Abstract
Objective:
To compare the outcomes of transurethral incision (TUI) and upper pole partial nephrectomy (PN) in patients with duplex system ureterocoele (DSU).
Patients and methods:
We retrospectively reviewed the medical charts of patients who presented with DSU in the first-year of life and were managed with either TUI or PN. Patients’ demographics, ultrasonography examinations, voiding cystourethrogram studies, and dimercaptosuccinic acid scans were reviewed. Also, the postoperative vesico-ureteric reflux status and febrile urinary tract infection occurrences, and subsequent surgical interventions were identified. The outcomes for the DSU location (intravesical vs extravesical) were compared.
Results:
Between January 1995 and September 2015, 44 patients underwent TUI (31 patients) or PN (13). The TUI patients presented at a median age of 1.1 months and were followed-up for a median of 47.4 months, whilst those who underwent PN presented at a median age of 1.06 months and were followed-up for a median of 44.23 months. Postoperatively, in the TUI group, four of 15 units had improved renal function and 11 units had stable function. In the PN group, five of nine units had stable renal function and the remaining four had worsened function (P = 0.019). Furthermore, 15 of the 31 patients (48%) in the TUI group required second interventions compared with one of 13 patients in the PN group (P = 0.01). There was no significant difference between the outcomes of intravesical and extravesical DSUs after TUI and PN.
Conclusion:
This study shows significant renal function preservation with TUI compared to PN. However, secondary surgical interventions were higher with TUI.
Introduction
Ureterocoele is defined as a congenital cystic dilatation of the intravesical part of the ureter due to malformation of the submucosa of the bladder [Citation1,Citation2]. About 75% of ureterocoeles are diagnosed antenatally or during early infancy by ultrasonography (US) [Citation3]. It is mostly found in females and usually affects the upper moiety of a duplex system [Citation1,Citation3].
The principal goals for management of ureterocoele include elimination of obstruction and reflux, preservation of renal function, control of infection, protection of the normal ipsilateral and contralateral renal units, and maintenance of continence [Citation2–Citation4]. Several preoperative factors such as ureterocoele location (intravesical vs extravesical), number of moieties (single vs duplex), presence of VUR, and non-refluxing hydroureteronephrosis affect the outcome of ureterocoele management [Citation5].
Management of ureterocoele remains a controversial topic in paediatric urology practice, especially duplex system ureterocoele (DSU). Different upper urinary tract (UUT) and lower urinary tract (LUT) approaches have been proposed [Citation4,Citation6–Citation10]. The upper pole partial nephrectomy (PN) is one of the most common UUT approaches, and endoscopic [Citation7,Citation9,Citation10] and transurethral incision (TUI) are the most common LUT approaches [Citation4,Citation6,Citation8].
There is paucity of published data on the outcomes of TUI and PN as the two main approaches for management of DSU. Meanwhile, TUI is accompanied with a greater need for a second intervention due to VUR and/or non-functioning upper moiety, thus PN seems to be a better option only in non-refluxing DSU [Citation3]. The aim of the present study was to compare the outcomes of both techniques when ureterocoele was diagnosed during the first year of life. These outcomes included; the occurrence of postoperative VUR, worsening or improvement of hydronephrosis according to Society for Fetal Urology (SFU) grading, renal functional gain or loss, and the need for a second intervention. Our hypothesis was that TUI would be better than PN in terms of the renal function preservation.
Patients and methods
The medical charts of patients who received treatment for ureterocoele at our tertiary care institution were retrospectively reviewed. We included patients with DSU who presented to our institution in the first year of life and underwent either TUI or PN. We excluded patients who were managed conservatively or using a modality other than TUI and PN, patients who presented with DSU after the first year of life, and patients who missed postoperative follow-up.
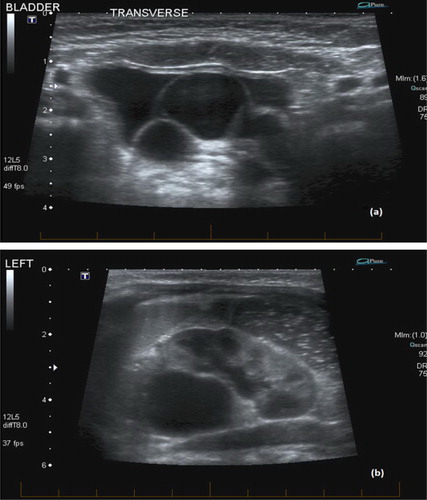
The patients’ demographics and preoperative investigations including US with hydronephrosis grading using the SFU grading () were reviewed, in addition to voiding cystourethrogram (VCUG) studies and DMSA scans. All preoperative and postoperative investigations were reviewed by one investigator (A.H.) who was blinded to the surgical intervention.
Fig. 1 (a) US image shows large lobulated left ureterocoele. (b) Associated left upper moiety Grade 4 hydronephrosis and lower moiety Grade 2 hydronephrosis.
Surgical interventions were selected according to the surgeons’ preference. Initial surgical interventions were indicated in cases of large obstructed ureterocoeles. TUI was the preferred primary approach for most surgeons. A cold knife was used for TUI. TUI was performed intravesically at the most dependent part of the ureterocoele and extended distally beyond the bladder neck in the case of the extravesical type. However, one surgeon preferred PN mainly for patients with non-functioning upper pole with no or low-grade ipsilateral VUR. Subsequent surgical interventions were indicated for worsening hydronephrosis, worsening VUR, or recurrent febrile UTI.
Moreover, the findings of postoperative US (at the last follow-up or before secondary surgical intervention), and postoperative DMSA scans were documented. Also, the postoperative status of VUR and occurrence of febrile UTI, and the need for a second surgical intervention were identified. Postoperative VUR (after TUI or PN) was indicated if the patient had any of the following; febrile UTI, new hydronephrosis in the other moiety or contralateral kidney or worsening hydronephrosis.
Assessment of the outcomes of TUI and PN as definitive alternatives for the management of DSU was our primary outcome. Improvement of hydronephrosis (by US) and renal function (by DMSA) were considered indicators of success. Improvement of hydronephrosis was defined as downgrading of the dilated pelvicalyceal system after TUI or downgrading or disappearance of hydronephrosis of the ipsilateral lower pole after PN. The change in ipsilateral renal function, using DMSA, after TUI and PN was calculated. Improvement was considered with an increase in the total ipsilateral renal function, whilst worsening was considered with a >10% decline in total ipsilateral renal function. A net change in renal function ranging from –10% to 10% was considered stable.
Data were recorded and analysed using the IBM Statistical Package for the Social Sciences (SPSS®, version 20; SPSS Inc., IBM Corp., Armonk, NY, USA). The chi-squared test was used to estimate the associations between categorical variables and the Mann–Whitney U-test was used to estimate the associations between continuous variables. A P < 0.05 was considered to indicate statistical significance.
Results
Between January 1995 and September 2015, 79 patients were identified who presented to our department with ureterocoele. Nine patients who were managed conservatively and two who missed follow-up were excluded. Another 13 patients were excluded because the method of ureterocoele management was neither TUI nor PN. These patient underwent LUT reconstruction ± PN (nine) and total nephrectomy (four). Moreover, 11 patients who presented with ureterocoele after the age of 1-year were excluded. Therefore, 44 patients with DSUs were included in this study. All DSUs were unilateral and 64% (28 patients) were extravesical.
Demographic data and patients’ characteristics are shown in . All patients had preoperative US. However, data of VCUG were not available for two patients in the TUI group.
Table 1 Patients’ demographics and characteristics.
In all, 31 patients (70.5%) underwent TUI and 13 (29.5%) underwent PN. Patients who underwent TUI presented at a median (range) age of 1.1 (0–11.8) months and were followed-up for a median (range) of 47.4 (9.03–199.8) months, whilst patients who underwent PN presented at a median (range) age of 1.06 (0.1–11.9) months and were followed-up for a median (range) of 44.23 (8.3–139.7) months. The overall median (range) follow-up was 46.7 (8.3–199.8) months. Postoperative outcomes are described in .
Table 2 Postoperative outcomes after primary intervention.
During initial evaluation, lower pole ipsilateral VUR was diagnosed in 18/31 renal units in the TUI group compared with three of 13 renal units in the PN group (P = 0.019). High-grade VUR was identified in 61% (11/18) of the refluxing renal units in the TUI group. Whilst all refluxing renal units in the PN group were low-grade (P = 0.049). Furthermore, contralateral VUR was diagnosed in three of 31 of renal units in the TUI group compared with two of 13 of renal units in the PN group.
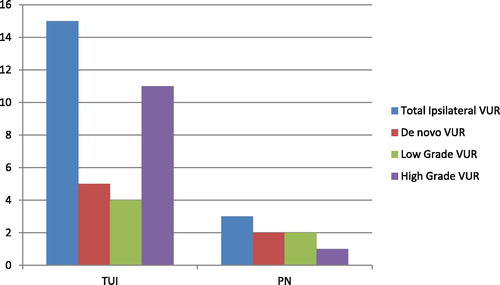
Postoperatively, VCUG was performed in 24/31 patients in the TUI group and seven of 13 patients in the PN group (). Notably, four of the five de novo VURs were diagnosed in the upper moieties of the TUI group. Contralateral VUR was diagnosed in five of 24 patients in the TUI group compared with three of seven patients in the PN group. All diagnosed contralateral VURs in both groups were low-grade.
Postoperative DMSA was performed in 12/31 patients in the TUI group and nine of 13 patients in the PN group. In the TUI group, four of 15 renal units had improved renal function and 11 renal units had stable function. In the PN group, five of nine renal units had stable renal function and the other renal units had worsened function. The mean (range) change of ipsilateral renal function in the TUI group was 1.2 (–9 to 19)% compared with –8.7 (–26 to 8)% (P = 0.19) in the PN group.
Hydronephrosis improved in 22/31 (71%) of the renal units in the TUI group compared with 12/13 of the renal units in PN group. Furthermore, there was worsening of hydronephrosis in five of the 31 patients (16%) in the TUI group compared with one of the 13 patients in the PN group.
Febrile UTI was diagnosed in 13/31 (42%) patients in the TUI group compared with two of the 13 patients in the PN group. Three patients in TUI group had more than two febrile UTIs, whilst only one patient in the PN group had more than two febrile UTI episodes. Secondary intervention was required in one of the three patients in the TUI group and in the patient in the PN group.
In the TUI group, 15 patients (48%) had second interventions. The median (range) age at second surgical intervention was 31.1 (16.6–79.3) months. Four patients had second interventions due to worsening VUR, two due to frequent febrile UTI, four with combined worsening VUR (upper moiety) and frequent febrile UTI, and five due to worsening hydronephrosis (). Two of those who underwent PN only as a second intervention had worsening VUR and febrile UTI. Hence, a third surgical intervention in the form of re-implantation, was indicated
Table 3 Types of secondary surgical intervention according the primary approach.
In the PN group, only one patient required a second surgical intervention due to frequent febrile UTI associated with Grade 3 VUR. This second surgical intervention was carried out at 37.5 months after the PN. Six patients in the TUI group had PN as a second surgical intervention; three due to worsening VUR, two due to worsening hydronephrosis, and one due to febrile UTI.
Extravesical DSU was diagnosed in 28 patients. There was no significant difference between the intravesical and extravesical cases regarding the outcomes of TUI in terms of postoperative VUR (P = 0.74), febrile UTI (P = 0.22), de novo VUR (P = 0.89), and second intervention (P = 0.098); and the outcomes of PN in terms of postoperative VUR (P = 0.27), febrile UTI (P = 0.71), de novo VUR (P = 0.053), and second intervention (P = 0.41) ().
Table 4 Comparison between intravesical and extravesical DSUs for the outcomes following TUI and PN.
Discussion
Primary TUI has been widely used as minimally invasive approach for decompression of ureterocoele [Citation4,Citation6,Citation8]. In a meta-analysis by Byun and Merguerian [Citation11], duplex system, preoperative high-grade VUR, and extravesical ureterocoele were associated with increased need for a second intervention. Our present results confirmed our hypothesis that TUIs were associated with better function and there was no need for second interventions for more than half of patients who presented in the first year of life.
Over a median follow-up period of 47.4 months after TUI and 44.2 months after PN, we found that there was a need for a second intervention in almost half of patients (48.4%) in the TUI group compared with one of the 13 patients in the PN group (P = 0.01). A similar study by Castagnetti et al. [Citation12] reported the outcomes of 32 patients with DSU treated with TUI and nine treated with PN, during the first year of life. A second intervention was required in 20% of patients after TUI vs none of the nine patients after PN [Citation12]. In a study by Jesus et al. [Citation13], a second intervention was required in 25/60 (42%) patients with DSU treated with TUI. This percentage was even higher (73.7%) in a study by Sander et al. [Citation14]. Adorisio et al. [Citation2] evaluated the effectiveness of TUI as a primary intervention in 46 patients with extravesical DSU. Over a mean follow-up of 3.8 years, ureterocoele decompression was achieved in 43 patients (93%), only three patients required a second intervention for correction of persistent ureterocoele (two ureteropyelostomy and one uretero-ureterostomy), 14 patients developed VUR in the lower moiety of the ipsilateral kidney (10 had spontaneous resolution and four underwent endoscopic correction) and five patients developed VUR in the upper moiety of the ipsilateral kidney (two had spontaneous resolution after 6 months of follow-up and three were treated with endoscopic injection). Yet, no deterioration of renal function was seen in any of the patients [Citation2]. Nevertheless, the incidence of VUR after TUI is high and endoscopic injection therapy has been an appropriate minimally invasive approach that greatly reduces the need for re-implantation surgery [Citation15,Citation16].
In a recent study by Boucher et al. [Citation17], the outcomes of TUI and PN for the management of extravesical ureterocoele were comparable in terms of the need for second procedures. However, depending on the degree of preoperative VUR, PN is still associated with a substantial rate of second intervention, ranging between 10% and 62% [Citation7,Citation18]. This need for a second intervention depends largely on the presence of preoperative VUR. In a study by Merlini and Lelli Chiesa [Citation1], the rate of second intervention after PN ranged between 15% and 20% whenever VUR was absent preoperatively, and between 50% and 100% whenever VUR was present preoperatively. Nonetheless, a recent study found that both TUI and PN are successful techniques for primary management of DSU regardless of preoperative parameters [Citation12].
Decompression of ureterocoele during PN occurs by leaving the stump of the upper ureter open after upper pole hemi-nephrectomy and partial upper ureterectomy [Citation2,Citation7,Citation9,Citation10]. However, ureterocoele decompression after PN has been achieved in ∼50% of cases, with the need of a second intervention in 19–62% of cases [Citation7,Citation18]. From the literature it appears that PN is better than TUI for managing DSU without preoperative VUR, with a success rate of up to 80% [Citation7,Citation19]. However, an ipsilateral and contralateral VUR has been reported in 40–50% during long-term follow-up [Citation7]. A major concern about PN is the need for flank incision and the risk of injuring the lower pole vasculature. However, it can now be performed laparoscopically [Citation5].
For renal function, the present study found that the improvement in renal function was significantly better after TUI compared with PN (25% vs 0%; P = 0.019). In a study by Vates et al. [Citation20], PN resulted in renal functional improvement in two of eight patients and worsened in two. These variations may be due to the small numbers included in our and their studies. Although worsened function after PN seems logical, one cannot explain the improvement of ipsilateral function in the Vates et al. [Citation20] study.
In the present study, there was no significant difference between TUI and PN for the occurrence of febrile UTI (41.9% vs 15.4%; P = 0.09), postoperative VUR (62.5% vs 42.9%; P = 0.79), de novo VUR (20.8% vs 28.6%; P = 0.67), and hydronephrosis improvement (71% vs 92.3%; P = 0.123). In a study by Jesus et al. [Citation13], postoperative VUR occurred in 40% of patients after TUI of DSU. Although the incidence of new-onset VUR is high after TUI, it appears that most of the cases resolve spontaneously during the follow-up period [Citation13,Citation21].
In the present study, there was no significant difference in the outcome of TUI in intravesical vs extravesical DSU for postoperative VUR (P = 0.74), febrile UTI (P = 0.22), de novo VUR (P = 0.89), and second intervention (P = 0.098) (). This was congruent with the results of the Castagnetti et al. [Citation22] study. There were comparable outcomes between 24 extravesical DSU and 17 intravesical DSU for de novo VUR, non-functioning upper moiety, and the need for a second intervention [Citation22].
We think that technical factors may interfere in the outcomes of TUI in DSU. It has been reported that the choice of TUI approach is important for achieving efficient decompression without causing VUR [Citation23,Citation24]. Whatever the approach, it is recommended that the TUI should be performed above the level of the bladder wall in the intravesical portion of the ureterocoele to create a valve-like flap, thus avoiding VUR [Citation15,Citation19,Citation22].
Our present results add to the evaluation of two popular treatments for patients with DSU who present within the first year of life. We found that early TUI could preserve more renal function than PN. However, the risks of second surgical interventions and febrile UTI were higher in comparison with PN. In our opinion, PN is a reasonable treatment without LUT reconstruction, for patients with non-functioning upper moiety when associated with no or low-grade VUR.
Limitations of the present study include: i) the retrospective nature, ii) the small number of patients, and iii) the short follow-up period. However, the number of patients in the present study is comparable with other studies on DSU [Citation12,Citation13,Citation15,Citation19,Citation22], probably due to the low incidence of DSU. Moreover, the choice of primary treatment, TUI vs PN, was largely according to surgeon preference. PN may have been chosen for patients with suspected low or no function at the upper pole. However, this might not be entirely true as about half of the patients who underwent PN had lost some function after surgery. The results of the present study should be also interpreted with caution as the lower rate of secondary surgery in PN could also be attributed to the higher rate of VUR in the TUI group.
Conclusion
For patients with DSU presenting in the first year of life, significant renal function preservation was seen with TUI compared to PN. However, secondary surgical interventions and the rate of febrile UTI were higher with TUI.
Conflict of interest
None.
Funding source
None.
Contributors’ statements
Amr Hodhod: Data collection and drafting the initial manuscript.
Yasser A. Noureldin: Drafting the initial manuscript and editing the final manuscript.
Mohamed El-Sherbiny: Editing the final manuscript.
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Ethical statement
This study was conducted in accordance with the Declaration of Helsinki and its amendments, and after obtaining the institutional ethics approval.
Acknowledgements
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- E.MerliniChiesa P.LelliObstructive ureterocele-an ongoing challengeWorld J Urol222004107114
- O.AdorisioA.EliaL.LandiM.TavernaV.MalvasioA.D.DantiEffectiveness of primary endoscopic incision in treatment of extravesical ureterocele associated with duplex systemUrology772011191194
- R.M.DecterJ.K.SprungerR.J.HollandCan a single individualized procedure predictably resolve all the problematic aspects of the pediatric ureterocele?J.Urol165200123082310
- D.E.CoplenJ.S.BartholdControversies in the management of extravesical ureterocelesUrology562000665668
- M.CastagnettiA.El-GhoneimiManagement of duplex system ureteroceles in neonates and infantsNat.Rev.Urol62009307315
- A.A.ShokeirR.J.NijmanUreterocele: an ongoing challenge in infancy and childhoodBJU Int902002777783
- D.A.HusmannD.H.EwaltW.J.GlenskiP.A.BernierUreterocele associated with ureteral duplication and a nonfunctioning upper pole segment: management by partial nephroureterectomy aloneJ.Urol1541995723726
- D.A.HusmannW.R.StrandD.H.EwaltS.A.KramerIs endoscopic decompression of the neonatal extravesical upper pole ureterocele necessary for prevention of urinary tract infections or bladder neck obstruction?J.Urol167200214401442
- T.PetitP.RavasseP.DelmasDoes the endoscopic incision of ureteroceles reduce the indications for partial nephrectomy?BJU Int831999675678
- J.S.VallaJ.BreaudL.CarfagnaS.TursiniH.SteyaertTreatment of ureterocele on duplex ureter: upper pole nephrectomy by retroperitoneoscopy in children based on a series of 24 casesEur.Urol432003426429
- E.ByunP.A.MerguerianA meta-analysis of surgical practice patterns in the endoscopic management of ureterocelesJ.Urol176200618711877
- M.CastagnettiE.VidalM.BureiP.ZucchettaL.MurerW.RigamontiDuplex system ureterocele in infants: should we reconsider the indications for secondary surgery after endoscopic puncture or partial nephrectomy?J.Pediatr.Urol920131116
- L.E.JesusW.A.FarhatA.C.AmaranteR.B.DiniB.LeslieD.J.Bägliet al.Clinical evolution of vesicoureteral reflux following endoscopic puncture in children with duplex system ureterocelesJ.Urol186201114551458
- J.C.SanderA.N.BilgutayI.StanaselC.J.KohN.JanzenE.T.Gonzaleset al.Outcomes of endoscopic incision for the treatment of ureterocele in children at a single institutionJ.Urol1932015662666
- A.KajbafzadehA.H.SalmasiS.PayabvashH.ArshadiH.R.AkbariS.MoosaviEvolution of endoscopic management of extravesical ureterocele: a new approachJ.Urol177200711181123
- B.ChertinD.de CaluweP.PuriIs primary endoscopic puncture of ureterocele a long-term effective procedure?J.Pediatr.Surg382003116119
- A.BoucherJ.CloutierA.RousseauR.CharroisS.BolducIs an initial endoscopic treatment for all ureteroceles appropriate?J.Pediatr.Urol92013339343
- A.A.CaldamoneH.M.Snyder3rdJ.W.DuckettUreteroceles in children: followup of management with upper tract approachJ.Urol131198411301132
- D.HusmannB.StrandD.EwaltM.ClementS.KramerT.AllenManagement of ectopic ureterocele associated with renal duplication: a comparison of partial nephrectomy and endoscopic decompressionJ.Urol162199914061409
- T.S.VatesT.BukowskiJ.TriestA.FreedmanC.SmithA.Perlmutteret al.Is there a best alternative to treating the obstructed upper pole?J.Urol1561996744746
- R.GanderM.AsensioG.F.RoyoJ.LloretEvaluation of the initial treatment of ureterocelesUrology892016113117
- M.CastagnettiM.CimadorM.SergioE.de GraziaTransurethral incision of duplex system ureteroceles in neonates: does it increase the need for secondary surgery in intravesical and extravesical cases?BJU Int93200413131317
- D.Ben MeirC.J.SilvaP.RaoD.ChiangP.A.DewanDoes the endoscopic technique of ureterocele incision matter?J.Urol1722004684686
- J.T.JankowskiJ.S.PalmerHolmium: yttrium-aluminum-garnet laser puncture of ureteroceles in neonatal periodUrology682006179181