Abstract
Objective:
To compare the effect of interrupted- and continuous-suture urethroplasty on complication rates in Snodgrass tubularised incised-plate (TIP) hypospadias repair.
Patients and methods:
This was a prospective randomised study comprising 100 boys (age range 1–5 years) with primary subcoronal, distal- and mid-penile hypospadias who underwent repair from October 2010 to March 2015 in a tertiary care hospital. Boys with glanular, recurrent, and proximal hypospadias were excluded from the study. The boys were prospectively randomised into two groups: Group A, comprised 50 boys who underwent interrupted subcuticular suture Snodgrass TIP urethroplasty; and Group B, comprised 50 boys who underwent continuous subcuticular suture Snodgrass TIP urethroplasty. Outcomes were assessed in terms of complication rates and aesthetic appearance during follow-up.
Results:
There was no significant difference in the occurrence of complications between the groups. There were 21 complications, with 10 occurring in Group A and 11 in Group-B. Urethrocutaneous fistula was the most common complication in both groups (six in Group A and seven in Group B), the fistulae were <2 mm in nine patients and 3–5 mm in the remaining four. Partial glans dehiscence occurred in one patient in each group. One patient from each group also had superficial wound infection, meatal stenosis and urethral stricture respectively, all of which were managed conservatively. The resultant urinary stream was single and good in all patients of both groups.
Conclusions:
The type of suture technique had no significant effect on complication rates after Snodgrass hypospadias repair and thus the choice of technique depends on surgeon preference.
Introduction
Snodgrass tubularised incised-plate (TIP) urethroplasty is the currently most commonly used hypospadias repair, especially for distal hypospadias. It has resulted in significant improvement in the outcome of hypospadias repair. Despite this, the incidence of postoperative complications after hypospadias repair is 1–24% [Citation1]. Therefore, besides the surgical technique used for hypospadias repair, other factors affecting the outcome of hypospadias repair may exist. Some of these factors including patient age, type of hypospadias, presence and degree of chordee, quality and width of urethral plate, type of suture, type of suturing technique, use of magnification during repair, type of dressing used after repair, use of catheter during repair, provision of soft tissue coverage over urethra, and use of antibiotics after repair have been reported in literature [Citation1–Citation19]. However, the exact roles of these factors in the successful outcome of hypospadias repair are yet to be determined.
Table 3 Incidence of complications in both groups.
We performed a prospective randomised study to evaluate and compare the effect of interrupted- vs continuous-suture urethroplasty on complication rates in Snodgrass TIP hypospadias repair.
Patients and methods
Setting, design and participants
This prospective randomised study was conducted on boys with primary anterior hypospadias whose parents had agreed to participate in the study, and who were admitted and operated upon in a tertiary medical centre from October 2010 to March 2015. The mean (range) age of the boys with primary anterior hypospadias was 26.2 (12–66) months. Informed signed consent was obtained from the parents of the boys before the start of the study. Ethical clearance for conducting the study was also obtained from Institutional Ethics Committee.
Inclusion criteria: Only primary cases with subcoronal, distal- or mid-penile hypospadias with minimal chordee and suitable for Snodgrass TIP urethroplasty were included in the study.
Exclusion criteria: Cases with glanular, recurrent, or proximal hypospadias, or moderate-to-severe chordee were excluded from the study.
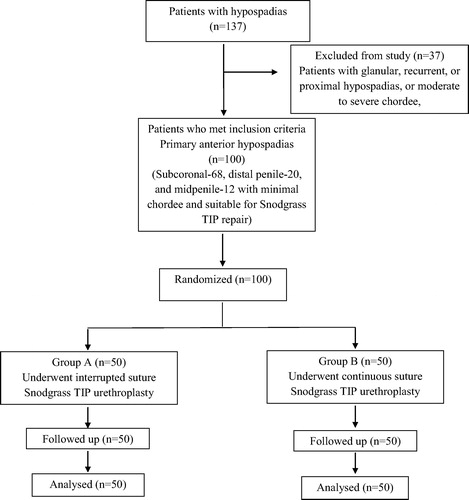
All patients were assessed with history and clinical examination, and routine blood investigation. The Consolidated Standards of Reporting Trials (CONSORT) 2010 guidelines were followed ().
Table 1 Checklist items according to the Consolidated Standards of Reporting Trials (CONSORT) 2010 guidelines.
Randomisation
All patients who met the inclusion criteria were prospectively randomised into two parallel groups based on type of suture technique used for urethroplasty in Snodgrass hypospadias repair (). Randomisation was done using sequential numbering of patients and then randomisation with simple random sampling with the help of a computer random table to distribute patients in a ratio of 1:1 between the two groups.
Study procedure (intervention)
Group A, comprised 50 boys who underwent interrupted-suture Snodgrass TIP urethroplasty; and Group B, comprised 50 boys who underwent continuous-suture Snodgrass TIP urethroplasty. Prophylactic preoperative i.v. antibiotic (amoxicillin-clavulanic acid) was administered routinely in all patients at the start of surgery. The surgery was performed under general anaesthesia with caudal analgesia to decrease the postoperative pain in all patients. In all patients, Snodgrass TIP urethroplasty was done with subcuticular 6–0 polyglactin 910 (Vicryl) suture in two layers over an 8–10 F catheter. Neourethral coverage with preputial dartos flap was also used in all cases. All patients were operated on by author-1 and author-2 using similar operative and perioperative principles of hypospadias repair. The catheter remained in situ for 10–12 days for bladder drainage.
After removal of the catheter, urinary stream was observed in all patients of both groups. All patients had postoperative antibiotic prophylaxis with amoxicillin + clavulanic acid in appropriate doses for 7 days. The dressing was removed in all patients on the fifth postoperative day.
Follow-up and outcome assessment
Patients were examined at the time of catheter removal, then monthly for the first initial 6 months, followed by every 6 months, with mean (range) follow-up of 23.5 (9–36) months.
Outcomes were assessed by author-3 and author-4, who were not aware of the suturing technique used in the Snodgrass TIP repair. Thus, outcome assessment was made blind. Outcomes were assessed in both groups based on the following criteria; (i) operative time, (ii) occurrence of complications including both early and late postoperative complications, (iii) urinary stream during voiding, and, (iv) aesthetic appearance score using a scale of 0–10. A score of zero was assigned to complete failure of repair, whilst a score of 10 represented an appearance similar to that of a normal circumcised penis with the meatus at the tip of glans.
Statistical analysis
The outcomes were also verified statistically using the Statistical Package for Social Science (SPSS®, version 17.0; SPSS Inc., Chicago, IL, USA). Fisher’s exact test was used to compare categorical variables and ANOVA was used to compare continuous variables, with a P < 0.05 considered statistically significant.
Results
Of 137 patients with hypospadias, 100 patients meeting the inclusion criteria, i.e., with primary anterior hypospadias (subcoronal in 68, distal penile in 20, and mid-penile in 12) were selected for the study () and were randomly divided into two groups each comprised of 50 patients ().
Table 2 Incidence of different types of hypospadias in both groups.
Operative time
The mean operative time taken for the repair in Group A (139 min) was more than that in Group B (132.4 min), but this difference was statistically insignificant (ANOVA, P > 0.10). Initially, the time taken for the repair in Group A was more compared to Group B, whilst latterly the operative time for the interrupted-suture urethroplasty was almost the same as for the continuous-suture urethroplasty hypospadias repair.
Complications
Complications occurred in 21 (21%) patients, 10 in Group A and 11 in Group B, which was not statistically significantly different (P = 0.5). Urethrocutaneous fistula was the most common early complication occurring in 13 patients (six in Group A and seven in Group B) following removal of the catheter, again with no statistically significant difference between the groups (P > 0.6). The size of urethrocutaneous fistula was <2 mm in nine patients (four in Group A and five in Group B), and 3–5 mm in the remaining four patients (two in Group A and two in Group B), with no significant difference between the groups (P > 0.6). Of the nine patients with urethrocutaneous fistula of <2 mm, spontaneous closure of fistula occurred in eight patients during follow-up, whilst one patient required fistula repair after 6 months. However, fistula repair was necessary in all four patients with urethrocutaneous fistula of 3–5 mm after 6 months. In all these patients, no further urethrocutaneous fistula occurred at 6 months follow-up after fistula repair. Other important early postoperative complications included partial superficial wound infection (one in each group; P > 0.7) that improved on conservative treatment with no occurrence of urethrocutaneous fistula, and partial glans dehiscence with ventral migration of the neomeatus (one in each group; P > 0.7). In both patients with partial glans dehiscence, glansplasty was done after 6 months. There was no occurrence of complete wound dehiscence in any of the patients in either group. Late postoperative complications included meatal stenosis (one in each group; P > 0.7) and urethral stricture (one in each group; P > 0.7). Both meatal stenosis and urethral stricture responded to regular weekly meatal dilatation and urethral dilatation for 2–3 months ().
Urinary stream during micturition
Of 100 patients, the 77 without any postoperative complication had a good single urinary stream (38 in Group A and 39 in Group B). The remaining two patients in Group A without any postoperative complication had a splayed but good urinary stream after removal of catheter that improved on regular follow-up. The urinary stream was single and good in two patients (one in each group) with superficial wound infection, whilst it was splayed and good in two patients with partial glans dehiscence. Patients with meatal stenosis and urethral stricture initially had a single but thin urinary stream that improved on serial meatal dilatation and urethral dilatation.
Aesthetic appearance
Aesthetic appearance was satisfactory in all patients, with average aesthetic scores of 8–9 in all patients in both groups except in two (one in each group) with partial glans dehiscence and six with large fistula postoperatively.
Discussion
The goal of hypospadias repair is to create cosmetically and functionally normal penis that should be straight during erection, with a vertically slit-like meatus at the tip of the penis and adequate calibre urethra promoting a single and coherent urinary stream in a standing position. In an attempt to achieve these goals of hypospadias repair >250 reported methods of hypospadias repair have been described and even newer techniques and their modifications continue to evolve. Different types of urethroplasty techniques involve simple tubularisation of the urethral plate, midline incision and tubularisation of urethral plate (TIP), use of adjacent skin flaps, free skin grafts, buccal mucosal grafts, and mobilised vascular flaps (mostly using inner preputial skin) [Citation1,Citation11,Citation20]. Amongst these, the TIP repair is more versatile than other repairs and has gained widespread acceptance for hypospadias repair especially for distal hypospadias. The fact that it is a consistent and easily reproducible technique, which produces acceptable cosmetic and functional results in a timely manner, is a testament to its simplicity.
Variations in surgical techniques and various other factors can affect the functional and cosmetic outcome of the operation [Citation1–Citation19]. However, the exact roles of these factors are yet to be determined. Whilst use of absorbable sutures for hypospadias repair has been universally accepted, there is no general agreement on the suturing technique (interrupted or continuous). The choice of suturing technique in hypospadias repair is mainly dictated by surgeon’s preference. Moreover, the method of the suturing technique may affect the outcome of hypospadias repair as in bowel anastomosis. The effect of various suturing techniques has been best studied in bowel anastomosis and it has been found that the use of an interrupted-suturing technique for bowel anastomosis results in a decreased complication rate as compared to continuous suturing [Citation21]. Similarly, the effect of suturing technique on outcome of hypospadias repair has also been studied [Citation7–Citation11], but still there are no specific guidelines for the suturing technique.
In their study, Ulman et al. [Citation9] compared the use of 6–0 polyglactin in a single layer, full thickness, uninterrupted fashion to subcuticular suturing in uninterrupted fashion with 7–0 polydioxanone. They found that use of a subcuticular 7–0 continuous suture was associated with a lower incidence of complications as compared to full-thickness suture urethroplasty in hypospadias repair. Similarly, Khan et al. [Citation11] also found that the use of an inverting continuous suture was associated with a lower incidence of urethrocutaneous fistula as compared to over-and-over suture continuous suture urethroplasty in hypospadias repair.
In their study, El-Sherbiny et al. [Citation10] found that on univariate analysis suturing technique was a significant risk factor that could affect the outcome of hypospadias repair. They found that on univariate analysis, the use of a running suture was significantly associated with a higher fistula rate (23%) as compared to an interrupted suturing technique (9%). However, on multivariate analysis they found that the suturing technique had no independent significance. In another univariate analysis study, Sarhan et al. [Citation7] found no significant difference in the fistula rate after an interrupted (15%) or continuous suture (12.5%) technique in hypospadias repair. Snodgrass et al. [Citation22], in their study, also found no difference in urethroplasty complications in patients on the basis of sutures and suturing techniques. Our present study also supports the findings of these studies, as we found no significant difference between the fistula rate amongst the interrupted- (12%) and continuous-suturing (14%) techniques in hypospadias repair. Similarly, there was no significant difference in overall outcomes of the interrupted- (20%) and continuous-suturing (22%) techniques in hypospadias repair. An advantage of our present study is that it was a prospective randomised study similar to that reported by Sarhan et al. [Citation7]. A limitation of our study is that surgeons were not blinded to the suturing techniques in both groups, which may result in bias in outcome. However, we tried to eliminate any bias in outcome assessment by assigning the outcome assessment to author-3 and author-4, who were blinded to the type of suturing techniques used for urethroplasty in the patients selected for the study. Beside this, in our present study we matched most of the factors that could affect outcome of hypospadias repair in both groups, to concentrate on the effect of the suturing technique on the outcome of hypospadias repair so that the chance of error in statistical analysis due to the presence of confounding factors might be minimised. Another limitation of the present study is the small sample size in both groups, therefore the power of study was low and further studies with larger sample sizes are required to support these findings.
Conclusions
In the present study, the type of suture technique had no significant effect on the occurrence of complications after Snodgrass hypospadias repair and thus suturing choice depends on surgeon preference. However, due to the small sample size of the present study, further studies with larger sample sizes are required to support this conclusion.
Conflict of interest
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- W.T.SnodgrassHypospadiasA.J.WeinL.R.KavoussiA.C.NovickA.W.PartinC.A.PetersCampbell-Walsh urology10th ed.2012Elsevier SaundersPhiladelphia35023536
- M.C.UygurD.UnalM.O.TanC.GermiyanoğluD.ErolFactors affecting outcome of one-stage anterior hypospadias repair: analysis of 422 casesPediatr Surg Int182002142146
- C.GermiyanoğluB.NuhoğluA.AyyildizK.T.AkgülInvestigation of factors affecting result of distal hypospadias repair: comparison of two techniquesUrology682006182185
- T.YildizI.N.TahtaliD.C.AtesI.KelesZ.IlceAge of patient is a risk factor for urethrocutaneous fistula in hypospadias surgeryJ Pediatr Urol92013900903
- A.J.HollandG.H.SmithEffect of the depth and width of the urethral plate on tubularized incised plate urethroplastyJ Urol1642000489491
- M.T.NguyenW.T.SnodgrassM.R.ZaontzEffect of urethral plate characteristics on tubularized incised plate urethroplastyJ Urol171200412601262
- O.SarhanM.SaadT.HelmyA.HafezEffect of suturing technique and urethral plate characteristics on complication rate following hypospadias repairs: a prospective randomized studiesJ Urol1822009682686
- O.M.SarhanA.S.El-HefnawyA.T.HafezM.T.ElsherbinyM.E.DawabaA.M.GhaliFactors affecting outcome of tubularized incised plate (TIP) urethroplasty: single-center experience with 500 casesJ Pediatr Urol52009378382
- I.UlmanV.ErikciA.AvanoğluA.GökdemirThe effect of suturing technique and material on complication rate following hypospadias repairEur J Pediatr Surg71997156157
- M.T.El-SherbinyA.T.HafezM.S.DawabaA.A.ShorrabM.A.BazeedComprehensive analysis of tubularized incised-plate urethroplasty in primary and re-operative hypospadiasBJU Int93200410571061
- B.A.KhanM.A.ShahF.B.KhanComparative study of inverting suture line versus over and over continuous suturing in hypospadias repairJ Ayub Med Coll Abbottabad2120093436
- J.G.BorerA.B.RetikHypospadiasA.J.WeinL.R.KavoussiA.C.NovickA.W.PartinC.A.PetersCampbell-Walsh urology9th ed.2007Elsevier SaundersPhiladelphia37033744
- S.P.HakimP.A.MerguerianR.RabinowitzL.D.ShortliffeP.H.McKennaOutcome analysis of the modified Mathieu hypospadias repair: comparison of stented and unstented repairsJ Urol1561996836838
- K.Y.ChinD.BurchetteR.UppalUrethral stent in hypospadias repairJ Plast Reconstr Aesthet Surg66201311581160
- P.D.Furness3rdJ.HutchesonSuccessful hypospadias repair with ventral based vascular dartos pedicle for urethral coverageJ Urol169200318251827
- D.B.MeirP.M.LivneIs prophylactic antimicrobial treatment necessary after hypospadias repair?J Urol171200426212622
- N.KanaroglouE.WehbiA.AlotayD.J.BagliM.A.KoyleA.J.Lorenzoet al.Is there a role for prophylactic antibiotics after stented hypospadias repair?J Urol190201315351539
- U.S.ChatterjeeM.K.MandalS.BasuR.DasT.MajhiComparative study of dartos fascia and tunica vaginalis pedicle wrap for the tubularized incised plate in primary hypospadias repairBJU Int94200411021104
- Y.HayashiK.MizunoY.MoritokiA.NakaneT.KatoS.Kurokawaet al.Can spongioplasty prevent fistula formation and correct penile curvature in TIP urethroplasty for hypospadias?Urology81201313301335
- R.SubramaniamA.F.SpinoitP.HoebekeHypospadias repair: an overview of the actual techniquesSemin Plast Surg252011206212
- J.M.BurchR.J.FrancioseE.E.MooreW.L.BifflP.J.OffnerSingle layer continuous versus two-layer interrupted intestinal anastomosis: a prospective randomized trialAnn Surg2312000832837
- W.T.SnodgrassN.BushN.CostTubularized incised plate hypospadias repair for distal hypospadias repairJ Peditr Urol62010408413