Abstract
Objectives:
To evaluate the presence of balanitis xerotica obliterans (BXO), clinically and pathologically, in the urethra of boys with failed previous hypospadias repair and where surgical management was planned.
Patients and methods:
Between February 2010 and March 2015, boys with failed distal penile hypospadias repair who were planned for surgical management were evaluated for the presence of clinical and pathological evidence of BXO. Samples were obtained from the urethral plate and fossa navicularis, after obtaining informed consent and ethical approval. The samples were fixed, sectioned, and haematoxylin and eosin stained for light microscopic examination.
Results:
In all, 157 boys were enrolled in our study, with a mean (SD) age of 6.4 (2.8) years. All the boys had a history of failed hypospadias repair surgeries (once or more). The presentation was fistula in 34 boys (21.7%), meatal stenosis in 45 (28.7%), urethral stricture in 28 (17.8%), and total dehiscence in 50 (31.8%). BXO was detected clinically in 46 boys (29.3%). The total number of biopsies taken was 314, of which 124 (39.5%) were pathologically BXO-positive samples. Of the 157 boys, BXO-positive cases were clinically associated with fistula in seven boys (4.5%), meatal stenosis in 18 (10.8%), urethral stricture in seven (4.5%), and total dehiscence in 15 (9.6%). Of the 314 pathological samples, pathologically BXO-positive samples were associated with fistula in 20 samples (6.4%), meatal stenosis in 40 (12.7%), urethral stricture in 22 (7%), and total dehiscence in 42 (13.4%).
Conclusions:
In failed hypospadias cases BXO should be considered, especially for cases with multiple failures, meatal stenosis, and total dehiscence. Urethral plate and fossa navicularis biopsies are important in planning a proper approach for subsequent repair.
Introduction
Balanitis xerotica obliterans (BXO) or lichen sclerosus et atrophicus affects the genital skin and can extend into the urethra. The disease is of unknown aetiology and Stuhmer was the first to report its effect on the male genitalia in 1928 [Citation1,Citation2].
The disease has variable degrees of clinical features, ranging from a mild to an extensive form and a definitive diagnosis is made by histopathological examination. The presence of BXO in the prepuce and external urethral meatus in boys after circumcision has been confirmed by different studies [Citation2,Citation3].
Complications after hypospadias repair include meatal stenosis, fistula, neourethral stricture, and total dehiscence. The true incidence of BXO is not known; however, some reports suggest a higher incidence in patients with failed hypospadias repair [Citation4].
The present study evaluated the association of BXO with cases of failed attempts of surgical repair of distal penile hypospadias.
Patients and methods
Case selection
This was a prospective observational study, carried out between February 2010 and March 2015, in which all boys with previously failed attempts of distal penile hypospadias repair in our hospital and those referred from other hospitals for surgical management, were evaluated for the presence of clinical and pathological evidence of BXO.
Exclusion criteria included boys with proximal hypospadias, de novo hypospadias, and adult cases. Samples were obtained from the urethral plate and fossa navicularis. Informed consent was signed by the parents of the boys. Ethical approval was obtained from our Institutional Board Committee. The samples were fixed, sectioned and haematoxylin and eosin (H&E) stained for light microscopic examination for the presence of BXO.
Histopathology
H&E staining was performed on 4-µm thick formalin-fixed, paraffin-embedded tissue sections, obtained from boys with failed hypospadias repair, using the staining protocol of Yesudian et al. [Citation5].
Morphological evaluation was performed on the stained slides; the epidermis, dermal-epithelial junction, and dermis were evaluated in all cases.
Statistical analysis
Data were tabulated and statistically analysed using Stata® software (Stata Corp. 2011. Stata Statistical software: Release 12. College Station TX: Stata Corp LP). We used Fisher’s exact test and the Mann–Whitney’s test, as appropriate. A P ≤ 0.05 was considered to indicate statistical significance.
Results
In all, 157 boys were enrolled in the study, with a mean (SD) age of 6.4 (2.8) years. All the boys had had previously failed surgeries for glandular (11 boys), coronal (35), sub-coronal (93) and distal penile hypospadias (18). We could identify the type of primary repair in 126 boys [meatal advancement and glanduloplasty incorporated (11 boys), tubularised incised-plate repair (85), onlay flap (13), and staged hypospadias using penile flaps (17)] and in 31 the primary repair could not be identified. Of the 157 boys, 29 had had a first complication repair, 86 had had a second complication repair, and 42 had had repairs more than twice.
In all, 34 boys (21.7%) presented with fistula, 45 (28.7%) presented with meatal stenosis, 28 (17.8%) presented with urethral stricture, and 50 (31.8%) presented with total dehiscence. There were clinically positive cases of BXO in 47 boys (30%). A total number of 314 biopsies were taken and there were pathologically BXO-positive samples in 124 (39.5%).
Clinically BXO-positive cases were associated with fistula in seven boys (4.5%), meatal stenosis in 18 (10.8%), urethral stricture in seven (4.5%), and total dehiscence in 15 (9.6%). The differences between the association of clinically evident cases and the patient’s presentation were not statistically significant (P = 0.270; ).
Table 1 Patient presentation in association to clinical and pathological evidence of BXO.
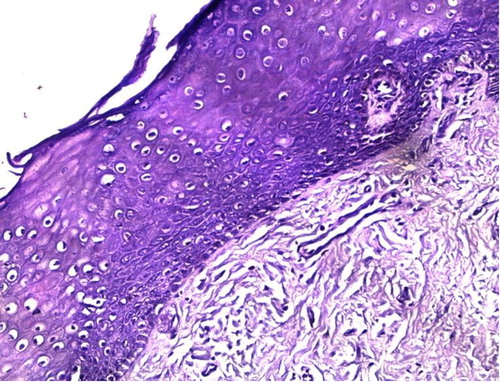
Histopathologically, BXO-positive lesions showed pronounced orthokeratotic hyperkeratosis accompanied by atrophy of the epidermis and loss of rete ridges, a distinctive combination of features. Basal cell vacuolation and clefting of the dermal-epithelial junction may also occur. The upper dermis is usually markedly oedematous and collagen forms a homogenised band, beneath which there may be a lymphoplasmacytic infiltrate ( and ).
Fig. 1 H&E image showing epidermal atrophy and orthokeratotic hyperkeratosis, showing basal cell vacuolisation, clefting of dermal-epithelial junction; dermis shows dense collagenisation and lymphocytic infiltrate (×200).
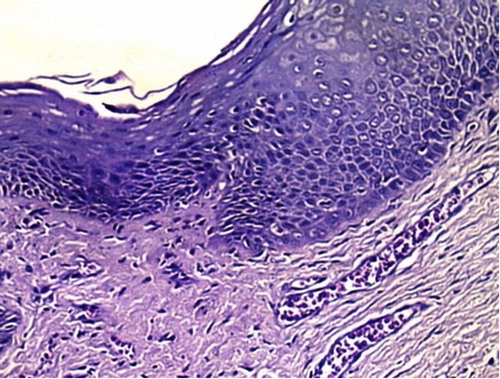
Fig. 2 H&E image showing atrophic epidermis with loss of rete ridges, dermal hyalinisation, thickened basement membrane and marked dermal collagenisation (×200).
Pathologically BXO-positive samples were associated with fistula in 20 (6.4%), meatal stenosis in 40 (12.7%), urethral stricture in 22 (7%), and total dehiscence in 42 (13.4%) of all samples ().
Samples taken from the fossa navicularis that had pathology positive criteria for BXO were more prevalent with a presentation of meatal stenosis, total dehiscence and urethral stricture, whilst BXO positivity was less associated with fistula and this was statistically significant (P = 0.038; ).
Table 2 Patient presentation in relation to pathologically BXO-negative or BXO-positive fossa navicularis samples.
Samples obtained from the urethral plate that had pathological criteria for BXO were more prevalent in boys with meatal stenosis, total dehiscence, and fistula, whilst BXO positivity was less associated with urethral stricture; however, that was not statistically significant (P = 0.934; ).
Table 3 Patient presentation in relation to pathologically BXO-negative or BXO-positive urethral plate samples.
Discussion
BXO is an idiopathic and chronic dermatitis that affects the glans and prepuce, sometimes extending into the urethra. The exact aetiology of this disease is unknown [Citation6]. Clinical features of BXO may be seen clinically; however, a conclusive diagnosis is only possible through histopathological examination [Citation7]. BXO was first described as an adult disease, until a series of cases of BXO with acquired phimosis and meatal stenosis was reported in boys [Citation8,Citation9]. An incidence of BXO of up to 19% has been reported amongst boys undergoing circumcision for preputial pathology [Citation3]. Incidence of urethral stricture and meatal stenosis due to BXO after hypospadias repair has been reported in different series, with an incidence of up to 4% [Citation3,Citation10,Citation11].
Postoperative complications after hypospadias repair include urethra–cutaneous fistula formation, meatal stenosis, and dehiscence. Urethral stricture and meatal stenosis due to BXO are not well recognised amongst paediatric surgeons and there are few detailed published reports about this complication after hypospadias repair [Citation4].
Venn and Mundy [Citation12] reported an incidence of histopathological evidence of urethral stricture due to BXO in 28/114 patients (24.5%) with anterior urethral strictures. Barbagli et al. [Citation13] reported an incidence of 31/106 patients (29%), who underwent anterior urethroplasty for anterior urethral strictures. Barbagli et al. [Citation13] also reported a high incidence of BXO in patients with failed hypospadias repair. On the other hand, some authors believe that BXO affects only the skin, with no effect on the urethra. Hence, the relationship between BXO and post-urethroplasty anterior urethral stricture is still disputed. Although BXO can be diagnosed clinically, definitive diagnosis depends on histopathological examination. Characteristic features include atrophic epidermis with hyperkeratosis with zone of vacuolar degeneration of the basal layer. Collagen forms a homogenous band at the dermal-epithelial junction with elastin fibres to form an amorphous substance in the advanced stages [Citation14].
Barbagli et al. [Citation15] studied a series of 99 patients diagnosed with BXO by biopsy, who had multiple biopsies taken from the foreskin, penile skin, glans, urethral meatus, mucosa of the navicularis, and penile and bulbar urethra, to confirm the presence of BXO. They reported an incidence of 85.4% positive cases for BXO. Meatal BXO was documented histologically in up to 91.5% of cases, fossa navicularis in 84.4%, and penile urethra in 70.6%.
In the present study, there was histological evidence for a BXO prevalence of 39.5% amongst boys with failed distal hypospadias repair. More cases were diagnosed histopathologically than clinically, in agreement with the findings of other studies [Citation2,Citation9].
Samples taken from the fossa navicularis had pathology positive criteria for BXO with greater presentation in association with meatal stenosis, total dehiscence, and urethral stricture, whilst BXO was less associated with fistula. This was not evident for the urethral plate biopsies. These results emphasise the concept of greater impact of BXO in the development of meatal stenosis and fossa navicularis stricture, following anterior urethroplasty surgery. The presence of BXO, as an aetiological factor of failed hypospadias repair or urethroplasty, dictates the use of buccal mucosal graft and avoidance of skin substitutes to provide satisfactory outcomes and reduce the recurrence of complications caused by BXO [Citation16]. This highlights the significance of taking biopsies to exclude the presence of BXO in complicated hypospadias surgery to select the appropriate method of repair. It is well established in the literature that urethroplasty using buccal mucosal graft is superior to local penile skin flaps in the presence of BXO [Citation17–Citation20]. We believe that over-looked or undiagnosed BXO in complicated hypospadias patients would increase the risk of treatment failure.
Limitations of the present study include the lack of data relating to previous surgeries, as most of the cases were referred to our hospital from other centres.
Conclusions
In failed hypospadias repair cases, BXO should be considered, especially for cases with multiple failures, meatal stenosis, and total dehiscence. Urethral plate and fossa navicularis biopsies are important in planning a proper approach to subsequent repair.
Source of funding
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- W.S.KizerT.PrarieA.F.MoreyBalanitis xerotica obliterans: epidemiologic distribution in an equal access health care systemSouth Med J962003911
- G.BarbagliE.PalminteriS.BalòS.VallascianiE.MeariniE.Costantiniet al.Lichen sclerosus of the male genitalia and urethral stricture diseasesUrol Int73200415
- P.M.BaleA.LochheadH.C.MartinI.GollowBalanitis xerotica obliterans in childrenPediatr Pathol71987617627
- S.UemuraJ.M.HutsonA.A.WoodwardJ.H.KellyC.W.ChowBalanitis xerotica obliterans with urethral stricture after hypospadias repairPediatr Surg Int162000144145
- P.D.YesudianH.SugunendranC.M.BatesC.O'MahonyLichen sclerosusInt J STD AIDS162005465473
- P.C.GargolloH.P.KozakewichS.B.BauerJ.G.BorerC.A.PetersA.B.Retiket al.Balanitis xerotica obliterans in boysJ Urol174200514091412
- S.JayakumarB.AntaoO.BevingtonP.FurnessG.K.NinanBalanitis xerotica obliterans in children and its incidence under the age of 5 yearsJ Pediatr Urol82012272275
- R.D.CatterallJ.K.OatesTreatment of balanitis xerotica obliterans with hydrocortisone injectionsBr J Vener Dis3819627577
- I.DepasqualeA.J.ParkA.BrackaThe treatment of balanitis xerotica obliteransBJU Int862000459465
- W.H.HendrenR.E.CaesarChordee without hypospadias: experience with 33 casesJ Urol1471992107109
- J.M.GaratG.ChéchileF.AlgabaJ.M.SantaulariaBalanitis xerotica obliterans in childrenJ Urol1361986436437
- S.N.VennA.R.MundyUrethroplasty for balanitis xerotica obliteransBr J Urol811998735737
- G.BarbagliM.LazzeriE.PalminteriD.TuriniLichen sclerosis of male genitalia involving anterior urethraLancet3541999429
- Y.MiharaM.MiharaY.HagariS.ShimaoLichen sclerosus et atrophicus. A histological, immunohistochemical and electron microscopic studyArch Dermatol Res2861994434442
- G.BarbagliF.MirriM.GallucciS.SansaloneG.RomanoM.LazzeriHistological evidence of urethral involvement in male patients with genital lichen sclerosus: a preliminary reportJ Urol185201121712176
- D.DubeyA.SehgalA.SrivastavaA.MandhaniR.KapoorA.KumarBuccal mucosal urethroplasty for balanitis xerotica obliterans related urethral strictures: the outcome of 1 and 2-stage techniquesJ Urol1732005463466
- C.K.PatelJ.C.BuckleyL.N.ZinmanA.J.VanniOutcomes for management of lichen sclerosus urethral strictures by 3 different techniquesUrology912016215221
- R.L.MoriK.W.AngermeierStaged urethroplasty in the management of complex anterior urethral stricture diseaseTransl Androl Urol420152934
- M.J.BelsanteJ.P.SelphA.C.PetersonThe contemporary management of urethral strictures in men resulting from lichen sclerosusTransl Androl Urol420152228
- Y.M.XuC.FengY.L.SaQ.FuJ.ZhangH.XieOutcome of 1-stage urethroplasty using oral mucosal grafts for the treatment of urethral strictures associated with genital lichen sclerosusUrology832014232236
