppieA.J.VickersK.VoraG.DalbagniB.H.BochnerStandardization of pelvic lymphadenectomy performed at radical cystectomy: can we establish a minimum number of lymph nodes that should be removed?Cancer107200623682374
- B.G.VolkmerR.KueferG.C.BartschJr.K.GustR.E.HautmannOncological follow up after radical cystectomy for bladder cancer-is there any benefit?J Urol181200915871593
- S.MicaliP.De CarliR.MianoD.O’SullivanL.LamannaF.MicaliDouble-J ureteral stents: an alternative to external urinary stents in orthotopic bladder substitutionEur Urol52001575584