Abstract
Background:
In patients with pelvic fracture urethral injury there are two options for management: First, to realign as an early primary realignment over a catheter; and second, to place a suprapubic tube with delayed urethroplasty of the inevitable stricture.
Methods:
We reviewed previous reports from 1990 to the present, comparing early endoscopic realignment, early open realignment and suprapubic tube placement, to determine the rates of incontinence, erectile dysfunction and stricture formation.
Results:
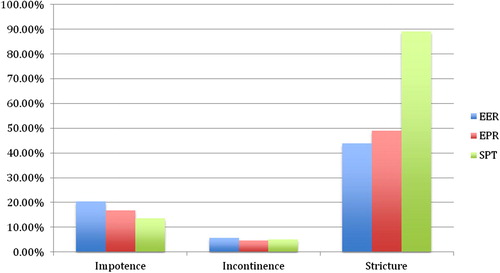
Twenty-nine articles were identified. The rates of erectile dysfunction, incontinence, and stricture formation, respectively, were: for early endoscopic realignment, 20.5%, 5.8% and 43.8%; for open realignment over a catheter, 16.7%, 4.7% and 48.9%; and for a suprapubic tube and delayed urethroplasty 13.7%, 5.0%, and 89.0%. A one-way anova showed no difference in the mean rate of erectile dysfunction (P = 0.53) or incontinence (P = 0.73), and only stricture formation was significantly different (P < 0.1).
Conclusion:
The rates of incontinence and erectile dysfunction are similar between the groups. Only the rate of stricture formation was higher in the suprapubic tube and delayed urethroplasty group.
Introduction
In patients with pelvic fracture urethral injury (PFUI), there are two options for management. The first is early primary realignment over a catheter, and the second is to place a suprapubic tube with delayed urethroplasty (STDU) of the inevitable stricture. Here we evaluate the historical development of the treatment of PFUI and review contemporary reports for the risks and benefits of each therapy, using a one-way anova to compare the mean rates of complications.
Historical overview
Young [Citation1] in 1929 was the first to report the immediate open surgical repair of a PFUI via a perineal approach. Later, it was determined that the lithotomy position associated with the perineal approach was unfavourable with concomitant pelvic fractures; the perineal approach was abandoned for a retropubic approach [Citation2,Citation3]. Whilst the retropubic approach might be safer for a patient with recent fractures, the repair necessitates exploration and dissection of an already traumatised region [Citation4]. Importantly, further reports showed a greater risk of erectile dysfunction (ED) associated with the retropubic approach than with a STDU (0% vs. 33%), probably due to damage to the surrounding neurovascular bundle [Citation5]. There was also concern that dissecting the retropubic space could convert a partial urethral tear into a complete urethral tear [Citation6]. With this being the case, the immediate open retropubic surgical repair of an acute PFUI injury fell out of favour.
Meanwhile, urologists were also working on realignment techniques, to bring the urethra together over a catheter, without retropubic dissection. The first realignment was reported in 1934 [Citation7]. Traction was then added to the catheter placed through the urethra, via weights, to aid in the re-approximation of the urethral edges [Citation8]. Several further studies showed that there was still fibrous tissue bridging the gap, and not mucosa, even with the aid of weights [Citation2,Citation9]. In addition, the use of weights was abandoned as it was shown to cause worse incontinence because of damage to the bladder neck, and distal urethral necrosis [Citation10].
In 1953, Johanson [Citation11] was the first to question whether or not the STDU was superior to the realignment strategy. Whilst the stricture is inevitable, a STDU guarantees that the degree of ED is due to the initial injury and not the manipulation for early non-endoscopic realignment (EPR) [Citation12]. Suprapubic cystotomy became the preferred treatment for the next 30 years[Citation4]. In the early 1990s novel techniques for minimally invasive, radiological and endoscopic techniques for realignment were introduced which challenged the standard of suprapubic cystotomy alone [Citation13–Citation16]. Since then, there have been many reports arguing for both methods of the management.
Complications
The goal of management is to realign the urethra whilst minimising the risks of ED, incontinence and subsequent urethral stricture [Citation4]; [Citation13–Citation41] and summarise the findings of the above complications in early endoscopic realignment (EER), early open primary realignment, and STDU in studies from 1990 to the present. Importantly, in these series, many of the patients did not undergo primary realignment because of haemodynamic instability of the patient, or failure of primary realignment, which might be associated with a worse initial injury.
Table 1 Contemporary studies evaluating EER, EPR and STDU for rates of ED, incontinence, and stricture formation.
ED
The main concern of EPR is further damage to the neurovascular bundle. Whilst the open retropubic approach probably affects the neurovascular bundle [Citation5], increasing the risk of ED [Citation4,Citation42], there is growing evidence that this is no longer the case with primary EER techniques currently used [Citation4,Citation32,Citation35]. Dhabuwala et al. [Citation43] were the first to suggest that the injury, not the treatment, induced the ED. Kotkin and Koch [Citation35] went on to report their experience with EPR vs. simple catheter placement (with partial disruption), and found no difference to suggest that EPR made the ED worse. MRI [Citation44] and MRI with duplex ultrasonography [Citation45] studies show that patients with ED have more significant damage than those with no ED, all in a cohort of patients who had been treated only with STDU. summarises the finding that rates of ED are equal between EER (P = 0.53), EPR and STDU, at 20.5%, 16.7% and 13.7%, respectively.
Incontinence
Incontinence after a PFUI is rare, and when present it is believed that the initial injury is responsible for the degree of incontinence [Citation4]. Several review articles did not support open suture realignment due to the increased risk of incontinence [Citation4,Citation42]. However, this detrimental effect was seen for primary suture realignment, with a 21% rate of incontinence after open suture realignment, compared with 4% for STDU and 5% for EPR [Citation4]. The results in this review were based on small series, and a variation of open techniques. shows that the rate of incontinence is similar between EER, EPR and STDU, at 5.8%, 4.7% and 5.0%, respectively (P = 0.73). This is probably partly due to the minimal manipulation with current open and endoscopic realignment techniques.
Stricture
Johanson [Citation11] was the first to accept that an early suprapubic tube leads to inevitable stricture formation. This has remained true through the modern era. The potential advantages of STDU were really to avoid the risk of incontinence and ED with EPR techniques. As shown above, the chance of this is equal between EPR and EER. However, the stricture rate remains very high for STDU compared with that of EER and EPR, at 89.0%, 43.8% and 48.9%, respectively (P < 0.01).
Other potential benefits of EPR vs. STDU include a more rapid return to spontaneous voiding [Citation26]. In addition, Kulkarni et al. [Citation46] reported on their experience, in the developing vs. developed world, of the acute management of PFUI. They reported higher rates of suprapubic tube placement in patients in India than in Italy (80% vs. 50%, respectively) and subsequently higher rates of complex strictures in patients in India than in Italy (85% vs. 32%, respectively), and finally the management of the stricture was easier in the Italian population, with 28% treated successfully with endoscopic treatment, compared to 1% in the Indian group [Citation46]. The authors support early urological evaluation and EPR as likely contributors to the decreased rates of complex strictures.
Several authors have also shown that the strictures after EPR can often be treated successfully with dilatation and direct visual internal urethrotomy alone vs. open repair [Citation21,Citation26,Citation32,Citation36]. Koraitim [Citation47] recently showed that those with primary realignment were found to have fewer abdomino-perineal repairs required than those with only a suprapubic tube (24% vs. 42%), and also had shorter defects.
Other complications
Direct complications from realignment have been reported in very few patients. Pelvic abscess occurred in one of 43 (3%) patients in one study [Citation48], and there are two reports of perineal abscess in one of six [Citation41] and one of four patients [Citation33]. A urethral fistula was detected in one of 14 patients in another study [Citation14]. Septicaemia was a complication in 15% of patients with delayed realignment, with a mean time of placement of 10 days[Citation27].
Technique
Primary endoscopic realignment
Once the PFUI is diagnosed most authors still attempt a single, gentle catheter placement at the bedside or in the operating room, by a urologist [Citation24,Citation38,Citation39]. If this fails, then there are various endoscopic techniques available. Many authors favour retrograde flexible cystoscopy [Citation20,Citation24,Citation26] after failing to place a catheter. Next, either rigid or flexible cystoscopy can be done simultaneously through a cystotomy and through the urethra [Citation15,Citation20,Citation24] whilst the two operators move towards each other until one cystoscope passes the defect so that a wire can be placed to allow the placement of a retrograde council-tip catheter () [Citation50].
Figure 2 Endoscopic realignment with retrograde rigid urethroscopy and flexible antegrade urethroscopy. With permission from [Citation50].
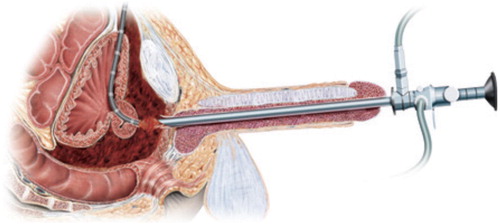
The success rates of endoscopic realignment are excellent, at 72–100% [Citation26,Citation29,Citation30,Citation32]. More experience improves success, and one group initially reported an 80% success [Citation49] then later a 93% success rate [Citation27] with more experience.
Other techniques include magnetic catheters [Citation16], interlocking sounds [Citation39], passing a wire [Citation14] or feeding tube [Citation32,Citation40], or an antegrade catheter placed through a suprapubic tract [Citation38] across the defect. Radiographic techniques have also been described [Citation36].
Timing of catheter placement
Most authors recommend attempting to place the catheter as soon as it is feasible. Some authors suggest that if the initial attempt is unsuccessful, then simply leave a suprapubic tube and try again after 2–3 days[Citation24]. Delayed placement has been successful as late as 10–19 days after injury[Citation27,Citation40].
When to remove the catheter
Authors do not agree on the duration of catheterisation after early primary realignment, and values range from 3 to 8 weeks[Citation39,Citation40,Citation48]. A reasonable approach might be to take a peri-catheter retrograde urethrogram or immediate retrograde urethrogram at the time of catheter removal, after at least 3 weeks for partial disruption, and 6 weeks for complete disruption [Citation29]. With extravasation, the catheter is left in place or replaced and tested again every week until there is no extravasation.
STDU
The suprapubic tube can initially be placed via a cystotomy during an open laparotomy, or a trocar into a distended bladder, or a needle passed into the bladder, then a wire passed through the needle, and serial dilatations over the wire until a suprapubic catheter can be passed. Most authors endorse a 3–6-month period of healing before an attempt at delayed urethroplasty [Citation51]. In experienced hands, the long-term success rates are 90–98% [Citation52–Citation57].
Conclusion
Whilst the rates of ED and incontinence are similar between EPR, EER and STDU, the increased rate of strictures, and more complex strictures, with STDU lead us to suggest EPR or EER as an initial approach for the immediate treatment of a PFUI. Given the ease and success of EER we prefer this to other techniques of realignment. However, as seen in and , the success of EPR is equally successful in experienced hands. Lastly, not all patients can successfully undergo early realignment. STDU might be needed in the unstable patient, in complex injuries, and when attempts at early realignment fail. Fortunately, the ultimate anastomotic urethroplasty can be performed with a high chance of success in centres of excellence.
Conflict of interest
Dr. Warner and Dr. Santucci have no conflicts of interest to report.
Source of funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- H.H.YoungTreatment of complete rupture of the posterior urethra, recent or ancient, by anastomosisJ Urol21192941
- S.S.ClarkR.F.PrudencioLower urinary tract injuries associated with pelvic fractures. Diagnosis and managementSurg Clin North Am521972183201
- J.M.PierceJr.Management of dismemberment of the prostatic-membranous urethra and ensuing stricture diseaseJ Urol1071972259264
- M.M.KoraitimPelvic fracture urethral injuries: the unresolved controversyJ Urol161199914331441
- K.S.CoffieldW.L.WeemsExperience with management of posterior urethral injury associated with pelvic fractureJ Urol1171977722724
- W.L.WeemsManagement of genitourinary injuries in patients with pelvic fracturesAnn Surg1891979717723
- J.K.OrmondR.M.CothranA Simple method of treating complete severance of the urethra complicating fractures of the pelvisJAMA102193421802181
- J.H.DeWeerdImmediate realignment of posterior urethral injuryUrol Clin North Am419777580
- H.RagdeG.F.McInnesTranspubic repair of the severed prostatomembranous urethraJ Urol1011969335337
- I.H.Al-AliI.HusainDisrupting injuries of the membranous urethra – the case for early surgery and catheter splintingBr J Urol551983716720
- B.JohansonThe reconstruction in stenosis of the male urethraZ Fur Urologie461953361375
- R.Turner-WarwickPrevention of complications resulting from pelvic fracture urethral injuries – and from their surgical managementUrol Clin North Am161989335358
- F.GuilleB.CipollaJ.M.LevequeS.GuirassyJ.F.OlivoB.LobelEarly endoscopic realignment of complete traumatic rupture of the posterior urethraBr J Urol681991178180
- J.K.CohenG.BergG.H.CarlD.D.DiamondPrimary endoscopic realignment following posterior urethral disruptionJ Urol146199115481550
- E.L.GheilerJ.R.FronteraImmediate primary realignment of prostatomembranous urethral disruptions using endourologic techniquesUrology491997596599
- J.R.PorterT.K.TakayamaA.J.DefalcoTraumatic posterior urethral injury and early realignment using magnetic urethral cathetersJ Urol1581997425430
- H.J.QuintT.H.StanisicAbove and below delayed endoscopic treatment of traumatic posterior urethral disruptionsJ Urol1491993484487
- J.RehmanD.SamadiR.RicciardiJr.E.KreutzerEarly endoscopic realignment as primary therapy for complete posterior urethral disruptionsJ Endourol/Endourol Soc121998283289
- B.R.JepsonJ.A.BoullierR.G.MooreR.O.ParraTraumatic posterior urethral injury and early primary endoscopic realignment: evaluation of long-term follow-upUrology53199912051210
- S.J.KielbZ.L.VoeltzJ.S.WolfEvaluation and management of traumatic posterior urethral disruption with flexible cystourethroscopyJ Trauma5020013640
- S.M.MoudouniJ.J.PatardA.ManuntaP.GuiraudB.LobelF.GuilleEarly endoscopic realignment of post-traumatic posterior urethral disruptionUrology572001628632
- J.KuM.E.KimY.S.JeonN.K.LeeY.H.ParkManagement of bulbous urethral disruption by blunt external trauma: the sooner, the better?Urology602002579583
- H.TaziM.OualiM.H.LrhorfiS.MoudouniK.TaziA.LakrissaEndoscopic realignment for post-traumatic rupture of posterior urethraProgres En Urologie: J l’Assoc Francaise D’urologie de Societe Francaise D’urologie13200313451350
- V.B.MouravievM.CoburnR.A.SantucciThe treatment of posterior urethral disruption associated with pelvic fractures: comparative experience of early realignment versus delayed urethroplastyJ Urol1732005873876
- C.E.HealyD.S.LeonardR.CahillD.MulvinD.QuinlanPrimary endourologic realignment of complete posterior urethral disruptionIrish Med J1002007488489
- P.HadjizachariaK.InabaP.G.TeixeiraP.KokorowskiD.DemetriadesC.BestEvaluation of immediate endoscopic realignment as a treatment modality for traumatic urethral injuriesJ Trauma64200814431449
- E.O.Olapade-OlaopaO.M.AtalabiA.O.AdekanyeS.A.AdebayoK.A.OnawolaEarly endoscopic realignment of traumatic anterior and posterior urethral disruptions under caudal anaesthesia – a 5-year reviewInt J Clin Prac642010612
- M.SoferN.J.MabjeeshJ.Ben-ChaimG.AviramY.Bar-YosefH.Matzkinet alLong-term results of early endoscopic realignment of complete posterior urethral disruptionJ Endourol/Endourol Soc24201011171121
- L.S.LeddyA.J.VanniH.WessellsB.B.VoelzkeOutcomes of endoscopic realignment of pelvic fracture associated urethral injuries at a level 1 trauma centerJ Urol1882012174178
- F.J.KimA.PompeoD.SehrtW.R.MolinaR.M.Mariano da CostaC.Julianoet alEarly effectiveness of endoscopic posterior urethra primary alignmentJ Trauma Acute Care Surg752013189194
- D.A.HusmannW.T.WilsonT.B.BooneT.D.AllenProstatomembranous urethral disruptions. management by suprapubic cystostomy and delayed urethroplastyJ Urol14419907678
- S.HerschornA.ThijssenS.B.RadomskiThe value of immediate or early catheterization of the traumatized posterior urethraJ Urol148199214281431
- H.W.FollisM.O.KochW.S.McDougalImmediate management of prostatomembranous urethral disruptionsJ Urol147199212591262
- M.M.KoraitimPelvic fracture urethral injuries. evaluation of various methods of managementJ Urol156199612881291
- L.KotkinM.O.KochImpotence and incontinence after immediate realignment of posterior urethral trauma: result of injury or management?J Urol155199616001603
- T.A.LonderganL.H.GundersenM.J.van EveryEarly fluoroscopic realignment for traumatic urethral injuriesUrology491997101103
- M.L.PodestaR.MedelR.CasteraA.RuarteImmediate management of posterior urethral disruptions due to pelvic fracture: therapeutic alternativesJ Urol157199714441448
- D.S.ElliottD.M.BarrettLong-term followup and evaluation of primary realignment of posterior urethral disruptionsJ Urol1571997814816
- R.AsciS.SarikayaR.BuyukalpelliA.SaylikA.F.YilmazS.YildizVoiding and sexual dysfunctions after pelvic fracture urethral injuries treated with either initial cystostomy and delayed urethroplasty or immediate primary urethral realignmentScand J Urol Nephrol331999228233
- E.BalkanN.KilicH.DogruyolThe effectiveness of early primary realignment in children with posterior urethral injuryInt J Urol1220056266
- M.SalehipourA.KhezriR.AskariP.MasoudiPrimary realignment of posterior urethral ruptureUrol J22005211215
- G.D.WebsterG.L.MathesC.SelliProstatomembranous urethral injuries. A review of the literature and a rational approach to their managementJ Urol1301983898902
- C.B.DhabuwalaS.HamidD.M.KatsikasJ.M.PierceJr.Impotence following delayed repair of prostatomembranous urethral disruptionJ Urol1441990677678
- Y.NarumiH.HricakN.A.ArmenakasC.M.DixonJ.W.McAninchMR imaging of traumatic posterior urethral injuryRadiology1881993439443
- N.A.ArmenakasJ.W.McAninchT.F.LueC.M.DixonH.HricakPosttraumatic impotence. Magnetic resonance imaging and duplex ultrasound in diagnosis and managementJ Urol149199312721275
- S.B.KulkarniG.BarbagliJ.S.KulkarniG.RomanoM.LazzeriPosterior urethral stricture after pelvic fracture urethral distraction defects in developing and developed countries, and choice of surgical techniqueJ Urol183201010491054
- M.M.KoraitimEffect of early realignment on length and delayed repair of postpelvic fracture urethral injuryUrology792012912915
- D.E.PattersonD.M.BarrettR.P.MyersJ.H.DeWeerdB.B.HallR.C.BensonJr.Primary realignment of posterior urethral injuriesJ Urol1291983513516
- E.O.Olapade-OlaopaS.A.AdebayoO.M.AtalabiA.A.PopoolaI.A.OgunmodedeU.F.EnabuleleRigid retrograde endoscopy under regional anaesthesia. A novel technique for the early realignment of traumatic posterior urethral disruption.Afr J Med Med Sci312002277280
- M.HohenfellnerR.A.SantucciEmergencies in Urology2007Springer Verlag
- C.ChappleG.BarbagliG.JordanA.R.MundyN.Rodrigues-NettoV.Pansadoroet alConsensus statement on urethral traumaBJU Int93200411951202
- S.J.HosseiniA.RezaeiM.MohammadhosseiniI.RezaeiB.JavanmardSupracrural rerouting as a technique for resolution of posterior urethral disruption defectsUrol J62009204207
- A.F.MoreyJ.W.McAninchReconstruction of posterior urethral disruption injuries: outcome analysis in 82 patientsJ Urol1571997506510
- M.R.CooperbergJ.W.McAninchN.F.AlsikafiS.P.ElliottUrethral reconstruction for traumatic posterior urethral disruption. outcomes of a 25-year experienceJ Urol178200720062010
- W.S.KizerN.A.ArmenakasS.B.BrandesA.G.CavalcantiR.A.SantucciA.F.MoreySimplified reconstruction of posterior urethral disruption defects: limited role of supracrural reroutingJ Urol177200713781381
- M.M.KoraitimTranspubic urethroplasty revisited: total, superior, or inferior pubectomy?Urology752010691694
- N.LumenP.HoebekeB.D.TroyerB.YsebaertW.OosterlinckPerineal anastomotic urethroplasty for posttraumatic urethral stricture with or without previous urethral manipulations. a review of 61 cases with long-term followupJ Urol181200911961200