Abstract
Objective:
To assess the effectiveness and advantages of ultra-mini-percutaneous nephrolithotomy (UM-PCNL) versus standard PCNL (S-PCNL), as one of the most important differences between the various PCNL techniques is the size of the renal access, which contributes to the broad spectrum of complications and outcomes.
Patients and methods:
This clinical randomised trial was conducted in 2016. In all, 70 patients with renal or upper ureteric stones of 10–20 mm in diameter, who were candidates for PCNL, were divided equally into two groups. Group A, underwent UM-PCNL using a 9.8-F ureteroscope through a 16-F sheath; and Group B, underwent S-PCNL using a 24-F nephroscope through a 30-F sheath. The stones were fragmented by pneumatic lithotripsy. Any perioperative complications and need for analgesia were recorded, and postoperative pain was assessed in both groups using a visual analogue scale (VAS).
Results:
There were statistically significant differences in postoperative haemoglobin values, haemoglobin drop, transfusion rate, duration of hospitalisation and postoperative VAS pain score between the groups (P < 0.05). There were no significant differences in operation time, need for auxiliary procedures or stone-free rate.
Conclusion:
A minimally invasive UM-PCNL using a 9.8-F ureteroscope can play an important role in the treatment of symptomatic renal and upper ureteric stones of <20 mm in diameter with lesser blood loss, duration of hospitalisation, need of transfusion, and postoperative pain compared with S-PCNL.
Introduction
Since the introduction of percutaneous nephrolithotomy (PCNL) there have been various modifications to improve success rates. The overall complication rate of PCNL can be up to 83%, which can be minimised by accurate patient selection and careful postoperative follow-up [Citation1]. One of the most important differences between the various PCNL techniques is the size of renal access (and the required specialised equipment), which contributes to the broad spectrum of complications and outcomes. Today, PCNL techniques include: standard PCNL (S-PCNL), mini-PCNL (also called mini-perc), ultra-mini-PCNL (UM-PCNL) [Citation2], and the recently introduced micro-PCNL. S-PCNL is the standard procedure in the treatment of renal and upper ureteric stones using a 28–30-F ureteroscope. The mini-PCNL (mini-perc) was first introduced by Helal et al. [Citation3] in 1997 using a 10-F paediatric cystoscope in children, which reduced the complications of the standard method. This technique was shown to have a stone-free rate (SFR) of 85% with minimal morbidity in young children [Citation4]. Furthermore, it was shown that it could be used for all kinds of upper tract stones [Citation5]. In UM-PCNL, the adult size ureteroscope is replaced with a nephroscope with a smaller metal sheath. The last procedure is micro-PCNL using unique equipment as well. In micro-PCNL, the 4.85-F needle reaches the collecting system under direct vision, and renal access and PCNL are performed in a single step [Citation6].
In the present randomised clinical trial, we evaluated the effectiveness and advantages of UM-PCNL vs S-PCNL. We describe our modified UM-PCNL technique that allows the use of transureter lithotripsy equipment through a tract that is smaller than for S-PCNL and even smaller than previously reported for mini-PCNL.
Patients and methods
In this a randomised clinical trial, 70 patients (45 males and 25 females) were recruited from the Urology Department of Emam Ali Hospital of Bojnurd who were undergoing elective lithotripsy between January 2016 and April 2017. Inclusion criterion was patients with 10–20 mm symptomatic renal and upper ureteric stones that were inappropriate for extracorporeal shockwave lithotripsy (ESWL), ureteroscopy or due to the lack of a holmium laser. The patients were equally divided into two groups. Exclusion criteria included: pregnancy, abnormal coagulopathy state, recent use of NSAIDs, UTI, and stones of >20 mm.
The sample size was calculated using PASS software, with a power of 80%, α of 0.05, and level of confidence of 95%. Based on these calculations, an n = 35 was determined for each group.
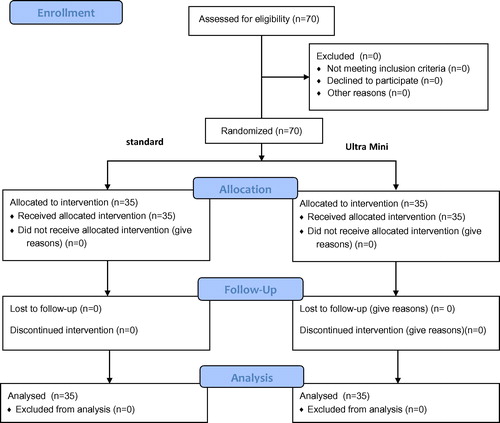
In all, 70 patients who met the inclusion criteria were randomly assigned based on the list of random number generator into two groups. Group A, comprised 35 patients who underwent UM-PCNL; and Group B, comprised 35 patients who underwent S-PCNL ().
After obtaining informed consent from the patients, the research objectives were explained to the patients.
Before surgery, we performed several assessments including: complete physical examination, full medical history, complete blood count, urine analysis, urine culture, blood clotting tests, kidney–urinary–bladder X-ray (KUB), renal ultrasonography (US), and IVU or non-contrast CT. UM-PCNL was performed under general anaesthesia in Group A. After induction of anaesthesia, with the patient in lithotomy, a 5-F urethral catheter was inserted into the ureter via cystoscopy. Then the patient was repositioned to prone. Then, an 18-G access needle was placed into the preferred calyx under fluoroscopic guidance. A tiny incision was made in the skin and fascia, and then the 16-F fascial dilator was used to dilate the nephrostomy tract to pass the 16-F semi-rigid plastic sheath. Then, a 9.8-F, 33-cm semi-rigid ureteroscope (Richard Wolf Medical Instruments, Vernon Hills, IL, USA) was introduced to the sheath. The ureteric stones were broken into pieces using pneumatic lithotripsy. Fragmented stones too large for spontaneous passage from the ureter were removed using a grasper. Finally, the ureteroscope and sheath were removed and the tract site was packed for 2–3 min. The ureteric catheter remained in situ for 48 h (before discharge). In Group B, the patients underwent S-PCNL. Again, under general anaesthesia in lithotomy, a 5-F ureteric catheter was placed via cystoscopy. Having changed the position to prone, an 18-G access needle was inserted into the preferred calyx under fluoroscopic guidance. A 30-F dilator dilated the tract under fluoroscopic guidance using a ‘one-shot’ dilatation method. A 30-F Amplatz sheath was inserted. The S-PCNL was performed with a rigid 24-F nephroscope (Richard Wolf Medical Instruments) and pneumatic LithoClast (Boston Scientific, Marlborough, MA, USA). Finally, the Amplatz and nephroscope were removed and the tract site was packed for 2–3 min. The ureteric catheter was left in situ for 2 days.
Any perioperative complications and need for analgesia were recorded. Pethidine was used for pain control in both groups. We administered a mean (range) of 50 (25–75) mg pethidine in Group A and 100 (75–150) mg in Group B to reduce postoperative pain in our patients.
KUB and US were performed in all patients to evaluate the success rate 48 h after the procedure before discharge. Furthermore, we assessed postoperative pain in both groups using a visual analogue scale (VAS), which ranged from zero (no pain) to 10 (maximum pain). Written informed consent was signed by all patients, and the consent study protocol was approved by the Institutional Ethics Committee.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS®, version 13; SPSS Inc., Chicago, IL, USA) was used for all analyses. We used the independent samples t-test and the Mann–Whitney U-test for comparison of quantitative variables and the chi-squared test for qualitative variables. To remove the effect of factors affecting the duration of hospitalisation and postoperative flank pain, a linear regression model was used. In addition, quantitative variables are given as the mean ± standard deviation (SD) and a P < 0.05 was considered statistically significant.
Ethical considerations
The study was licensed by the Ethics Committee of North Khorasan University of Medical Sciences based on guidelines of the Declaration of Helsinki (Hong Kong revision, 1983) and good clinical practice. All patients participating in the study read and signed the consent letter.
A recommendation for reporting the randomisation clinical trial was conducted based on the definition of the Consolidated Standards of Reporting Trials (CONSORT) statement.
Results
In all, 70 patients were equally divided into two groups of 35 patients. The UM-PCNL group (Group A), contained 23 males (65.7%) and 12 females (34.3%), with a mean (SD) age of 41.58 (13.35) years; and the S-PCNL group (Group B), included 22 males (63%) and 13 females (37%), with a mean (SD) age of 43.55 (10.94) years.
The patients’ characteristics are summarised in . Considering each variable in both groups, we found statistically significant differences in postoperative haemoglobin values, haemoglobin drop, transfusion rate, duration of hospitalisation, and postoperative pain score (VAS) between the two groups (P < .05).
Table 1 Patients’ characteristics.
Neither group had supracostal or multiple accesses. There were no significant differences in operation time, need for auxiliary procedures, and SFR. There were few complications in both groups and these included: fever (two in the Group A and three in Group B), intraoperative bleeding (one in both groups), and one case of perirenal urinary collection in Group A compared to three cases in Group B, which were managed by prolonged ureteric catheterisation. There was no significant difference between the groups for the success rate. Moreover, two cases of urinary leakage from the nephrostomy tract were reported in Group A, one treated with JJ insertion and the other with prolonged ureteric catheterisation, and one in Group B that was also managed by prolonged ureteric catheterisation.
Discussion
The management of kidney and upper ureteric stones using a safer, effective and less harmful procedure is an ambition of every treatment surgery.
In the present study, we evaluated the efficacy of UM-PCNL and S-PCNL procedures in the treatment of symptomatic renal and upper ureteric stones of <20 mm after failed ESWL or anatomical considerations that required PCNL. We used ureteroscopes as surrogates for different size nephroscopes. The SFR for our present UM-PCNL cohort was 93.5%, which is concordant with the other studies that have reported SFRs of 77.8–97.2% [Citation7–Citation11].
Giusti et al. [Citation7] reported that the haematocrit drop and duration of hospitalisation were lesser for mini-PCNL compared to S-PCNL, which is similar to our present findings. However, they reported a longer operation time in for their mini-PCNL group, which is exactly the opposite of our present results. Moreover, the SFR was 94% for their S-PCNL group and 77.8% in their mini-PCNL group for the treatment of stones of <20 mm in diameter. It is clear that renal access has a negative effect on renal tissue and thus larger tracts can lead to more haemorrhage and subsequent haemoglobin drop, which can be an important issue in children and physically frail patients.
In 2013, Zeng et al. [Citation12] reported that the mini-PNL procedure had a shorter operation time and lesser haemoglobin drop for simple and complex renal stones; findings are consistent with our present study. These outcomes may be attributed to the influence of the smaller size of renal access in mini-PCNL, which led to its introduction as a safe and effective procedure in the treatment of renal and ureteric stones [Citation5,Citation11–Citation14].
Jackman et al. [Citation15] reported 83 mL blood loss, 6.6% haematocrit reduction, and 1.7 days hospitalisation in their patients undergoing mini-PCNL, with a SFR of 89%. They concluded that mini-PCNL may bring practical advantages in comparison to S-PCNL for haemorrhage, duration of hospitalisation, and postoperative pain, which confirms our present results.
In 2013, Desai [Citation2,Citation16] revealed UM-PCNL as an effective and safe technique for renal and ureteric stones. They reported a 1.4 mg/mL haemoglobin decrease, hospital stay of 1.2 days and a SFR of 86.66% for renal stones and 97.2% for upper ureteric stones, without any significant postoperative complications. By contrast, Li et al. [Citation17] reported no significant advantages of mini-PCNL over S-PCNL for the surgical trauma during their procedures.
In another study, Yang et al. [Citation10] reported an operation time of 45 min, SFR of 97.2%, and no need of blood transfusion for mini-PCNL in their patients with upper ureteric stones. To our knowledge, no other study has compared S-PCNL and UM-PCNL as in our present study. One of the disadvantages of UM-PCNL was the poor visibility due to intraoperative haemorrhage in the surgical field. Indeed, the presence of bleeding in the surgical field is one of the most frequent causes of intraoperative blurred vision. Thus, correct use of the access tract and efficient irrigation is beneficial in reducing bleeding and its negative subsequent impact on the operation. To summarise, there were various advantages of UM-PCNL over S-PCNL in the treatment of renal and ureteric calculi. In our present study, we found UM-PCNL to be a less invasive and effective technique using a 9.8-F ureteroscope through a small access tract for the treatment of renal and ureteric calculi, which reduced the common consequences of the conventional S-PCNL procedure. The haemoglobin drop, reported pain, need of transfusion, and duration of hospitalisation were all lesser in the UM-PCNL group. However, it had its own drawbacks, which included decreased visualisation, poor irrigation, and difficult stone extraction. One of the most important benefits of this method was the lesser postoperative pain, which may make it superior to S-PCNL.
Some limitations of our present study warrant consideration. The low number of patients studied and their recruitment from a single institution are two major limitations. Therefore, it carries all the inherent potential issues associated with such studies. According to our experience, we recommend UM-PCNL in patients with renal and upper ureteric stones of <20 mm refractory to ESWL. However, we do not recommend this procedure for larger stones.
Conclusion
The UM-PCNL, a minimally invasive PCNL method using a 9.8-F ureteroscope, can play an important role in the treatment of symptomatic renal and upper ureteric stones of <20 mm with lesser blood loss, duration of hospitalisation, need of transfusion, and postoperative pain compared with S-PCNL. This is a new technique that awaits further technical developments before it can be offered as a standard technique in all patients.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- M.S.MichelL.TrojanJ.J.RassweilerComplications in percutaneous nephrolithotomyEur Urol512007899906
- J.DesaiG.ZengZ.ZhaoW.ZhongW.ChenW.WuA novel technique of ultra-mini-percutaneous nephrolithotomy: introduction and an initial experience for treatment of upper urinary calculi less than 2 cmBiomed Res Int20132013490793
- M.HelalT.BlackJ.LockhartT.E.FigueroaThe Hickman peel-away sheath: alternative for pediatric percutaneous nephrolithotomyJ Endourol111997171172
- S.V.JackmanS.P.HedicanC.A.PetersS.G.DocimoPercutaneous nephrolithotomy in infants and preschool age children: experience with a new techniqueUrology521998697701
- X.LiZ.HeK.WuS.K.LiG.ZengJ.Yuanet al.Chinese minimally invasive percutaneous nephrolithotomy: the Guangzhou experienceJ Endourol23200916931697
- M.R.DesaiR.SharmaS.MishraR.B.SabnisC.StiefM.BaderSingle-step percutaneous nephrolithotomy (microperc): the initial clinical reportJ Urol1862011140145
- G.GiustiA.PiccinelliG.TavernaA.BenettiL.PasiniM.Corintiet al.Miniperc? no, thank you!Eur Urol512007810815
- Z.HuangF.FuZ.ZhongL.ZhangR.XuX.ZhaoChinese minimally invasive percutaneous nephrolithotomy for intrarenal stones in patients with solitary kidney: a single-center experiencePLoS One72012e40577
- M.MongaS.OglevieMinipercutaneous nephorlithotomyJ Endourol142000419421
- S.F.YangM.LeiX.LiMinimally invasive percutaneous nephrolithotomy for impacted upper ureteric calculi (a report of 71 cases)Chin J Mod Operative Surg42003297298
- W.ZhongG.ZengW.WuW.ChenK.WuMinimally invasive percutaneous nephrolithotomy with multiple mini tracts in a single session in treating staghorn calculiUrol Res392011117122
- G.ZengZ.ZhaoS.WanZ.MaiW.WuW.Zhonget al.Minimally invasive percutaneous nephrolithotomy for simple and complex renal caliceal stones: a comparative analysis of more than 10,000 casesJ Endourol27201312031208
- S.LahmeV.ZimmermannsA.HochmuthA.Janitzki[Minimally invasive PCNL (mini-perc). alternative treatment modality or replacement of conventional PCNL?]Urologe A472008563568
- Q.LongJ.GuoZ.XuY.YangH.WangY.Zhuet al.Experience of mini-percutaneous nephrolithotomy in the treatment of large impacted proximal ureteral stonesUrol Int902013384388
- S.V.JackmanS.G.DocimoJ.A.CadedduJ.T.BishoffL.R.KavoussiT.W.JarrettThe “mini-perc” technique: a less invasive alternative to percutaneous nephrolithotomyWorld J Urol161998371374
- J.DesaiR.SolankiUltra-mini percutaneous nephrolithotomy (UMP): one more arma mentariumBJU Int112201310461049
- L.Y.LiX.GaoM.YangJ.F.LiH.B.ZhangW.F.Xuet al.Does a smaller tract in percutaneous nephrolithotomy contribute to less invasiveness? a prospective comparative studyUrology7520105661