Abstract
Objective:
To compare outcomes of the Mathieu incised-plate (Mathieu-IP) technique vs the standard tubularised incised-plate (TIP) technique for primary management of distal hypospadias.
Patients and methods:
Between April 2012 and August 2015, 66 patients (aged 15–60 months) with primary distal hypospadias were randomly allocated to two groups. Group 1 included 34 patients who underwent Mathieu-IP repair and Group 2 included 32 patients managed using the TIP technique for primary management of distal hypospadias. Postoperatively, all patients were examined weekly up to 1 month and then at 3 and 6 months. Perioperative data, complications and outcomes of both procedures were statistically analysed and compared.
Results:
There were no statistically significant differences in patient demographics between the groups at baseline. There was no statistically significant difference in the mean (SD) operative time between Groups 1 and 2, at 95 (7.6) and 91.2 (8.1) min, respectively. There was no statistically significant difference in the shape of the urine stream at micturition or the neomeatus between the groups postoperatively. The rate of postoperative fistula was significantly higher in Group 2 (TIP) compared to Group 1 (Mathieu-IP), at 18.7% vs 2.9% (P = 0.004). There was no postoperative meatal stenosis in Group 1, which did occur in five patients (15.6%) in Group 2 (P = 0.002).
Conclusion:
The Mathieu-IP technique appeared to be better than the standard TIP technique with regard to postoperative fistula formation and meatal stenosis, and with acceptable cosmesis.
Abbreviations:
Introduction
About 80% of patients with hypospadias have their orifices in the coronal and subcoronal positions [Citation1]. Many surgical repair techniques have been practiced by many surgeons for correction of hypospadias anomaly. There are two methods that have been widely used, perimeatal-based flap (Mathieu) and tubularised incised-plate (TIP) urethroplasty [Citation2]. The major disadvantage of Mathieu technique is that the horizontal, rounded meatus is less acceptable than the slit-like meatus of the TIP technique. In the last two decades the Mathieu procedure has become less popular than TIP and this may be due to the simplicity and the good cosmetic slit-like final appearance of the meatus of the TIP technique [Citation3]. The drawbacks of TIP urethroplasty are the relatively high incidence of urethrocutaneous fistula (0–33%) and also meatal stenosis that necessitate regular dilatation; these complications are more challenging with narrow urethral plates and flat shallow glans [Citation4,Citation5]. A modification of the classic Mathieu technique, by adding incision of the urethral plate including the native hypospadias orifice, enhance the benefits of using this technique in hypospadias with a narrow original meatus and improving cosmesis [Citation6,Citation7].
In the present prospective randomised study, we assessed the benefits of the Mathieu incised-plate (Mathieu-IP) technique in improving outcomes and cosmesis in comparison with the standard TIP technique.
Patients and methods
The study was conducted between April 2012 and April 2015 on patients with primary distal hypospadias (coronal, sub-coronal, distal penile), after approval of the Local Ethics Committee of Benha Faculty of Medicine and obtaining informed written consents from the parents of the children.
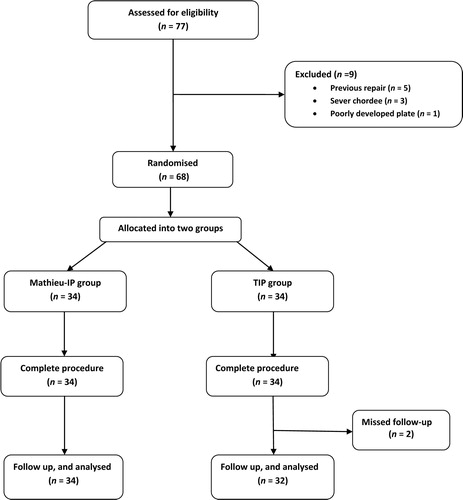
The details of study flow are shown in . In all, 77 patients with distal hypospadias (coronal, sub-coronal, distal penile) presented to the outpatient clinic and were eligible to be enrolled. We excluded nine patients for the following reasons: presence of severe chordee in three, previous hypospadias surgery in five, and a poorly developed urethral plate in one. The remaining 68 patients were randomly divided using the sealed-envelope method into two groups. Group 1, included 34 patients who were managed by the Mathieu procedure plus incision of the urethral plate (Mathieu-IP); and Group 2, included 34 patients who underwent TIP urethroplasty (Snodgrass procedure). All patients in both groups completed the procedure (see ).
The postoperative functional assessment and cosmetic evaluation was carried out by medical personnel other than the surgeons and by the parents at the follow-up visits and included: the site of the new meatus; calibre and force of the stream; and the presence of complications in the form of urethral cutaneous fistula, meatal stenosis, glandular dehiscence, haematoma, infection, and disruption of the neourethra [Citation8]. Also the shape of the meatus, whether slit-like or rounded, was assessed by both the parents and medical personnel.
Two patients in Group 2 (TIP) were lost to follow-up, so the final number for analysis and comparison was 32 patients, whilst all 34 patients in Group 1 (Mathieu-IP) completed follow-up.
Technique of Mathieu-IP
Under general anaesthesia, a 5-0 polyglactin 910 (Vicryl®, Ethicon, Somerville, NJ, USA) traction suture was placed on the dorsal part of the glans. The distance between the tip of the glans and the site of the hypospadias opening was measured. A suitable 6-F nelaton catheter was used as a tourniquet when needed. A ‘U’-shaped incision was created according to the distance measured beforehand. The width of the base end of the flap should be wider than the tip. Two lateral incisions were made parallel to the original urethral plate and deepened in the glanular part to form the glanular wings. A midline incision of the urethral plate was made extending from within the native meatus to the tip of the glans just beyond the pre-planned meatus site. Urethroplasty was completed by suturing the perimeatal-based skin flap with the edges of the urethral plate over a suitable urethral catheter using 6-0 polyglactin 910 suture in a running subcuticular manner until the tip of the glans. A dartos flap was harvested to cover the two suture lines. Then the glanular wings were closed symmetrically over the neourethra using transverse mattress 6-0 polyglactin 910 sutures in two layers. The penile shaft was covered by the available penile skin. A compression dressing with local gentamycin ointment was applied to the surgical area, and all patients received third-generation cephalosporin injection therapy for 1 week. The catheter was removed 7 days after surgery and all patients were followed weekly for the first month and then at 3 and 6 months.
Technique of standard TIP
The technique strictly adhered to the standard TIP and in brief, we did the following: a circumscribing skin incision was made 2 mm below the hypospadias meatus, penile degloving, the para-urethral plate incision was made, and a vertical midline incision of the urethral plate was made from within the hypospadiac meatus and extended up to the mid-glans. The urethral plate was tubularised, beginning proximally, and closed in two layers using 6/0 polyglactin 910 suture. The neomeatus was formed on a catheter 2 F larger than the urethral stent. A flap was harvested from the prepuce to cover the neourethra and finally glanuloplasty. A suitable urethral stent was left in situ for 7–10 days, with a compressive dressing applied.
Statistical analysis
Data were collected and tabulated; categorical data were expressed as number and percentage, and quantitative data were expressed as the mean (SD). The Statistical Package for the Social Sciences (SPSS® version 20) software was used for statistical analysis and comparisons between the groups were done using the chi-square test, Fisher’s exact test and Student’s t-test. P values were estimated and considered statistically significant at P < 0.05.
Results
This study included 66 patients divided randomly, using the sealed-envelope method, into two groups. Group 1 (Mathieu-IP) included 34 patients who underwent Mathieu-IP technique and Group 2 (TIP) included 32 patients who were managed using the TIP technique. There were no significant statistical differences between the two groups at baseline for age, site of the meatus, presence of chordee, and circumcision. The patient’s characteristics are presented in .
Table 1 The patients’ preoperative characteristics.
The operative and postoperative data are presented in . There was no significant difference in the mean (SD) operative time in Groups 1 and 2, at 95 (7.6) and 91.2 (8.1) min, respectively. There were no intraoperative complications in either group. For postoperative follow-up, all patients were examined weekly in the first month, then at 3 and 6 months. The new urethral meatus was vertical slit-like in 62 patients (30 in Group 1 and 32 in Group 2) and rounded in four patients in Group 1.
Table 2 Operative and postoperative data.
There were significant differences between the two groups regarding urethrocutaneous fistula and meatal stenosis in favour of Group 1 (Mathieu-IP). Fistula occurred in one patient in Group 1 and in six patients in Group 2. There was no meatal stenosis in Group 1, whilst in Group 2 there were five cases, four of which had concomitant fistula. The seven cases of urethrocutaneous fistula were repaired 6 months later by fistulectomy and a meatotomy was also performed in the four cases with concomitant stenosis. The other case of meatal stenosis without fistula was managed successfully by daily meatal dilatation for 2 months.
The stream of urine was ‘single normal’ in 32 and 26 cases in Groups 1 and 2 respectively, ‘sprayed’ in two and one case in Groups 1 and 2 respectively, and ‘narrow’ in five cases in Group 2 only.
There was no bleeding, glanular dehiscence, retention of urine, urethral diverticulosis or retraction of the new meatus during the 6-month postoperative period in either group.
Discussion
Hypospadias is a common congenital abnormality and various urethroplasty techniques have been elaborated for repair of hypospadias [Citation9]. In the present study, we compared two techniques for repairing distal hypospadias; the original TIP urethroplasty and the Mathieu technique with an incision in the urethral plate modification (Mathieu-IP), with particular reference to the rate of meatal stenosis and fistula formation.
Mathieu first described his procedure for repair of distal hypospadias using a perimeatal-based flap in 1932. Since then the technique gained in popularity, as the complication rate is <4% in most series; however, this procedure is only used for distal hypospadias, as non-hair-bearing penile skin should be used and it is rarely used for mid-shaft hypospadias [Citation10,Citation11].
In 1994, Snodgrass described TIP urethroplasty, and since then it has gained wide acceptance and become more popular with most urologists for distal and proximal hypospadias. The TIP technique is simple and gives good cosmetic results with a slit-like appearance of the final meatus. However, TIP urethroplasty has the drawbacks of the occurrence of urethrocutaneous fistula and meatal stenosis and thus the need for regular urethral dilatation, and these complications occur especially in cases with flat and narrow urethral plates [Citation5].
The cause of meatal complications in TIP is a matter of debate. Nguyen et al. [Citation12] correlated the stenosis of the meatus with the technique used by the surgeon to tubularise the urethral plate to the tip of the glans, whereas Holland and Smith [Citation5] stated that the urethral plate characteristics were the most significant factor in the complications of TIP, with a narrow and flat urethral plate more liable to urethral complications (stenosis and fistula) regardless of the deep incision and tubularisation of the plate.
Sarhan et al. [Citation13] reported that a urethral plate of ≥8 mm is crucial for the success of the TIP procedure. Also the size of the glans plays a significant role in the rate of complications after TIP rather than the type and shape of the glans (cleft or flat glans) [Citation14]. Conversely, in the Mathieu procedure the creation of the neourethra is not dependent on urethral plate characteristics or the size of the glans [Citation15].
In Mathieu technique the main disadvantage is the rounded meatus that is cosmetically less acceptable than the normal slit-like meatus [Citation16].
In the present study, we compared the results of a combined Mathieu technique plus urethral plate incision (Mathieu-IP) vs standard TIP and found significant differences between the two groups for meatal stenosis and urethrocutaneous fistula rates that occurred in 21.8% of the TIP group compared with 2.9% (one case) only in Mathieu-IP group. These results agree with Aminsharifi et al. [Citation18] who also compared the same two urethroplasty techniques and stated that the Mathieu–IP technique had reduced rates of meatal stenosis and fistula formation and gave good acceptable cosmetic results. They found a 25% complication rate in the TIP group (three meatal stenosis and two urethrocutaneous fistulae) and no complications in the Mathieu-IP group.
Our present results are less successful than those of Aminsharifi et al. [Citation18], as we had one case of urethrocutaneous fistula (2.9%) in the Mathieu-IP group, and this may have been due to the different inclusion criteria, as Aminsharifi et al. had no cases of chordee nor distal penile hypospadias and in ours, cases with minimal chordee (two cases, 5.9%) and distal penile hypospadias (six cases, 17.6%) were included.
Our present results also conform to those of Kiss et al. [Citation17] who performed the Mathieu–IP technique and reported good cosmesis and fewer complications, only one case (5.3%) of 19 cases had a urethrocutaneous fistula.
In our present study, the augmentation of the flap with a vascular dartos intermediate flap, improved the results (no cases of meatal stenosis and only one case of fistula) and this agrees with Retik et al. [Citation19] who used an intermediate vascular layer on top of a perimeatal-based flap in 204 patients and reported a 100% success rate.
The main limitation of the present study is the relatively few patients and the lack of more functional evaluations of the toilet trained children, and this is recommended for future studies, especially when the bulk of the study cohort are toilet trained children.
Conclusion
The combined Mathieu with incision of the urethral plate technique improves the cosmetic results by producing a slit-like meatus with a lower incidence of fistula formation and meatal stenosis than the TIP technique for the primary management of distal hypospadias without or with minimal chordee.
Conflicts of interest
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- C.J.DevineJrT.D.AllenP.P.KelalisN.B.HodgsonJ.W.DuckettC.E.HortonHypospadiasDial Ped Urol1197824
- M.A.RichM.A.KeatingH.M.SnyderJ.W.DuckettHinging the urethral plate in hypospadias meatoplastyJ Urol142198915511553
- A.CookA.KhouryC.NevilleD.J.BagliW.A.FarhatJ.L.Pippi SalleA multicenter evaluation of technical preferences for primary hypospadias repairJ Urol174200523542357
- A.ElbakryTubularized-incised urethral plate urethroplasty: is regular dilatation necessary for successBJU Int841999683688
- A.HollandG.SmithEffect of the depth and width of the urethral plate on tubularized incised plate urethroplastyJ Urol1642000489491
- M.SamuelS.CappsA.WorthyDistal hypospadias: which repair?BJU Int9020028891
- V.R.JayanthiG.A.McLorieA.E.KhouryB.M.ChurchillFunctional characteristics of the reconstructed neourethra after island flap urethroplastyJ Urol1531995 1657–9
- A.J.HollandG.H.SmithF.I.RossD.T.CassHOSE: an objective scoring system for evaluating the results of hypospadias surgeryBJU Int882001255258
- A.ElbakryFurther experience with the tubularized-incised urethral plate technique for hypospadias repairBJU Int892002291294
- Y.HayashiS.SasakiY.KojimaT.MaruyamaK.TozawaK.Mizunoet al.Primary and salvage urethroplasty using Mathieu meatal-based flip-flap technique for distal hypospadiasInt J Urol820011016
- E.HanssonM.BeckerM.AbergH.SvenssonAnalysis of complications after repair of hypospadiasScand J Plast Reconstr Surg Hand Surg412007120124
- M.T.NguyenW.T.SnodgrassM.R.ZaontzEffect of urethral plate characteristics on tubularized incised plate urethroplastyJ Urol171200412601262
- O.SarhanM.SaadT.HelmyA.HafezEffect of suturing technique and urethral plate characteristics on complication rate following hypospadias repair: a prospective randomized studyJ Urol1822009682686
- W.SnodgrassA.MacedoP.HoebekeP.D.MouriquandHypospadias dilemmas: around tableJ Pediatr Urol72011145157
- M.A.ImamoğluH.BakirtasComparison of two methods – Mathieu and Snodgrass – in hypospadias repairUrol Int712003251254
- E.YesildagG.TekantN.SarimuratS.N.BuyukunalDo patch procedures prevent complications of the Mathieu technique?J Urol171200426232625
- A.KissP.NyirádyL.PirótM.MerkszCombined use of perimeatal – based flap urethroplasty (Mathieu) with midline incision or urethral plate in hypospadias repairEur J Pediatr Surg132003383385
- A.AminsharifiA.TaddayunA.AssadolahpoorA.KhezriCombined use of Mathieu procedure with plate incision for hypospadias repair: a randomized clinical trialUrology722008305308
- A.B.RetikJ.MandellS.B.BauerA.AtalaMeatal based hypospadias repair with the use of dorsal subcutaneous flap to prevent urethrocutaneous fistulaJ Urol152199412291231