Abstract
Objective:
To assess the prediction of stone clearance and complications of percutaneous nephrolithotomy (PCNL) using the ‘STONE’ nephrolithometry score, assessing stone size, tract length (skin-to-stone distance), degree of obstruction, number of calyces involved and stone essence (density).
Patients and methods:
This was a prospective study of patients undergoing single-tract PCNL while prone, conducted at a university hospital. All patients had non-contrast-enhanced computed tomography within 3 weeks of the procedure. Only patients with a unilateral procedure and radio-opaque stones were included. The five variables of the STONE nephrolithometry score were calculated before the procedure. The stone-free rates were assessed with a plain abdominal film at 4 weeks and complications were graded using the modified Clavien system.
Results:
In all, 107 patients were included in the final analysis. Overall, 80% of patients were rendered stone-free. Among the individual variables, a larger stone (P = 0.002) and the involvement of multiple calyces (P = 0.04) were associated with residual stones, while tract length (skin-to-stone distance), stone density and presence of hydronephrosis were not. Patients who were rendered stone-free had a statistically significant lower overall STONE score than those with residual stones, at 7.24 vs. 8.14 (P = 0.02). The score also correlated with operative duration, which was significantly longer with a higher STONE score (P = 0.03). The complication rate was 18% and most complications were Clavien grade 2, with bleeding requiring a blood transfusion (11 patients) being the commonest. There were no deaths within 30 days of surgery, but there was no correlation between the STONE score and complications.
Conclusion:
The STONE nephrolithometry score is a simple and easy to apply system for predicting complexity in stone clearance with PCNL.
Introduction
Despite the availability of guidelines for managing urolithiasis there is no widely accepted standardised system for classifying stones in the upper urinary tract [Citation1]. With the marked increase in the incidence and prevalence of renal stones, the use of percutaneous nephrolithotomy (PCNL) is now considered as the standard treatment for large and complex renal stones [Citation2,Citation3].
Recently, Okhunov et al. [Citation4] proposed a novel quantitative scoring system which integrates five components measured from non-contrast-enhanced CT (NCECT) images before surgery to provide a picture of the complexity that can affect the percutaneous management of renal calculi. The stone score is calculated using five variables, abbreviated as an acronym ‘STONE’. These include stone size, tract length (skin-to-stone distance), degree of obstruction, number of calyces involved and stone essence (density). The scoring system can be used as a standard method for predicting the stone-free rate (SFR) after PCNL, and help in preoperative patient counselling, surgical planning and uniform academic reporting of the outcome. However, other investigators have not validated the study by Okhunov et al. [Citation4]. Thus we prospectively analysed and report the use of the STONE nephrolithometry score for evaluating the outcome of PCNL.
Patients and methods
This was a prospective study conducted by the section of Urology at the Aga Khan University Hospital, Karachi, Pakistan. An institutional review board approved the study, and all adult patients (>18 years) who underwent unilateral, single-tract PCNL for radio-opaque calculi, and had NCECT at our institute before surgery, were included. We excluded patients with radiolucent stones, bilateral renal stones, a history of previous surgery on the ipsilateral kidney, the presence of a nephrostomy tube or ureteric stent, active UTI, coagulopathy, skeletal deformity or special/abnormal anatomy of the upper tract (i.e., horseshoe kidney, PUJ obstruction, bifid or double system, etc.).
The demographic, clinical and operative data were collected and information including age, sex, body mass index (BMI), laterality, operative duration and hospital stay was prospectively collected. All patients had abdominal CT using a 64-slice machine (Aquilion, Toshiba Medical Systems, Shimoishigami, Otawara-Shi, Japan) within 3 weeks of PCNL, with 3-mm axial and reformatted 3-mm coronal sections evaluated on a picture-archiving computer system (View Pro-X version 4.0.6.2; Rogan-Delft, Veenendaal, Holland).
The CT variables proposed by Okhunov et al. [Citation4], i.e., stone size, tract length, degree and presence of obstruction (hydronephrosis), number of involved calyces and stone essence (density), were measured by one experienced radiologist. Each of the variables was scored according to the predefined system proposed by Okhunov et al., and the STONE nephrolithometry score calculated using the sum of individual variable scores.
All procedures were performed with the patient prone, using single-tract dilatation with Alken dilators under fluoroscopic guidance. The technique of PCNL was described earlier [Citation5]. Stones were fragmented using either the Lithoclast™ (Richard Wolf GmbH, Knittlingen, Germany), or simultaneous combined therapy with the Lithoclast and an ultrasonic lithotripter (Richard Wolf GmbH). The procedure was continued until no stone could be identified by both nephroscopic and fluoroscopic inspection. A flexible cystoscope (0°, 5 mm, 15 F, Karl Storz, Germany) and holmium-YAG laser (Lumenis Versapulse, 265 μm fibre) was used to access difficult locations. The patients were assessed for the presence of any residual stone by follow-up imaging with a plain abdominal film, and a stone-free status was defined as complete clearance, with no visible fragments or stone fragments of ⩽2 mm at 1 month after surgery.
Data were analysed statistically by univariate analysis, between stone-free and patients with residual stone. Student’s t-test was used to compare continuous variables and the chi-squared test for categorical variables. In all tests, P < 0.05 was considered to indicate significant differences. The primary outcome of the study was to determine the SFR and compare it with individual variables and the sum of the STONE score for clearance. The secondary outcome was to evaluate the ability of this scoring system to predict peri/postoperative complications within 30 days of the procedure. All complications were classified according to modified Clavien grading system.
Results
From April 2014 to September 2014, 167 patients were treated by PCNL and of these, 107 qualified for inclusion and were assessed in the final analysis. The mean (SD) age at presentation was 45.2 (17.5) years and the mean BMI was 27.5 (4.9) kg/m2. The study population comprised mainly men (62%) and the side of the procedure was almost equal. The patients’ demographics and stone characteristics evaluated for the STONE score are shown in .
Table 1 The demographic and clinical data of the 107 patients, and the stone characteristics used to calculate the STONE score.
Overall, 86 patients (80%) were rendered stone-free. Significantly many stones which were cleared were smaller than those that were not completely cleared. Among the individual variables, a larger stone (P = 0.002) and involvement of multiple calyces (P = 0.04) were associated with residual stones, while tract length, stone density and presence of hydronephrosis were not (). In all, 28% of patients had a longer tract (>100 mm), of whom nearly 87% were stone-free, compared to 80% of those with shorter tracts (<100 mm; P = 0.306). Nearly half of the patients had hydronephrosis but the stone clearance rate was almost equal between them and those with no hydronephrosis (P = 0.771). Nearly two-thirds of the patients had harder stones (>950 Hounsfield units) with a slightly lower SFR (78%) than the 85% in those with softer stones (<950 units; P = 0.35). Patients who were rendered stone-free had a statistically significantly lower overall STONE score than those with residual stones (P = 0.02). The score also correlated with the operative duration, being significantly longer with a higher STONE score (P = 0.03; ).
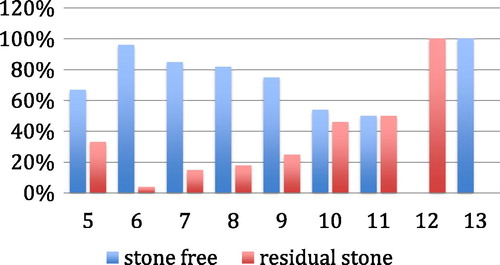
is a plot of the stone clearance rate with STONE score, and shows that rate decreased with increasing score, except for the overall score of 13 in one patient who had complete clearance.
Among patients with residual stones, six (29%) had additional treatments, with shock-wave lithotripsy in four and semi-rigid ureteroscopy and JJ stenting in one each. None of the patients had a repeat PCNL. Overall, 19 patients (18%) had peri/postoperative complications, including one of Clavien grade 1, 11 of Clavien grade 2, four of Clavien grade 3a, and three of Clavien grade 3b (). The most common complication was bleeding requiring a blood transfusion, in 11 patients. There were no deaths within 30 days of surgery, but there was no correlation between the STONE score and complications.
Table 2 Complications of PCNL classified according to modified Clavien grading system.
Discussion
In the general population the incidence of urolithiasis is 5–10%, and nearly 30% of the workload in an active urology department is related to treating urinary stones [Citation6]. For large and complex kidney stones PCNL is an important surgical intervention, and its success depends on several variables. Some of these can be predicted before surgery, i.e., stone burden and upper tract anatomy, but success also depends on surgical experience [Citation7].
To establish an accurate diagnosis and to determine the optimum treatment and surgical planning, preoperative imaging is a critical step [Citation8]. CT has become the leading imaging method for urolithiasis, providing high-resolution spatial imaging along with multi-planar reconstruction for the accurate determination of stone complexity, i.e., size and distribution, pelvi-calyceal anatomy and anatomical relationship with other structures, hence contributing to surgical planning [Citation9,Citation10].
Several scoring systems have been developed for predicting the SFR after shock-wave lithotripsy, retrograde intrarenal surgery and PCNL [Citation11,Citation12]. These have incorporated different variables that can influence success rates, but the imaging methods on which these systems are developed show some inconsistencies [Citation13].
The scoring systems in contemporary use for predicting the outcome of PCNL are Guy’s stone score, the STONE nephrolithometry score, the Clinical Research Office Of Endo-Urological Society (CROES) nephrolithometric nomogram, and staghorn morphometry. These have attempted to incorporate important variables in an efficient and simple manner to quantify renal stone complexity [Citation13]. An optimal scoring system should be quick, simple, reproducible and easily implemented, and must have a good correlation with SFRs and complications [Citation14]. It also helps to define the complexity of the stone, and benefit not only patient counselling, but also auditing, training and revalidation, and comparison between different centres, surgeons and techniques by uniform and standardised reporting [Citation15–Citation18].
The Guy’s score and CROES nomograms were initially developed using abdominal plain films, while the staghorn morphometry score and STONE score were developed on the basis of CT findings of variables that can be obtained specifically from CT. The Guy’s stone score includes stone number, location, presence of staghorn stones and abnormal anatomy to determine different grades, and it was reported that the SFR declined with increasing grades of complexity [Citation14]. Mishra et al. [Citation19] proposed a classification system for staghorn stones using the stone volume and its distribution in the collecting system. This ‘staghorn morphometry’ requires CT urography and CT-based volumetric assessment software that is complex to adapt. This was done to improve the prediction of efficacy, reduce the morbidity, and to plan PCNL with respect to the requirement for tracts and stage(s) of PCNL. By contrast, Smith et al. [Citation7], based on a multivariate analysis, reported a nephrolithometric nomogram (CROES) that also takes into account patient and surgeon factors, i.e., previous surgery and the case volume of surgeons.
Okhunov et al. [Citation4] developed and validated the STONE score from preoperative NCECT, based on a Medline review of English-language studies from 1976 to 2012 and identifying clinically relevant variables affecting the outcomes of PCNL. This scoring system was externally validated in a multi-institutional study with 850 patients, and showed that the model was significantly associated with the SFR, overall complication rate, estimated blood loss, operative duration and length of hospital stay [Citation20]. In contrast to the other scoring systems, the STONE score uses variables that are easy to calculate, derived from NCECT (most common diagnostic method used for evaluating patients with stone) and requires no specialised software.
In the present study, tract length, BMI and the degree of obstruction were not associated with a lower SFR. Others have reported that patients with a greater BMI and consequently longer tract (skin-to-stone distance) will be technically challenging, and this could affect the peri-operative variables.
Zhu et al. [Citation21], in a multivariate analysis, showed that greater obstruction and consequent hydronephrosis lead to lower success rates. This variable was not significant in the present study, because although stone fragments might migrate and scatter from the original sites to the other remote areas of the collecting system, a dilated system is also easy to puncture.
The present patients were different from those assessed by Okhunov et al. [Citation4], being younger and with a higher mean STONE score of 7.24, compared to 6.8 in their stone-free group, but a lower score of 8.14 vs. 9.7 in those with residual stone. The mean operative duration in the stone-free group was comparable to that reported by Okhunov et al., but it was shorter in those with residual stone. The complication rates were comparable.
Okhunov et al. [Citation4] reported the STONE score to be highly predictive of the SFR, with an accuracy of 83.1% that was greater than any of the other individual variables. Similarly, in another study, Okhunov et al. [Citation22] reported an excellent interobserver reliability of the STONE system among medical students, urology residents, fellows and attending urologists.
We did not determine the accuracy of the score, nor did we assess the interobserver reliability, but we found this scoring system to correlate with the SFR, with lower scores predicting the likely probability of stone clearance. Although the difference between mean STONE score of the stone-free and residual-stone group was significant, it was small (<1 point). Similarly, a higher STONE score, with a more complex procedure, was correlated with a longer operation; it was not reflected in a greater likelihood of complications.
The CROES PCNL global study reported a success rate of 75.5% and a complication rate of 20.5% [Citation3]. They proposed that a higher stone burden, and complexity, are associated with lower SFRs and higher complication rates. Our results are comparable with these results. The overall complication rate of 18% is comparable to contemporary series and most complications were minor (Clavien grade 1 and 2). There was bleeding requiring transfusion in 10% of patients, higher than the 5.7% reported in a multicentre study by CROES [Citation3]. The possible reason for this higher transfusion rate could be a lower baseline haemoglobin level and consequently a lower reserve and threshold for transfusion. One of the most devastating complications of PCNL is injury to surrounding organs, most commonly large bowel injury [Citation23].
The main limitation of the present study was the relatively few patients included. For this reason, the vast majority of the patients (79 of 107) can be sub-classified into those with a ‘moderate complexity score of 6–8’, according to the study of Okunov et al. [Citation4], while only nine and 19 could be sub-classified into the ‘low complexity’ score of 3–5 and ‘high complexity’ score of 9–13, respectively. This might also explain why the difference between the stone-free patients and those with residual stone was <1 point. Interestingly, the low-complexity group had a SFR of 67%. This could be related to the expertise of three different urologists performing the procedure. However, this factor was not separately assessed in the present study. It was a single-centre study done within a short period with few patients. There was no correlation between the prevalence of complications and the STONE score, possibly because there were too few patients. A larger-scale multi-centre study should be undertaken to validate and confirm our results.
In conclusion, the STONE score is a simple and easy to apply system for predicting the complexity of the stone for PCNL, and stone clearance. Prospective studies with a larger sample are required to further confirm these findings.
Conflict of interest
None.
Source of funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
✰ This journal is partially supported by Karl Storz GmbH. That support had no influence on the peer-review of this paper, which was entirely independent of Karl Storz.
References
- M.S.ChooC.W.JeongJ.H.JungS.B.LeeH.JeongH.Sonet alExternal validation and evaluation of reliability and validity of the S-ReSC scoring system to predict stone-free status after percutaneous nephrolithotomyPLoS One92014e83628
- European Association of Urology. Turk C, Knoll T, Petrik A, et al. EUA Guidelines on Urolithiasis. Available at <http://uroweb.org/guideline/urolithiasis/> [accessed June 2015].
- J.de la RosetteD.AssimosM.DesaiJ.GutierrezJ.LingemanR.Scarpaet alThe clinical research office of the endourological society percutaneous nephrolithotomy global study: indications, complications, and outcomes in 5803 patientsJ Endourol2520111117
- Z.OkhunovJ.I.FriedlanderA.K.GeorgeB.D.DutyD.M.MoreiraA.K.Srinivasanet alSTONE nephrolithometry: novel surgical classification system for kidney calculiUrology81201311541159
- N.HaroonS.M.NazimM.H.AtherOptimal management of lower polar calyceal stone 15–20 mmKorean J Urol542013258262
- C.W.JeongS.J.JeongS.K.HongS.B.LeeJ.H.KuS.S.Byunet alNomograms to predict the pathological stage of clinically localized prostate cancer in Korean men: comparison with western predictive tools using decision curve analysisInt J Urol192012846852
- A.SmithT.D.AverchK.ShahrourD.OpondoF.P.DaelsG.Labateet alA nephrolithometric nomogram to predict treatment success of percutaneous nephrolithotomyJ Urol1902013149156
- D.MagrillU.PatelK.AnsonImpact of imaging in urolithiasis treatment planningCurr Opin Urol22013158163
- P.F.FulghamD.G.AssimosM.S.PearleG.M.PremingerClinical effectiveness protocols for imaging in the management of ureteral calculous disease: AUA technology assessmentJ Urol189201312031213
- M.E.LipkinG.M.PremingerImaging techniques for stone disease and methods for reducing radiation exposureUrol Clin North Am4020134757
- J.D.WiesenthalD.GhiculeteA.A.RayR.J.HoneyK.T.PaceA clinical nomogram to predict the successful shock wave lithotripsy of renal and ureteral calculiJ Urol1862011556562
- B.ResorluA.UnsalH.GulecS.S.OztunaA new scoring system for predicting stone-free rate after retrograde intrarenal surgery: the ‘Resorlu-Unsal stone score’Urology802012512518
- K.LabadieZ.OkhunovA.AkhaveinD.MoreiraJ.Moreno-PalaciosM.Del Juncoet alEvaluation and comparison of urolithiasis scoring systems in percutaneous kidney stone surgeryJ Urol1932014154159
- K.ThomasN.C.SmithN.HegartyJ.M.GlassThe Guy’s stone score – grading the complexity of percutaneous nephrolithotomy proceduresUrology782011277281
- M.De SioG.AutorinoF.QuartoF.CalabròR.DamianoF.Giuglianoet alModified supine versus prone position in percutaneous nephrolithotomy for renal stones treatable with a single percutaneous access: a prospective randomized trialEur Urol542008196203
- J.J.de la RosetteM.P.LagunaJ.J.RassweilerP.ConortTraining in percutaneous nephrolithotomy: a critical reviewEur Urol5420089941003
- D.AllenT.O’BrienR.TiptaftJ.GlassDefining the learning curve for percutaneous nephrolithotomyJ Endourol192005279282
- A.G.PapatsorisT.ShaikhD.PatelA.BourdoumisC.BachN.Buchholzet alUse of a virtual reality simulator to improve percutaneous renal access skills: a prospective study in urology traineesUrol Int892012185190
- S.MishraR.B.SabnisM.DesaiStaghorn morphometry. A new tool for clinical classification and prediction model for percutaneous nephrolithotomy monotherapyJ Endourol262012614
- Z.OkhunovD.MoreiraA.Georgeet alMulticenter validation of STONE nephrolithometryJ Urol1912015e839
- Z.ZhuS.WangQ.XiJ.BaiX.YuJ.LiuLogistic regression model for predicting stone-free rate after minimally invasive percutaneous nephrolithotomyUrology7820113236
- Z.OkhunovM.HelmyA.Perez-LansacA.MenhadjiP.BucurS.B.Kollaet alInterobserver reliability and reproducibility of S.T.O.N.E. nephrolithometry for renal calculiJ Endourol27201313031306
- S.KachrilasA.PapatsorisC.BachS.KontosZ.FaruquzA.Goyalet alColon perforation during percutaneous renal surgery: a 10-year experience in a single endourology centreUrol Res402012263268