Abstract
Objective:
To evaluate the long-term results after managing intraoperative and late-diagnosed cases of iatrogenic ureteric injury (IUI), treated endoscopically or by open surgery.
Patients and methods:
Patients immediately diagnosed with IUI were managed under the same anaesthetic, while those referred late had a radiological assessment of the site of injury, and endoscopic management. Open surgical procedures were used only for the failed cases with previous diversion.
Results:
In all, 98 patients who were followed had IUI after gynaecological, abdominopelvic and ureteroscopic procedures in 60.2%, 14.3% and 25.5%, respectively. The 27 patients diagnosed during surgery were managed immediately, while in the late-referred 71 patients ureteroscopic ureteric realignment with stenting was successful in 26 (36.6%). Complex open reconstruction with re-implantation or ureteric substitution, using bladder-tube or intestinal-loop procedures, was used in 27 (60%), 16 (35.5%) and two (4.5%) patients of the late group, respectively. A long-term radiological follow-up with a mean (range) of 46.6 (24.5–144) months showed recurrent obstruction in 16 (16.3%) patients managed endoscopically and reflux in six (8.3%) patients. Three renal units only (3%) were lost in the late-presenting patients.
Conclusion:
Patients managed immediately had better long-term results. More than a third of the late-diagnosed patients were successfully managed endoscopically with minimal morbidity. Open reconstruction by an experienced urologist who can perform a complex substitutional procedure was mandatory to preserve renal units in the long-term.
Introduction
Iatrogenic ureteric injury (IUI) is an uncommon complication during gynaecological and pelvic operations, and it is difficult to diagnose without a high index of suspicion. Unrecognised or improperly managed patients are associated with severe morbidity, with urinoma, fever, septicaemia or urinary fistula, and the neglected patients present later with stricture or a non-functional renal unit. Although retrograde ureterography is the most accurate diagnostic test, CT or complete IVU are also very useful diagnostic tools [Citation1,Citation2]. The initial diagnosis of IUI is usually missed in up to 70% of cases and the final outcome of treatment is influenced by the time of diagnosis [Citation3]. Injuries identified intraoperatively are immediately repaired over a stent or re-implanted into the bladder, while the primary objective in the treatment of late-presented cases is ablation of obstruction, prevention of urinary incontinence and preservation of renal function.
In the last decade, the successful endoscopic placement of a JJ stent via a retrograde or antegrade route allows the ureteric fistula to heal, preserves renal function, and is a reasonable recommendation to avoid major complex open reconstructive surgery in 23.5% of patients [Citation4].
In the present study we evaluated the long-term results after managing intraoperative and late-diagnosed cases of IUI, treated endoscopically or by open surgery.
Patients and methods
From November 1986 to December 2014, 98 patients with ureteric injuries caused during open gynaecological surgery, or to the abdomen and pelvis, or endoscopic treatment of ureteric stones, were managed in our institution. The types of procedures that were associated with these injuries are presented in shown in . Patients with a vesicovaginal fistula and those whose fistula developed without surgery were excluded from the study. Injuries identified during surgery were concomitantly managed under the same anaesthetic, with a small cystotomy incision and passing a ureteric catheter (6 F) up to the ipsilateral ureter, with injection of sterile methylene blue. Leakage of the dye in the operative field or failure to pass the catheter confirmed the site of injury or obstruction of the ureter. In these patients, dissection around the ureter to de-ligate or even repair the injury site was done whenever possible. In patients with a complete injury at the pelvic inlet, the healthy split ureteric ends were re-anastomosed around a stent. Patients with an unhealthy or short lower segment were managed with a ureteroneocystostomy or substitution to the ureteric defect using a Boari bladder flap, according to the level of the healthy proximal ureter from the urinary bladder. Most of these injured ureters had a normal calibre, and therefore a submucosal tunnel was created in the re-implanted unit, with a stent placed for 4–8 weeks.
Table 1 The type of surgical operations and method of repair associated with the IUI.
Patients with a suspected injury who presented or were referred late after surgery, with a recurrent fever or ipsilateral flank pain, or those with a urinary fistula, had a laboratory and radiological assessment. A radiological evaluation is the first step to identify either obstruction or extravasation of the dye from its normal pathway if there is a fistula, or even absence of excretion with or with no urinoma collection. Ultrasonography (US) and IVU were used routinely for the early cases, but in the last few years contrast-enhanced CT has been used for the diagnosis, especially with coronal reconstruction films.
Opacification of an extra-ureteric collection of the contrast medium excreted, or non-opacification of the distal ureter or urinary ascites, are very helpful in the diagnosis. All patients had a cystoscopic examination of the bladder to exclude concomitant urinary bladder injury. After identifying the ureteric orifices, under C-arm control, we try to pass a guidewire or inject contrast medium via an open-tip ureteric catheter or small-calibre ureteroscope, which can locate the site and degree of ureteric injuries. In patients with a partial injury, a JJ stent is fixed for 8–12 weeks. However, if it is not possible to access the proximal ureter after a failed PTFE catheter or balloon dilatation, a percutaneous nephrostomy (PCN) tube is placed, or an open exploration and repair is done, according to the time from previous injury. The reconstructive procedure depends on the site of the ureteric injury and the capacity of the bladder. We usually start by identifying the healthy ureter above the common iliac artery, followed by careful dissection down to the site of injury. A trial to access the distal ureteric segment was not always feasible, due to severe adhesion and fibrosis following a period of local cellulitis and urinary leakage. The ureter was implanted directly into the dome of the bladder with a submucosal tunnel and nipple according to the size of its lumen, or via a substitute using either a bladder tube or intestinal segment, to give a tension-free water-tight anastomosis. In patients with a previous PCN the tube was clamped for 1 day and removed 3–4 days after surgery. The follow-up was over 6 months after removing the stent, using renal US, voiding cysto-urethrography and IVU or CT with contrast medium. US was used yearly and patients with a suspected obstruction had a diuretic renal scan or contrast CT.
Results
The mean (range) age of the patients was 27.4 (21–45) years, and 30 (30.6%) were men and 68 (69.4%) were women. We relied on the dye to diagnose an intraoperative IUI, and by passing a ureteric catheter from the bladder via the suspected site, because the operating room was not always equipped for an immediate radiological assessment to confirm the injury. In all 27 patients managed immediately (27.6%) the ureteric injury was always unilateral, and those with a partial injury with an intact distal supravesical segment (three) had an immediate repair over a JJ stent. In 17 patients the injury was complete or the ureter was obstructed by a haemostatic suture deep in the pelvis at the level of the uterine artery. Because it was not possible to de-ligate or dissect the distal ureteric segment a direct ureterovesical re-implantation (UVR) was done, using a submucosal tunnel due to the normal calibre of the injured ureter and healthy pliable vesical mucosa. In three patients the complete ureteric injury was higher, at the level of the superior vesical or common iliac vessels, and this was managed by re-implantation over a stent using a Boari bladder tube to substitute this defect. In four patients a direct water-tight, tension-free and stented ureteric re-anastomosis was made (). In all patients there was no significant morbidity apart from the increased operative duration and prolonged hospitalisation.
Table 2 Time of diagnosis and type of treatment.
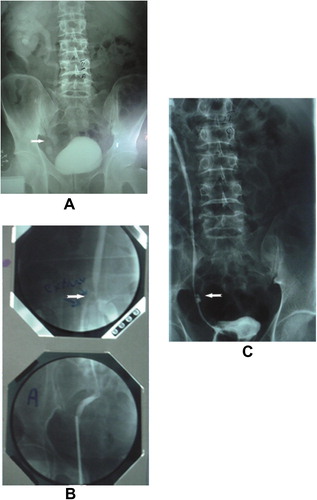
In all, 71 (72.4%) patients present late, with a urinary fistula in 58 (81.7%) after gynaecological, abdomino-pelvic and urological procedures in 48, six and four, respectively, compared with obstruction in 13 (18.3%) patients only after abdomino-pelvic surgery (). Some of those with a fistula were reported previously [Citation4], and here with an extended follow-up, in addition to new cases with different causes in the present study. Initial endoscopic treatment with radiological guidance to bypass the area of obstruction or the fistula was successful in 26 (36.6%) patients, with placement of a JJ stent up to the renal pelvis (). In 19 of the 58 patients with a fistula the stent was placed retrogradely using an 8.5 F ureteroscope in 16, and in three where this failed an antegrade JJ stenting from the PCN tract was successful. Seven of 13 patients with ureteric obstruction were managed by ureteroscopic dilatation and placing a stent.
Figure 1 (A) IVU after appendectomy with a dilated right ureter and urethrocutaneous fistula; (B) the steps of endoscopic treatment with retrograde dilatation; (C) postoperative stenting.
Patients in whom endoscopic treatment failed had open surgery for a ureteric fistula and obstruction in 39 and six, respectively, after gynaecological, abdominal and urological procedures in 32, nine and four cases. Direct UVR was used in 27 patients, with ureteric substitution using a Boari bladder tube or ileal substitution was used in 16 and two, respectively. The most common open surgical procedure for treating a IUI in early and late patients was UVR, in 44 of the 72 (61%) (), followed by substitutional procedures in 21 (29.2%) (), while in situ repair or re-anastomosis of the ureter was possible only in seven (9.8%; ).
Figure 2 (A, left; B, right). (A) Non-contrast CT of the abdomen and pelvis at 1 month after radical hysterectomy, with an obstructed left ureter and right uretero-vaginal fistula. (B) CT with contrast medium before a bilateral UVR re-implantation.
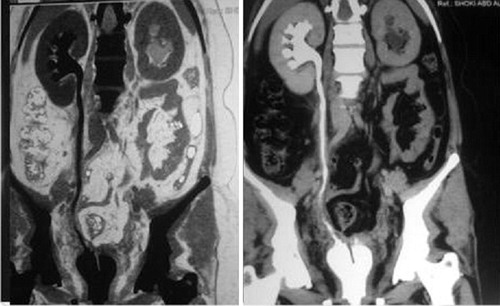
Figure 3 (A, left; B, right). (A) IVU at 16 weeks after a left oophorectomy, with an obstructed left ureter. (B) IVU 7 years after a Boari flap procedure.

Table 3 The type of open reconstructive procedure in early and late cases.
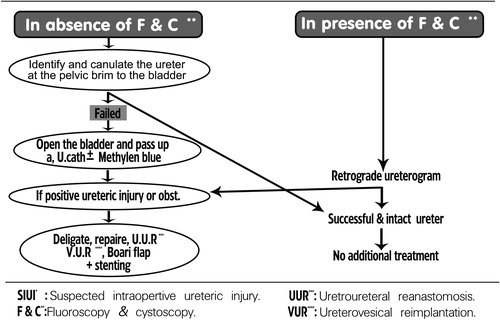
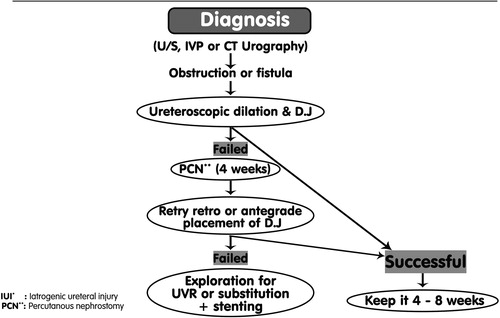
The initial radiological assessment 6 months after removal of the stents showed no complications, i.e., obstruction or reflux. All patients were evaluated regularly for ureteric patency and renal function annually, with a mean (range) follow-up of 46.6 (24.5–144) months, using US, IVU and contrast CT, or diuretic renal scintigraphy, according to a suspicion of obstruction or deterioration in renal function. There was a recurrent late obstruction that mandated a second intervention in six of 26 (23%) patients and 10 of 72 (14%), respectively, after endoscopic and open reconstruction as a primary treatment. These patients were managed by balloon dilatation and stenting, or open surgical procedures. There was postoperative reflux in only six (8.3%) patients after an open repair in early and late-managed cases, and this was managed by a recurrent long-term antibiotic programme in addition to selective α-blockers. The function of the renal units was stable during this long-term follow-up study, but for three in the late-diagnosis group (4.2%), who had a nephrectomy at 3, 5 and 12 years after an initial Boari bladder re-implantation, two episodes of endoscopic stenting in two patients, and intestinal substitution in one. and show our proposed algorithms followed during the management of early and late-diagnosed cases with IUI.
Discussion
The main concern in discussing IUIs is related to their prevention, to avoid major morbidity and complex reconstruction. This emphasis is related to the expectation of the surgeon during the dissection of structures close to the course of the normal-calibre ureter. However, trials to stop severe bleeding, with blind clamping or a suture around the uterine artery, are very common predisposing factors [Citation5].
As opposed to a bladder injury, which is almost always recognised during surgery, IUIs in many situations are difficult to identify intra-operatively and this requires a high index of suspicion, early recognition and immediate repair [Citation6]. As 70% of IUIs are unrecognised during surgery, any delay in the diagnosis increases the morbidity, with a deleterious effect on renal function [Citation3].
Most of these injuries (75%) are caused during gynaecological procedures, and in particular during 0.02–2% of abdominal hysterectomies [Citation7], 0.09% of emergency Caesarean sections [Citation8], compared to 0.3–10% with colorectal surgery [Citation9]. A limitation in the present study is the unequal number in each group and the variable degree of injury.
We were consulted intraoperatively for a suspected IUI in 27.6% of the present patients, over a long period. Most of these injuries occur after gynaecological surgery, followed by urological and abdominopelvic procedures in 60.2%, 25.6 and 14.3%, respectively, an incidence also reported by others [Citation10].
Our main concern is to identify the site and degree of injury, and after proper haemostasis we were able to repair the injury site in 11.1% of patients, or re-implant the proximal end of the completely torn ureter into the bladder via a water-tight, tension-free submucosal stented procedure in 63%. The prognosis and long-term results of this anti-reflux procedure were excellent, and the morbidity was minimal, because we re-implanted a normal healthy ureter into a healthy bladder with a pliable mucosa, using a suitable stent.
These types of IUIs are not often easily recognised during surgery, but anticipation and intraoperative vigilance, and consultation with a senior urologist, can reduce the risk and minimise prolonged morbidity and the need for a more complex reconstruction. The routine use of cystoscopy with either intravenous indigocarmine or a video monitor for stent placement has been considered by some authors, to reduce these ureteric injuries [Citation11].
In patients with a high-level injury, re-implantation into a bladder substitute was successful in 11.1%. The decision to use the distal ureter can incur more risk, as it was only successful in 14.8% due to entrapment of the distal segment by previous multiple sutures placed to stop bleeding around the uterine artery, with an ensuing difficult dissection to obtain a suitable length to substitute the gap.
However, many authors have used a distal segment of <5 cm, or even 2.5 cm, for end-to-end anastomosis to preserve the anti-reflux mechanism of the intravesical segment [Citation12].
By contrast with many other authors, our long-term results for the use of a Boari tube in acute IUI show that it is effective in patients with a short proximal ureter and a capacious bladder, that provides a long vesical tube to substitute up to the lower two-thirds of the ureter, with a tension-free submucosal anastomosis [Citation13,Citation14].
Cases of delayed recognition in the present study (72.4%) were mainly in patients with a urinary fistula or obstruction, in 81.7% and 18.3%, respectively. Minimally invasive ureteroscopic treatment with fluoroscopic guidance was used as a routine initial procedure, aiming for dilatation and bridging the ureteric defect with stenting, and this was successful as a definitive management in 36.6% of these cases. This was most successful in 42.9% after urological procedures, compared to 36% and 35.7% after gynaecological and abdominal surgery.
The stents were left in place for 3–4 months, although in some cases stenting was repeated during the follow-up to maintain ureteric continuity and preserve renal function. The endoscopic management of iatrogenic ureteric fistula has been reported previously, with success rates of 15–84% [Citation15,Citation16].
The results are better after endoscopic dilatation and stenting than after percutaneous diversion alone, aiming for spontaneous healing and guided canalisation with a lower risk of persistent fistula in 55% and ureteric stricture in 18% [Citation17,Citation18]. Therefore, percutaneous diversion alone is not a definitive treatment, but it relieves the symptoms of pain, fever and leakage, and it allows an earlier open surgical repair [Citation4].
In the present series, the endoscopic re-routing to the site of the fistula or obstruction was successful after either retrograde or antegrade dilatation and stenting, as reported in 14 of 25 patients (56%) by Koukouras et al. [Citation19] and 11 of 17 (64.7%) by Ja Hyeon et al. [Citation20]. However, the results of the noninvasive treatment of IUIs depend on many other factors, mainly the degree of interruption to ureteric continuity, the level of injury, and time of diagnosis. In a recent study by Al Otiabi [Citation21] the endoscopic placement of a ureteric stent alone was a successful management in seven of 20 patients (35%) with a ureterovaginal fistula and late diagnosis. Some of the successful results by other authors were reported after retrograde or antegrade ureteroscopy, using the ‘cut to the light’ technique. Moreover, five of the nine patients managed in this way developed a ureteric stricture within 5 months of the primary procedure, and this was corrected endoscopically [Citation22].
Whenever the endoscopic trials fail, a complex open reconstruction is mandatory to maintain the function of the renal unit. Previously we believed, with many others, that IUIs are better explored after 3–6 months from the time of initial injury, because many of these cases were referred or diagnosed late [Citation20]. Our long experience has shown that these patients can be explored after 4 weeks from PCN, with the suitable reconstruction procedure being selected according to the level of injury, evaluated from both an antegrade and/or retrograde ureterogram. The objectives of this short period of diversion are to resolve haemorrhagic and infection problems, to minimise the length of ureteric loss and stricture, prevent incontinence and preserve self-esteem, and to avoid obstruction, with its deleterious effect on renal function, before open reconstruction [Citation4].
As previously reported by others [Citation23], most of our late cases were repaired using vesical re-implantation (60%) or vesical substitution with a vesico-psoas hitch technique (35.5%), except in two patients (4.5%) with an injury below the pelvi-ureteric junction who had an intestinal substitution. The successful results of uretero-ureterostomy in 14.8% of early-diagnosed cases were not achieved in late cases, as in all these a suitable distal segment was not available for the anastomosis due to extensive deep pelvic fibrosis and adhesion from a previous fistula or haematoma. In a small series of nine patients with a ureterovaginal fistula, Lee et al. [Citation24] reported a successful uretero-ureterostomy in only four and the failure was attributed to extensive dissection and a difficult anastomosis.
In the present study the ureter was transected at the most healthy area above the lesion, making the procedure less difficult, the anastomosis more stable, and function over the period of follow-up, because we place the normal ureter into a healthy bladder with a water-tight, tension-free stented submucosal re-implantation.
In summary, with this rare injury and extended experience in management over a long period, we conclude that anticipating an IUI in certain surgical procedures, and consultation with a senior urologist for immediate management, were not associated with extra morbidity or loss of renal units. An immediate repair gives better long-term results. At least a third of the patients who are diagnosed late are managed definitively by ureteroscopic dilatation and stenting.
For patients where this fails, then diversion and a complex reconstruction after 4 weeks by an experienced urologist resulted in the loss of renal units in only 4.2% of the late group and 3% of the total series after a long follow-up from the devastating injury.
Conflict of interest
None.
Source of funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- T.H.LynchZ.L.Martine-PineiroE.PlasE.SerafetinidesL.Turkeriet alEAU guidelines on urological traumaEur. Urol.472005115
- S.BrandesM.CoburnN.ArmenakasJ.McAninchDiagnosis and management of ureteric injury an evidence based analysisBJU Int.942004277289
- S.P.ElliottJ.W.McAninchUreteral injuries. External and iatrogenicUrol. Clin. North Am.33200655
- S.El AbdG.GhoniemM.ElsharabyM.EmranA.El GamasyT.Felfelaet alUse of endoscopy in the management of post operative ureterovaginal fistulaInt. Urogynecol.81997185190
- J.H.HwangM.C.LimJ.Y.JoungS.S.SeoS.KangH.K.Seoet alUrologic complications & laparoscopic radical hysterectomy and lymphadenectomyInt. Urogynecol. J.23201216051611
- Y.OferB.JackL.PinhasUrologic injuries during cesarean section. Intraoperative diagnosis and managementJ. Urol.1722004196199
- A.HaestierR.SherwinUrologic complication following gynaecological surgeryObstet. Gynecol. Reprod. Med.2120101519
- D.RajasekarM.HallUrinary tract injuries during obstetric interventionBr. J. Obst. Gynaecol.1041997731
- J.MakeninJ.JohananssonC.TomasE.TamasP.K.HeinonenT.Laatikainenet alMorbidity of 10110 hysterectomies by type of approachHum. Reprod.16200114731478
- C.K.PayneUreteral injuries in females. Fistulas and obstructionS.RazFemale Urology1996WB SaundersPhiladelphia507520
- V.BabakC.RalphK.BrookeS.AbbasE.KarolynnG.Richardet alThe incidence of urinary tract injury during hysterectomy. A prospective analysis based on universal cystoscopyAm. J Obst. Gynecol.192200515991604
- P.SakellariouA.G.ProtopapasZ.VoulgarisN.KyritsisA.RodolakisG.Vlachoset alManagement of ureteric injuries during gynecologic operations: 10 years experienceEur. J. Obst. Gynecol. Reprod. Biol.1012002179184
- R.A.LeeVesicovaginal and ureterovaginal fistulaD.R.OstergardA.E.BentUrogynecology and Urodynamics3rd ed.1991Williams and WilkinsBaltimore296305
- J.W.UtrieBladder and ureteric injury. Prevention and managementClin. Obst. Gynecol.411998755763
- A.A.SelzmanJ.P.SpirnakE.D.KurshThe changing management of ureterovaginal fistulasJ. Urol.1531995626628
- R.F.LabaskyG.E.LeachPrevention and management of urovaginal fistulasClin. Obstet. Gynecol.331990382391
- N.T.SchmellerH.GottingerF.MarxPercutaneous nephrostomy as primary therapy of ureterovaginal fistulaUrol. A221983108112
- W.ThomasP.SanjeevC.PatrikTrauma to genitourinary tractSurgery28201073457352
- D.KoukourasT.PetasE.LiatsikosP.KallidonisE.K.SdralisG.Adonakiset alPercutaneous minimally invasive management of iatrogenic ureteral injuriesJ. Endourol.24201019211927
- K.U.Ja HyeonE.K.MinS.J.YoungK.L.NamH.P.YoungMinimally invasive management of ureteral injuries recognized late after obstetric and gynecologic surgeryInjury342003480483
- M.KhalidAl-OtaibiUreterovaginal fistulas. The role of endoscopy and percutaneous approachUrol. Ann.052012
- J.E.LingmanM.Y.WongJ.R.NewmarkEndoscopic management of total ureteral occlusion and uretrovaginal fistulaJ. Endourol.9221995391396
- A.C.WangUreteral injuries in obstetric and gynecologic proceduresJ. Gynecol. Surg.111995141145
- J.S.LeeJ.H.ChoeH.S.LeeJ.T.SeoUrologic complication following obstetric and gynecologic surgeryJ. Urol.532012795799