Abstract
Objective:
To determine if significant differences exist in the perioperative outcomes of patients aged >75 years treated with radical cystectomy (RC) compared to younger patients, as RC is frequently not offered to ‘elderly’ patients with bladder cancer because of supposed increased risks of complications.
Patients and methods:
We retrospectively analysed prospectively collected data of all patients that underwent RC in our centre from May 2013 to June 2015. In all, 81 consecutive RCs were identified and included in our study. Patients were divided into two age groups: Group A, aged <75 years (51 patients) and Group B, aged ≥75 years (30). Co-morbidities and perioperative outcomes were compared between the groups. Fisher’s exact test was used for statistical analysis.
Results:
In 68 patients RC was performed laparoscopically and the remaining 13 patients underwent open RC. The mean (range) age was 70.7 (36–85) years. There were 37 patients with muscle-invasive disease and 42 had non-muscle-invasive disease. The median hospital stay was not significantly different between the two age groups (10 vs 11 days). There was no significant difference in the preoperative Charlson co-morbidity index. The 30-day mortality rate was 4% for those aged <75 years and 6.6% for those aged ≥75 years, with overall perioperative complication rates of 57% vs 66%, respectively. Most complications were minor (Clavien–Dindo Grade I–II) and there was no statistically significant difference between the two cohorts. There was also no statistically significant difference in blood transfusion rates.
Conclusion:
RC in patients aged ≥75 years has similar perioperative morbidity when compared with younger patients and can be offered in selected elderly patients. Thus, age should not be an absolute contraindication for RC.
Introduction
Bladder cancer remains the second most common urological malignancy in the Western world, with the highest incidence in the elderly population [Citation1–Citation4]. In the UK, it is estimated that people aged ≥75 years account for more than half of the cases of bladder cancer diagnosed each year [Citation5]. Advances in medicine have led to increased life expectancy, thus compounding the impact of bladder cancer in the elderly population.
Radical cystectomy (RC) is considered the ‘gold standard’ treatment for muscle-invasive bladder cancer (MIBC). It is also indicated in those with high-risk and recurrent non-muscle invasive bladder cancer (NMIBC) [Citation1]. However, RC is associated with significant morbidity and a perioperative 90-day mortality rate of up to 8% [Citation6]. Therefore, this treatment option is not routinely offered to older patients. Some authors have reported a higher incidence of both minor and major complications in the elderly with complication rates as high as 64% [Citation7] and prolonged postoperative hospital stay [Citation8]. There is still considerable debate in the literature as to whether patients aged >70 years are suitable for such radical surgery [Citation2,Citation8,Citation9].
Advances in minimally invasive surgical techniques have facilitated a drive to offering radical surgery to elderly patients who previously would have been treated conservatively or offered radical radiotherapy [Citation2,Citation9–Citation11]. This minimally invasive approach has many advantages including reduced intraoperative blood loss and postoperative analgesic requirements, whilst facilitating earlier mobility leading to a shorter perioperative admission and possibly lower complication rates [Citation9–Citation12].
There are several publications comparing RC outcome in patients aged >70 years with younger patients. Articles focussing on patients aged >75 years have either reported unfavourable outcomes after such treatment [Citation8,Citation13] or focussed on comparing open vs minimally invasive techniques within the age cohort rather than comparing outcomes with younger patients [Citation12,Citation14].
The aim of the present study was to investigate whether there are any significant differences in preoperative co-morbidities, perioperative complications, length of stay (LOS), and mortality rate between patients aged ≥75 years and younger patients treated for bladder cancer by RC.
Patients and methods
All patients that underwent open or minimally invasive (hand-assisted laparoscopic) RC in Pinderfields General Hospital between May 2013 and June 2015 were included in the study. In all, 81 consecutive patients were identified. The indication for RC was MIBC in 37 patients, high-grade and/or recurrent NMIBC in 42, one lympho-epithelial lesion, and one T3 basal cell prostate cancer.
Preoperatively, CT of the chest, abdomen and pelvis was performed to assess for evidence of metastatic disease. Additionally, all patients underwent cardio-pulmonary exercise testing (CPEX) to determine their anaerobic threshold, and therefore fitness for surgery, as well as determining postoperative level of care (Level 1, 2 or 3 beds). Patients unable to perform CPEX were deemed unsuitable for surgery based on previous internal audit reviews.
All patients were enrolled on an enhanced recovery programme postoperatively. This comprises of clear fluids immediately postoperatively, free fluids and sitting out of bed on day 1, urethral drain out and mobilising on day 2, a soft diet if the patient passed flatus on day 3. Suppositories were given on day 7 if patients had opened their bowels and were passing flatus. Ureteric stents were removed on day 10. Patients were reviewed in the outpatient clinic 6 weeks after RC for clinical examination and routine blood tests. This was followed by regular outpatient visits with surveillance imaging.
Most patients had hand-assisted laparoscopic RC (68 patients) and 13 underwent open RC. All procedures were performed by two experienced surgeons (M.D. and P.W.).
Data collected included patients’ demographics, stage of disease, operative time, intraoperative blood loss and transfusion rates, LOS, Charlson co-morbidity index, perioperative complications, and 90-day postoperative mortality rate.
The Clavien–Dindo classification system was used to describe postoperative complications [Citation15]. Grade I and II complications were classified as minor and Grade III–V were classified as major. All data were prospectively entered into a database.
Patients were divided into two cohorts based on age; Group A, patients aged <75 years (51 patients) and Group B, patients aged ≥75 years (30 patients). Fisher’s exact test was used to compare the two groups. A P < 0.05 was considered to indicate statistical significance.
Results
There were 81 patients included in this study, with 51 patients aged <75 years (Group A) and 30 patients aged ≥75 years (Group B). The mean (range) age for patients in Group A was 65.9 (36–74) years and for patients in Group B was 78.7 (75–83) years. In all, 11 patients (37%) in Group B group were aged ≥80 years. In Group A, 12 patients were female and 39 were male. In Group B, five patients were female and 25 were male.
Ileal conduit diversion (79 patients) was the most common form of urinary diversion in both groups. The remaining two patients received a continent urinary diversion, in the form of a Studer ileal-neobladder (both patients in Group A).
The type of procedure performed, duration of procedure, intraoperative blood loss, and the indications for surgery are given in . Most procedures were performed for MIBC. The remaining cases were undertaken for NMIBC intravesical treatment failure, high-grade (Grade 3) NMIBC, salvage after radiotherapy, or for other cancers. In all, 17 patients were offered neoadjuvant chemotherapy (12 in Group A and five in Group B).
Table 1 Surgical procedure performed, duration of procedure, intraoperative blood loss and indications for RC.
The variation in the final histology TNM stage between the younger and older cohorts is given in . Group B had a higher percentage of both MIBC and non-organ confined disease, as well as a higher percentage of positive lymph nodes. However, using Fisher’s exact test for statistical analysis showed that these were not significant findings (). Of the 64 males included, 20 had concurrent adenocarcinoma of the prostate on final histology, 31% and 32% for groups A and group B, respectively.
Table 2 Final histology TNM stage for patients undergoing RC differentiated by age.
outlines both the Charlson score and the CPEX testing results for both cohorts of patients. A higher proportion of younger patients had a Charlson score of zero, whilst (apart from one younger patient with a Charlson score of 4) the older patients had a higher proportion of scores of 1–3. However, after statistical analysis this was shown to not be significant (). A greater percentage of Group B patients had an anaerobic threshold of ≥11 mL/kg/min, but this was not statistically significant (P = 0.61).
Table 3 Preoperative Charlson score and CPEX anaerobic threshold results for both cohorts of patients.
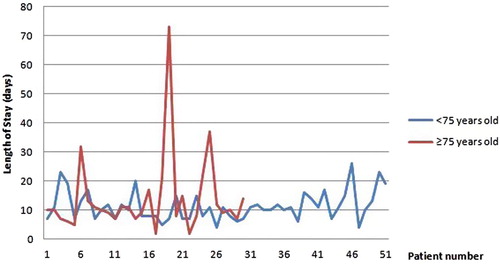
The LOS after RC is shown in . The median (range) LOS for Group A was 11 (4–26) days and 10 (2–73) days for Group B. There were six patients in Group B who stayed for >15 days and nine in Group A. Of these 15 patients, six (40%) had undergone open surgery.
The perioperative complications, classified using the Clavien–Dindo classification system, are given in . It can be seen from the results in that there was no statistically significant difference for both perioperative complications and blood transfusion rates between the two cohorts of patients, with overall complications rates being 57% and 66% for groups A and B, respectively.
Table 4 Perioperative complications rates classified by Clavien–Dindo classification and blood transfusion rates for both cohorts of patients.
Four patients returned to theatre due to complications, all from Group B (three bowel anastomotic leaks and one wound dehiscence). Each cohort had two deaths within 30 days of surgery, given a mortality rate of 4% and 6.6% for groups A and B, respectively.
Discussion
The expansion of the elderly population is putting ever increasing pressure on urological surgery, not least the surgical treatment of bladder cancer [Citation2–Citation4]. With the average life expectancy in the UK now 81.4 years for males and 84.6 years for females, and with 8% of the total populations now aged >75 years [Citation16], attitudes must change when considering patients for radical surgery.
RC has long been recommended as the ‘gold standard’ treatment for patients with MIBC, as well as being indicated for high-risk and recurrent NMIBC [Citation1,Citation17]. Published series report favourable survival outcomes after RC for MIBC when compared to bladder preservation treatments such as radical radiotherapy, transurethral resection of bladder tumours, and local chemotherapy [Citation17–Citation19]. Patients being managed conservatively could potentially lead to multiple hospital admissions with complications of bladder cancer such as haematuria, leading to significant anaemia, and bladder dysfunction.
Advances in laparoscopic surgical techniques have facilitated a drive to treat patients aged >75 years with bladder cancer with curative intent [Citation2,Citation9,Citation12,Citation14]. Reported advantages of laparoscopic RC include reduced postoperative hospital stay, reduced intraoperative blood loss (thus reducing blood transfusion rates), faster return to normal diet and bowel function, and better visualisation of the pelvic anatomy [Citation11,Citation20,Citation21], all of which would benefit an elderly population. However, open RC is still the recommended procedure for elderly patients, with patients with limited physiological reserves not being able to tolerate a prolonged Trendelenburg position and pneumoperitoneum being the most often cited reasons against laparoscopic RC [Citation12,Citation21,Citation22].
We have shown that within our present cohort of patients, there was no significant difference in the preoperative co-morbidity status between those aged <75 years and ≥75 years based on the Charlson scoring system. Interestingly, the older cohort of patients had a higher percentage of patients with a CPEX >11 mL/kg/min (77% vs 71%), but this was not statistically significant.
Another cited reason for not offering radical surgery to elderly patients is the supposedly increased risk of perioperative complications. RC is a major procedure that is associated with a high complication rate, ranging from 34% to 65% [Citation2,Citation4,Citation9,Citation10,Citation23]. Our present data are comparable with published results, with an overall complication rate of 60%, of which 86% were classified as Clavien–Dindo Grade I–II (i.e. minor). There was no significant difference between our two cohorts of patients for perioperative complication rates (). The major complication rates (Clavien–Dindo Grade ≥III) in our present series also compare favourably with other series (6% for patients aged <75 years, 13% for patients aged ≥75 years, overall 8.6%). Albisinni et al. [Citation23] and Izquierdo et al. [Citation4] reported an 18% and 27% major perioperative complication rate, respectively.
It has been reported that blood transfusion after RC can impact on survival postoperatively and cancer recurrence [Citation24,Citation25]. Both of our cohorts had lower transfusion rates compared to the published literature [Citation24–Citation26], at 15% and 10% in groups A and B, respectively. All but one of these transfusions was minor (1–2 units of blood).
The LOS after RC was comparable to the article reporting this [Citation9], with the elderly cohort LOS an average of 1 day less that the younger patients (10 vs 11 days).
A handful of recent publications have reported no significant difference in 30- and 90-day mortality rates between patients aged >70 years and younger cohorts [Citation2,Citation4,Citation9,Citation14]. Current published mortality rates after RC range from 0.8% to 8.3% [Citation3,Citation7,Citation27]. Our present results for both 30- and 90-day mortality conform to this; 4% for those aged <75 years and 6.6% for those aged ≥75 years.
Outcomes from major surgery, such as RC, can be continuously monitored in an unbiased fashion to facilitate timely changes to practice if outcomes are unfavourable. Cumulative summation charts have been proposed to offer a robust monitoring process in RC by being able to generate an ‘early warning’ score if measurable outcomes, such as complication rates and mortality, breech a defined bench mark [Citation28].
Conclusion
We have shown that for RC there is no significant difference between patients aged ≥75 years and younger patients for preoperative co-morbidity, perioperative complications, blood transfusion rates, and postoperative mortality. Age should not be an absolute contraindication to RC in elderly patients. Focus should be on preoperative performance status and co-morbidities when planning life-prolonging surgery.
Conflicts of interest
None declared.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- J.A.WitjesE.CompératN.C.CowanM.De SantisG.GakisN.Jameset al.Guidelines on muscle-invasive and metastatic bladder cancerEur Assoc Urol2015 Available at: https://uroweb.org/wp-content/uploads/EAU-Guidelines-Muscle-invasive-and-Metastatic-Bladder-Cancer-2015-v1.pdf. Accessed September 2017
- P.P.FontanaS.A.GregorioJ.G.RivasL.C.SánchezJ.C.LedoÁ.T.Gómezet al.Perioperative and survival outcomes of laparoscopic radical cystectomy for bladder cancer in patients over 70 yearsCent European J Urol6820152429
- V.NovotnyO.W.HakenbergD.WiessnerU.HeberlingR.J.LitzS.Oehlschlaegeret al.Perioperative complications of radical cystectomy in a contemporary seriesEur Urol522007397402
- L.IzquierdoL.PeriP.LeonM.Ramírez-BackhausT.ManningA.Alcarazet al.The role of cystectomy in elderly patients – a multicentre analysisBJU Int116Suppl. 320157379
- Office for National Statistics. Cancer Registration Statistics, England Statistical bulletins. Available at: http://www.ons.gov.uk/ons/rel/vsob1/cancer-statistics-registrations--england--series-mb1-/index.html. Accessed September 2017.
- M.E.NielsenK.MallinM.A.WeaverB.PalisA.StewartD.P.Winchesteret al.Association of hospital volume with conditional 90-day mortality after cystectomy: an analysis of the National Cancer Data BaseBJU Int11420144655
- F.LiedbergEarly complications and morbidity of radical cystectomyEur Urol Suppl920102530
- N.ZebicS.WeinknechtD.KroepflRadical cystectomy in patients aged ≥75 years: an updated review of patients treated with curative and palliative intentBJU Int95200512111214
- J.GuillotreauR.MiocinovicX.GaméS.ForestB.MalavaudJ.Kaouket al.Outcomes of laparoscopic and robotic radical cystectomy in the elderly patientsUrology792012585590
- R.M.CowardA.SmithM.RaynorM.NielsenE.M.WallenR.S.PruthiFeasibility and outcomes of robotic-assisted laparoscopic radical cystectomy for bladder cancer in older patientsUrology77201111111114
- A.FerganyLaparoscopic radical cystectomyArab J Urol1020124045
- S.ZengZ.ZhangX.YuR.SongR.WeiJ.Zhaoet al.Laparoscopic versus open radical cystectomy for elderly patients over 75-year-old: a single center comparative analysisPLoS One92014e98950
- C.S.LauJ.TalugS.B.WilliamsD.Y.JosephsonN.H.RuelK.G.Chanet al.Robotic-assisted laparoscopic radical cystectomy in the octogenarianInt J Med Robot82012247252
- T.YasuiK.TozawaR.AndoT.HamakawaS.IwatsukiK.Taguchiet al.Laparoscopic versus open radical cystectomy for patients older than 75 years: a single-center comparative analysisAsian Pac J Cancer Prev16201563536358
- D.DindoN.DemartinesP.A.ClavienClassification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a surveyAnn Surg2402004205213
- Office of National statistics. Ageing of the UK population. Available at: http://www.ons.gov.uk/ons/rel/pop-estimate/population-estimates-for-uk--england-and-wales--scotland-and-northern-ireland/mid-2014/sty-ageing-of-the-uk-population.html. Accessed 9/12/2015.
- J.L.GoreM.S.LitwinJ.LaiE.M.YanoR.MadisonC.Setodjiet al.Use of radical cystectomy for patients with invasive bladder cancerJ Natl Cancer Inst21022010802811
- F.A.YafiW.KassoufRadical cystectomy is the treatment of choice for invasive bladder cancerCan Urol Assoc J32009409412
- W.SupitC.A.MochtarR.B.SantosoR.UmbasOutcomes of radical cystectomy and bladder preservation treatment for muscle-invasive urothelial carcinoma of the bladderAsian J Surg372014184189
- J.R.CansinoJ.CisnerosS.AlonsoL.Martinez-PiñeiroA.AguileraA.Taberneroet al.Laparoscopic radical cystectomy: initial series and analysis of resultsEur Urol Suppl52006956961
- A.K.HemalS.B.KollaComparison of laparoscopic and open radical cystoprostatectomy or localized bladder cancer with 3-year oncological follow up: a single surgeon experienceJ Urol178200723402343
- K.A.RichardsA.K.KaderR.OttoJ.A.PettusJ.J.SmithIIIA.K.HemalIs robot assisted radical cystectomy justified in the elderly? A comparison of robotic versus open radical cystectomy for bladder cancer in elderly ≥75 years oldJ Endourol26201213011306
- S.AlbisinniJ.RassweilerC.C.AbbouX.CathelineauP.ChlostaL.Fossionet al.Long-term analysis of oncological outcomes after laparoscopic radical cystectomy in Europe: results from a multicentre study by the European Association of Urology (EAU) section of Uro-technologyBJU Int1152015937945
- B.J.LinderI.FrankJ.C.ChevilleM.K.TollefsonR.H.ThompsonR.F.Tarrellet al.The impact of perioperative blood transfusion on cancer recurrence and survival following radical cystectomyEur Urol632013839845
- T.M.MorganD.A.BarocasS.S.ChangS.E.PhillipsS.SalemP.E.Clarket al.The relationship between perioperative blood transfusion and overall mortality in patients undergoing radical cystectomy for bladder cancerUrol Oncol312013871877
- E.J.AbelB.J.LinderT.M.BaumanR.M.BauerR.H.ThompsonP.Thapaet al.Perioperative blood transfusion and radical cystectomy: does timing of transfusion affect bladder cancer mortalityEur Urol66201411391147
- R.ChahalS.K.SundaramR.IddendenD.F.FormanP.M.WestonS.C.HarrisonA study of the morbidity, mortality and long-term survival following radical cystectomy and radical radiotherapy in the treatment of invasive bladder cancer in YorkshireEur Urol432003246257
- K.M.SiddiquiJ.I.IzawaSystematic methods for measuring outcomes: How they may be used to improve outcomes after radical cystectomyArab J Urol132015122127