Abstract
Objective:
To analyse the effects of baseline body mass index (BMI) on the postoperative and remote consequences of nephrectomy in living kidney donors, as body weight is conventionally used as an exclusion criterion for kidney donation and a BMI of <35 kg/m2 is often required.
Patients and methods:
We retrospectively studied 189 living-related kidney donors who had their nephrectomy between 1986 and 2009 in our urology department. We recorded the BMI at the time of donation, and analysed variables after surgery, and clinico-biological factors remotely. The effect of the initial BMI after surgery and much later after nephrectomy was assessed.
Results:
The mean follow-up was 9.28 years. The mean (range) BMI at the time of donation was 26.5 (18.5–41.1) kg/m2; 33% of donors were overweight (BMI 25–30) and 21% were obese (⩾30), with 10.5% having a BMI of >35 kg/m2. The duration of hospitalisation was not related to the BMI. There was no significant difference between the mean BMI of donors with a simple postoperative history and donors who had complications after surgery. Among obese donors, only 7.7% had a complication, which was a surgical-site infection in all cases. The baseline BMI was higher among donors who maintained normal renal function and no proteinuria than in donors with impaired renal function and/or proteinuria; the difference was not significant. The occurrence of hypertension or diabetes was independent of baseline BMI. Donors with dyslipidaemia had no significantly greater baseline BMI than those with no dyslipidaemia.
Conclusion:
The BMI at the time of kidney donation does not seem to influence the short- or long-term consequences of nephrectomy in living donors.
Abbreviation:
Keywords:
Introduction
Living-donor kidney transplantation is currently considered the best treatment for end-stage kidney failure. The success not only depends on its results in the recipient, with a long graft survival time expected, but also on the safety of nephrectomy in the donors. To ensure this safety, the selection of potential donors must be rigorous. Even if the donor-selection criteria are not standardised, they have been the subject of international recommendations in a consensus conference held in Amsterdam in 2004 [Citation1]. A body mass index (BMI) of <35 kg/m2 is one of the key elements required to accept a potential donor. The increasing prevalence of obesity therefore threatens the availability of living donors [Citation2].
The aim of the present study was to assess the effects of the baseline BMI on the postoperative and remote consequences of nephrectomy in living donors.
Patients and methods
We conducted a retrospective study of 189 living-related kidney donors who had their nephrectomy between 1986 and 2009 in our urology department. We recorded the BMI at the time of donation and analysed variables after surgery, specifying the postoperative course and duration of hospital stay. Clinico-biological variables were assessed remotely, including renal function (serum creatinine level and creatinine clearance), proteinuria, hypertension, diabetes and dyslipidaemia. The effect of the baseline BMI during the perioperative period and later after nephrectomy was then assessed. All data were analysed using standard statistical software and the results considered statistically significant at P < 0.01.
Results
The epidemiological characteristics of the donors are summarised in . The mean (SD, range) age was 41.8 (12.1, 20–67), the body mass at the time of donation was 70.9 (13.3, 42–108) kg, the BMI was 26.5 (4.8, 18.5–41.1) kg/m2 and 33% of donors were overweight (BMI 25–<30) and 21% were obese (BMI ⩾ 30 kg/m2).
Table 1 The epidemiological characteristics of the donors.
All donors were operated by lumbotomy, and the mean (SD, range) duration of hospitalisation was 5.5 (3, 3–28) days. It was 5.6 days for donors with a BMI of <25 kg/m2, 4.9 days for overweight donors and 5.3 days for obese donors. There was no statistical correlation between the baseline BMI and duration of hospital stay (P = 0.57).
Nineteen donors (10%) had postoperative complications, and their mean baseline BMI was 25.6 kg/m2. The mean baseline BMI of the 170 donors with a simple postoperative course was 26.6 kg/m2, and the difference was not significant between the groups of donors with and with no complications (P = 0.48).
Among obese donors, 93% had a simple postoperative course; only 7% of obese donors had a postoperative complication, which was a surgical-site infection in all.
The mean (SD, range) follow-up of the donors was 9.2 (6.3, 0.6–24.8) years. Donors who maintained normal renal function (creatinine clearance > 90 mL/min) during the follow-up and who did not develop proteinuria had a mean baseline BMI of 26.8 kg/m2. However, the mean baseline BMI of donors with impaired renal function and/or proteinuria was 25.2 kg/m2, and 28% were obese (). Thus, the baseline BMI was higher in donors with normal renal function and no proteinuria during the follow-up, but with no significant difference (P = 0.13).
Hypertension was diagnosed in 45 donors during the follow-up, and their mean baseline BMI was 28.7 kg/m2. The baseline BMI of donors with a normal blood pressure was lower (25.8 kg/m2) but with no significant difference (P = 0.22). There was no statistical correlation between the baseline BMI and remote hypertension in donors (P = 0.18).
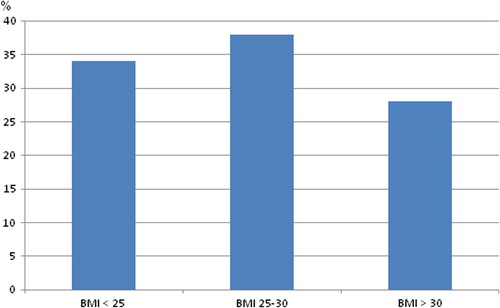
Diabetes was diagnosed in 21 donors after nephrectomy; their mean baseline BMI was 27.2 kg/m2 and 38% of them were obese at the time of donation. The mean baseline BMI of non-diabetic donors was not significantly lower (26.4 kg/m2). There was no statistical correlation between baseline BMI and remote diabetes in donors (P = 0.59).
Donors who developed dyslipidaemia during the follow-up had a greater mean baseline BMI than those with no dyslipidaemia (27.3 vs. 25.9 kg/m2) but the difference was not statistically significant (P = 0.13).
Discussion
Before being accepted for kidney donation, living donors must undergo a strict medical investigation to ensure the best functional outcome for recipients, and no or minimal donor morbidity. Body weight is one of the main exclusion criteria, with a BMI of <35 kg/m2 required by the recommendations of the consensus conference in 2004 [Citation1]. The BMI beyond which the person is not accepted for donation is sometimes set at 40 kg/m2 [Citation3]. Of the donors in the present study, 21% were obese and only one had a BMI of >40 kg/m2. In a literature review, Young et al. [Citation4] reported the results of 10 studies involving 484 obese living donors with a mean BMI of 34.5 kg/m2.
The mean weight at the time of nephrectomy in the present donors was 70.9 kg and the mean baseline BMI was 26.5 kg/m2, respectively, comparable to those of the series of Samhan et al. [Citation5] and Textor et al. [Citation6].
According to Young et al. [Citation4], the risk of postoperative complications secondary to nephrectomy in donors was no greater among obese donors. However, in a study of 871 donors, conducted by Johnson et al. [Citation7], a weight of ⩾100 kg was among risk factors significantly associated with postoperative complications of nephrectomy for kidney donation. In the present series there was no significant difference in baseline BMI between donors with or with no postoperative complications.
By contrast with the present study, where there was no statistical correlation between the duration of hospitalisation and baseline BMI, there was a statistically significant difference reported by Young et al. [Citation4] between the duration of hospital stay in obese donors and non-obese donors.
Some authors reported that obese donors were at risk of kidney dysfunction and proteinuria during the follow-up [Citation8]. This was not confirmed in the short term by Reese et al. [Citation9] who showed, in a recent retrospective study of >5000 living kidney donors, that at 6 months renal function did not differ in obese and non-obese donors. Also, Rook et al. [Citation10] reported that the function of the remaining kidney was preserved regardless of the initial BMI. In the present series, donors with normal renal function and no proteinuria during the follow-up had paradoxically a higher mean baseline BMI than donors with impaired renal function and/or proteinuria. However, the difference was not statistically significant.
Contrary to the findings of Praga et al. [Citation8], we noted that the occurrence of micro-albuminuria or proteinuria in our donors was not statistically correlated with their initial BMI. As in our study, Gossmann et al. [Citation11] found no significant difference in terms of baseline BMI between groups of donors with or with no proteinuria.
In some series, hypertension after kidney donation was positively correlated with the baseline BMI [Citation12,Citation13]. In the present study and that of Gossmann et al. [Citation11], there was no statistical correlation between the BMI at the time of donation and high blood pressure during the follow-up.
Unlike in the present study, where the occurrence of diabetes appeared to be independent of baseline BMI, El-Agroudy et al. [Citation14] reported that diabetes was more common among those donors who gained more weight after nephrectomy.
Demir et al. [Citation15] found that hyperlipidaemia was significantly associated with weight gain and reduced physical activity. In the present study, dyslipidaemic donors had a higher mean baseline BMI than other donors, with no significant difference.
In conclusion, the BMI at the time of donation did not seem to influence the short- or long-term consequences of nephrectomy in living donors in the present series. Thus, we consider that it is acceptable to select overweight or obese potential donors.
Conflict of interest
None.
Source of funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- F.DelmonicoReport of the Amsterdam forum on the care of the live kidney donor: data and medical guidelinesTransplantation79Suppl. 620055366
- R.N.FoleyH.N.IbrahimLong-term outcomes of kidney donorsCurr Opin Nephrol Hypertens192010129133
- G.V.PrasadD.LipszycM.HuangM.L.NashL.RapiA prospective observational study of changes in renal function and cardiovascular risk following living kidney donationTransplantation86200813151318
- A.YoungL.StorsleyA.X.GargD.TreleavenC.Y.NguanM.S.Cuerdenet alHealth outcomes for living kidney donors with isolated medical abnormalities: a systematic reviewAm J Transplant8200818781890
- M.SamhanA.M.OmarT.Al-Sae’edM.al-MousawiEarly changes in kidney function following living donor nephrectomyTransplant Proc311999365366
- S.C.TextorS.J.TalerN.DriscollT.S.LarsonJ.GloorM.GriffinF.Cosioet alBlood pressure and renal function after kidney donation from hypertensive living donorsTransplantation782004276282
- E.M.JohnsonM.J.RemucalK.J.GillinghamR.A.DahmsJ.S.NajarianA.J.MatasComplications and risks of living donor nephrectomyTransplantation64199711241128
- M.PragaE.HernandezJ.C.HerreroE.MoralesY.RevillaR.Díaz-Gonzálezet alInfluence of obesity on the appearance of proteinuria and renal insufficiency after unilateral nephrectomyKidney Int58200021112118
- P.P.ReeseH.I.FeldmanD.A.AschA.ThomassonJ.ShultsR.D.BloomShort-term outcomes for obese live kidney donors and their recipientsTransplantation882009662671
- M.RookR.J.BosmaW.J.Van Sonet alNephrectomy elicits impact of age and BMI on renal hemodynamics: lower postdonation reserve capacity in older or overweight kidney donorsAm J Transplant8200820772085
- J.GossmannA.WilhelmH.G.KachelJ.JordanU.SannH.Geigeret alLong-term consequences of live kidney donation follow-up in 93% of living kidney donors in a single transplant centerAm J Transplant5200524172424
- C.GracidaR.EspinozaU.CedilloJ.CancinoKidney transplantation with living donors. Nine years of follow-up of 628 living donorsTransplant Proc352003946947
- V.E.TorresK.P.OffordC.F.AndersonJ.A.VelosaP.P.FrohnertJ.V.DonadioJret alBlood pressure determinants in living-related renal allograft donors and their recipientsKidney Int31198713831390
- A.E.El-AgroudyA.A.SabryE.W.WafaA.H.NeamatallaA.M.IsmailT.Mohsenet alLong-term follow-up of living kidney donors: a longitudinal studyBJU Int100200713511355
- E.DemirM.BalalS.PaydasY.SertdemirU.ErkenDyslipidemia and weight gain secondary to lifestyle changes in living renal transplant donorsTransplant Proc37200541764179