Abstract
Objectives:
To assess the probability of spontaneous stone passage and its predictors after drainage of obstructed kidney by JJ stent, as insertion of an internal ureteric stent is often used for renal drainage in cases of calcular ureteric obstruction.
Patients and methods:
Between January 2011 and June 2013, patients for whom emergent drainage by ureteric stents were identified. The patients’ demographics, presentation, and stone characteristics were reviewed. The primary endpoint for this study was stone-free status at the time of stent removal, where all patients underwent non-contrast spiral computed tomography (NCCT) before stent removal. Ureteroscopic stone extraction was performed for CT detectable ureteric stones at the time of stent removal. Potential factors affecting the need for ureteroscopic stone extraction at the time of stent removal were assessed using univariate and multivariate statistical analyses.
Results:
Emergent ureteric stents were undertaken in 196 patients (112 males, 84 females) with a mean (SD) age of 53.7 (16.2) years, for renal obstruction drainage. At the time of stent removal, 83 patients (42.3%) were stone free; with the remaining 113 patients (57.7%) undergoing ureteroscopic stone extraction. On multivariate analysis, stone width [odds ratio (OR) 15.849, 95% confidence interval (CI) 2.83; P = 0.002) and radio-opaque stones (OR 12.035, 95% CI 4.65; P < 0.001) were independent predictors of the need for ureteroscopic stone extraction at the time of stent removal.
Conclusion:
Spontaneous ureteric stone passage is possible after emergent drainage of an obstructed kidney by ureteric stenting. Stone opacity, larger stone width, and positive preoperative urine culture are associated with a greater probability of requiring ureteroscopic stone extraction after emergent drainage by ureteric stenting.
Introduction
Emergent drainage of obstructed kidneys is needed in cases of ureteric calculi causing uraemia or sepsis. This obstruction can be relieved by placement of a nephrostomy tube (percutaneous nephrostomy, PCN) or a ureteric stent. Insertion of a JJ stent is often used for urgent decompression of obstructed kidneys secondary to calcular ureteric obstruction. The impact of stent insertion on ureteric peristalsis is not clear. The effect of ureteric stent insertion on ureteric peristalsis was experimentally studied in a porcine model and stent insertion was associated with an initial increase in peristaltic activity, which was followed by a decrease or arrest of peristalsis [Citation1].
Other clinical and experimental studies have shown that ureteric stents are associated with ureteric dilatation, diminished ureteric peristalsis, and impaired stone passage [Citation2-Citation5]; however, spontaneous stone passage is not an infrequent event after ureteric stent insertion.
After urgent decompression by ureteric stenting for an acutely obstructed kidney, an additional procedure is often necessary for the ureteric stone. However, it is not clear which stones in which patients will require further treatment, i.e. those stones that will pass or disappear after ureteric stenting. In the present study, we assessed the probability of spontaneous stone passage and its predictors after urgent drainage of acutely obstructed kidney by ureteric stenting.
Patients and methods
Data were retrospectively collected for patients who underwent emergent ureteric stent placement for drainage of calcular ureteric obstruction between January 2011 and June 2013. Patients were classified into two groups: patients in the first group were stone-free on non-contrast spiral CT (NCCT) and in the second group ureteric stones were still present. Ureteroscopic stone extraction was performed for ureteric stones detected by CT at the time of stent removal.
Study population
Patients that presented at the Emergency Room with an acutely obstructed kidney and were eligible for emergent drainage were assessed. A ureteric stent was inserted for uraemic patients with obstructed solitary (functional or anatomical) or bilateral obstructed kidneys. A ureteric stent was inserted for sepsis whenever an obstructed kidney was associated with two or more of the systemic inflammatory response syndrome (SIRS) criteria [Citation6]. In patients with PCN tube drainage, an active primary ureteroscopic stone treatment was attempted and patients who were managed by ESWL or percutaneous nephrolithotomy were excluded from the study.
Intervention
On presentation, patients were assessed by history, physical examination, urine analysis, midstream urine culture (MSUC), serum creatinine, blood electrolytes, and leucocytic count. NCCT of the urinary tract was performed for all patients at presentation. The stone size was measured in two dimensions, i.e. the stone length and width. The stone surface area was calculated using the formula, surface area = length × width × π × 0.25 [Citation7].
A single preoperative i.v. dose of third generation cephalosporin was given. Cystoscopic insertion of the JJ stent (Percuflex, Boston Scientific) was performed under regional anaesthesia with fluoroscopic control. The ureteric stent was inserted over a hydrophilic guidewire to allow safe bypassing of the obstructed ureteric segment and a 16 F urethral catheter was fixed for 24 h to allow free drainage of the obstructed kidney.
Post-intervention evaluation
Serum creatinine, blood electrolytes and blood count were repeated the next morning. Once the serum creatinine and/or leucocytic count began decreasing, patients were discharged. Patients were advised to drink plenty of fluids and for those with lucent stones to take urine alkalisers, e.g. potassium sodium hydrogen citrate. Patients were followed up at 2-week intervals after stent insertion in the outpatient clinic until stabilisation of serum creatinine (nadir level) and resolution of sepsis (SIRS). Once stable, NCCT was booked to plan further treatment and a time for ureteric stent removal.
For detectable stones at NCCT, either in the ureter or relocated to the kidney, retrograde ureteroscopy (URS; semi-rigid or flexible) was performed accordingly.
In patients who were stone free at NCCT the ureteric stent was removed and they were followed by renal ultrasonography for any residual hydronephrosis. For recurrent symptoms after JJ stent removal or persistent hydronephrosis, NCCT was repeated.
A spiral 64-detector row CT scanner (Light-Speed Plus, General Electric, Milwaukee, WI, USA) was used with 5-mm thickness scanning. For measurement of the stone attenuation value (stone density) and surface area, the post-scanning bone window protocol was used. An independent radiologist read the CT images.
Outcome measures
The primary endpoint of this study was stone-free status at the time of ureteric stent removal, where all patients underwent NCCT before stent removal. Ureteroscopic stone surgery was performed for CT-detectable ureteric stones at the time of ureteric stent removal. Potential factors affecting stone-free status at the time of ureteric stent removal were assessed using univariate and multivariate models. Patients were stratified into two groups, group A; stone-free and group B; persistent stone for URS.
Statistical analysis
Fisher’s exact and chi-square tests were used for comparing categorical variables, and the Mann–Whitney U-test and independent samples t-test were used to compare continuous variables when appropriate. A multivariate model (logistic regression analysis with backward elimination using the likelihood ratio) was used to identify independent predictors for stone-free probability at the time of ureteric stent removal. The Receiver operating characteristic (ROC) curve was used whenever indicated for assessment of significant predictors. Statistical analysis was performed using SPSS® version 20 statistical software program, with a P < 0.05 considered to indicate statistical significance.
Results
In all, 196 patients (196 renal units) were included during the specified period. After a median (range) of 3 (0.5–6.3) months from ureteric stent insertion, 83 patients (42.3%) were free of stones at NCCT and underwent ureteric stent removal only (group A). The remaining 113 patients (57.7%) underwent removal of the ureteric stent and ureteroscopic stone surgery (group B). There was no significant difference between the groups for patients’ body mass index (BMI), sex, presence of diabetes mellitus and hypertension, morbidity score, grade of preoperative hydronephrosis, serum uric acid level, blood haemoglobin, and stone location in the ureter ( and ).
Table 1 Potential categorical factors associated with stone-free status at time of JJ stent removal.
Table 2 Potential continuous factors associated with stone-free status at time of JJ stent removal.
However, most of the patients with a positive preoperative MSUC 37/52 (71.2%), radiopaque stones 89/114 (78.1%), sepsis at presentation 57/78 (73.1%) and significantly greater stone width, length, stone surface area and density, were in group B. Older patients and patients with solitary kidney 52/99 (52.5%), higher BMI, and longer ureteric stent duration were more likely to have a stone-free status (group A) ( and ).
Among group A, after ureteric stent removal, residual hydronephrosis or recurrence of symptoms were reported in 27 patients (32.5%) for whom NCCT confirmed stone-free status after a median (range) of 6 (4–9) weeks from stent removal. No secondary intervention was needed for ureteric stones among group A.
Prediction of stone-free status at time of JJ stent removal
In the final model (), a smaller preoperative stone width [odds ratio (OR) 1.36, 95% CI 1.01–1.8; P = 0.038) and stone surface area (OR 0.72, 95% CI 0.5–0.9; P = 0.007), negative preoperative MSUC (OR 3.3, 95% CI 1–10.7; P = 0.046), and lucent stones (OR 11.3, 95% CI 3.4–37.3; P < 0.001) were significantly associated with a greater stone-free probability at the time of JJ stent removal.
Table 3 Multivariate assessment of potential factors for the need of URS at the time of ureteric stent removal.
ROC curve for stone width and surface area associated with stone-free status
The threshold for stone width associated with a lesser probability of requiring URS for stone extraction was 6.5 mm (61% sensitivity, 71% specificity, OR 0.4, 95% CI 0.22–0.71; P = 0.002; ).
Figure 1 ROC curve for significant continuous predictors of stone free probability at time of JJ stent removal for stone width (A) and stone surface area (B).
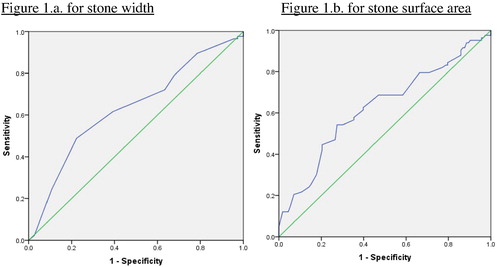
The threshold for stone surface area associated with a lesser probability of requiring URS for stone extraction was 12.3 mm (56% sensitivity, 35% specificity, OR 0.4, 95% CI 0.22–0.71; P = 0.003; ).
Discussion
Despite being frequently employed, the stone-free rate status after emergent ureteric stent fixation for an obstructing ureteric calculi and the need for additional URS at the time of stent removal need to be assessed.
Patients presenting with sepsis or uraemia are candidates for emergent renal drainage. Renal decompression by either insertion of a nephrostomy tube (PCN) or a ureteric stent for an acutely obstructing ureteric stone is a reasonable option. The impact of both PCN and ureteric stenting on the probability of spontaneous passage of ureteric stone has been studied in a canine model. Artificial stone insertion into both upper ureters was performed in 20 dogs; a ureteric stent was left at one side and PCN tube on the contralateral side. Compared with PCN, ureteric stents were associated with ureteric dilatation, reduced peristalsis, and impaired stone passage [Citation3,Citation8].
These manoeuvres can offer a prompt relief of pain, sepsis, and uraemia and they are usually followed by definitive treatment either by URS or ESWL [Citation9]. URS is safe, effective and seems to be the superior treatment option compared with ESWL for treating ureteric stones after initial decompression of acutely obstructed kidneys [Citation10]. After decompression of the obstructed kidney and general stabilisation of the condition, re-evaluation of the stone location and characteristics should be done for planning of the next step in treatment. NCCT allows identification of the stone with a sensitivity of 94–100% and accuracy of 93–98%, as well as identify signs of acute kidney obstruction [Citation11].
In a study of 256 URS for ureteric stones, 9.8% were negative. Smaller stone width was the independent predictor of negative URS [Citation12]. Insertion of ureteric stents after URS is not infrequent, as they seem useful to prevent the postoperative colic that may result from the passage of residual stones/debris; however, they might be associated with some discomfort and other urinary symptoms [Citation13–Citation15].
Data have shown that ureteric stents are associated with diminished ureteric peristalsis and probably cause impaired stone passage [Citation3], especially with longer durations of stenting of >2 months [Citation5,Citation16]. Although routine stent placement is not necessary before all ureteroscopic procedures, URS which is preceded by ureteric stenting is associated with higher stone-free rates and few complications vs URS not preceded by ureteric stenting [Citation17].
In the present study, in 83 of 196 patients (42.3%) their obstructing ureteric stone had disappeared by the time of ureteric stent removal. Smaller preoperative stone width, lucent stones, and negative preoperative negative MSUC were associated with a lesser probability of requiring URS stone surgery. In the present cohort, 71.2% of the patients with positive MSUCs had persistent stones and underwent URS. The presence of significant UTI might impair ureteric peristalsis and might even be associated with ureteric oedema, which may hinder stone passage.
In an obstructed kidney with a ureteric stone, a ureteric stent might pass beside the stone or cause stone disimpaction and relocation to the kidney, and may fragment friable stones on its way to the renal pelvis. However, immediate imaging after stenting was not available in the present cohort. The exact mechanism by which the stone disappeared in 42.3% of the study patients is not clear. Dissolution of stones, especially for patients on proper alkalisation treatment is favoured by the fact that 69.9% of stones were lucent in the stone-free group. Conversely, spontaneous stone passage might represent another mechanism particularly for small stones. A threshold stone width of 6.4 mm was identified as an independent predictor for stone-free status at the time of ureteric stent removal. The propensity of spontaneous passage of a ureteric stone is significantly reduced with stone diameters of >6.4 mm with up to 99% likelihood of eventual need for intervention [Citation18]. Lumma et al. [Citation19] reported that ureteric stent placement before URS for stone treatment has no positive or negative impact on stone-free status. Reduction of ureteric motility is always claimed as the cause of hindered stone passage with internal ureteric stenting. However, the new introduction of α-blockers as medical expulsive therapy for ureteric stones is based on the theory that these medications inhibit contractions of the ureteric musculature, reduce basal tone, and decrease peristaltic frequency [Citation20]. However, Pickard et al. [Citation21] reported that tamsulosin 400 μg and nifedipine 30 mg taken daily for up to 4 weeks was not effective at decreasing the need for further treatment to achieve stone clearance in patients with expectantly managed ureteric colic. Accordingly, an internal ureteric stent with a reduction in ureteric peristalsis may be associated with a greater propensity for the spontaneous passage of smaller stones.
Finally, for acute calcular ureteric obstruction in certain conditions, namely lucent stone and stone widths of <6.5 mm, surface area of <12.3 mm, stenting of the ureter is a valid less invasive alternative to primary treatment. Furthermore, patients could be counselled that they might not need further treatment and only stent removal would be the next step after proper imaging with NCCT.
The main limitations of our present study are inherent to its retrospective nature, with data lacking on the adjuvant treatment received including urine alkaliniser and α-blockers, where they might be confounders for stone-free probability. However, to the best of our knowledge this is the largest study addressing this issue and further prospective studies are encouraged.
In conclusion, spontaneous ureteric stone passage is possible after drainage of an obstructed kidney by ureteric stenting. A negative preoperative MSUC, lucent stones with smaller widths and surface areas are associated with a lesser probability of requiring ureteroscopic stone extraction after emergent drainage by ureteric stenting.
Conflict of interest
The authors declare that they have no conflict of interest.
Source of Funding
None.
Informed consent
Informed consent was obtained.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- R.VenkateshJ.LandmanS.D.MinorD.I.LeeJ.RehmanR.Vanlangendoncket alImpact of a double-pigtail stent on ureteral peristalsis in the porcine model: initial studies using a novel implantable magnetic sensorJ Endourol192005170176
- I.S.MudraiaS.S.ZenkovA.G.MartovV.I.KirpatovskiĭThe effect of ureteral stents on the peristalsis of the upper urinary tractsUrol Nefrol (Mosk)519983135
- G.M.LennonJ.A.ThornhillR.GraingerT.E.McDermottM.R.ButlerDouble pigtail ureteric stent versus percutaneous nephrostomy: effects on stone transit and ureteric motilityEur Urol3119972429
- Qi DF, Wu KJ, Li X, Shan ZC, Xia MY, Guo B, et al. [Effects of ureteral stents on rabbit upper urinary tract urodynamics]. Di Yi Jun Yi Da Xue Xue Bao 2004;24:1260-2.
- P.C.RyanG.M.LennonP.A.McLeanJ.M.FitzpatrickThe effects of acute and chronic JJ stent placement on upper urinary tract motility and calculus transitBr J Urol741994434439
- F.M.WagenlehnerA.PilatzW.WeidnerUrosepsis – from the view of the urologistInt J Antimicrob Agents38Suppl.20115157
- M.H.AtherS.M.NazimM.N.SulaimanEfficacy of semirigid ureteroscopy with pneumatic lithotripsy for ureteral stone surface area of greater than 30 mm2J Endourol232009619622
- A.SkolarikosG.AlivizatosA.PapatsorisK.ConstantinidesA.ZerbasC.DeliveliotisUltrasound-guided percutaneous nephrostomy performed by urologists: 10-year experienceUrology682006495499
- R.AutorinoL.OsorioLima E.A.ReChristianSeitzEnisTanovicZeljkoKikicet alRapid extracorporeal shock wave lithotripsy for proximal ureteral calculi in colic versus noncolic patientsEur Urol52200712641265 author reply 1265-6
- T.KannoA.MatsudaH.SakamotoY.HigashiH.YamadaSafety and efficacy of ureteroscopy after obstructive pyelonephritis treatmentInt J Urol202013917922
- L.Dalla PalmaR.Pozzi-MucelliF.StaculPresent-day imaging of patients with renal colicEur Radiol112001417
- J.E.KreshoverR.J.DicksteinC.RoweR.K.BabayanD.S.WangPredictors for negative ureteroscopy in the management of upper urinary tract stone diseaseUrology782011748752
- H.B.JoshiN.NewnsA.StainthorpeR.P.MacDonaghF.X.KeeleyJrA.G.TimoneyUreteral stent symptom questionnaire: development and validation of a multidimensional quality of life measureJ Urol169200310601064
- C.LeeM.KuskowskiJ.PremoliN.SkempM.MongaRandomized evaluation of ureteral stents using a validated symptom questionnaireJ Endourol192005990993
- H.B.JoshiA.StainthorpeR.P.MacDonaghF.X.KeeleyJrA.G.TimoneyM.J.BarryIndwelling ureteral stents: evaluation of symptoms, quality of life and utilityJ Urol169200310651069
- U.PatelM.J.KellettUreteric drainage and peristalsis after stenting studied using colour Doppler ultrasoundBr J Urol771996530535
- R.A.RubensteinL.C.ZhaoS.LoebD.M.ShoreR.B.NadlerPrestenting improves ureteroscopic stone-free ratesJ Endourol21200712771280
- J.M.TeichmanClinical practice. Acute renal colic from ureteral calculusN Engl J Med3502004684693
- P.P.LummaP.SchneiderA.StraussK.D.PlotheP.ThelenR.H.Ringertet alImpact of ureteral stenting prior to ureterorenoscopy on stone-free rates and complicationsWorld J Urol312013855859
- K.DavenportA.G.TimoneyF.X.KeeleyA comparative in vitro study to determine the beneficial effect of calcium-channel and alpha(1)-adrenoceptor antagonism on human ureteric activityBJU Int982006651655
- R.PickardK.StarrG.MacLennanT.LamR.ThomasJ.Burret alMedical expulsive therapy in adults with ureteric colic: a multicentre, randomised, placebo-controlled trialLancet3862015341349
