Abstract
Objectives To present the current state of the art in various robot-assisted microsurgical procedures in male infertility and review the latest literature, as the technology in infertility procedures has substantially developed since the incorporation of the Vinci® robotic platform (Intuitive Surgical, Inc., Sunnyvale, CA, USA).
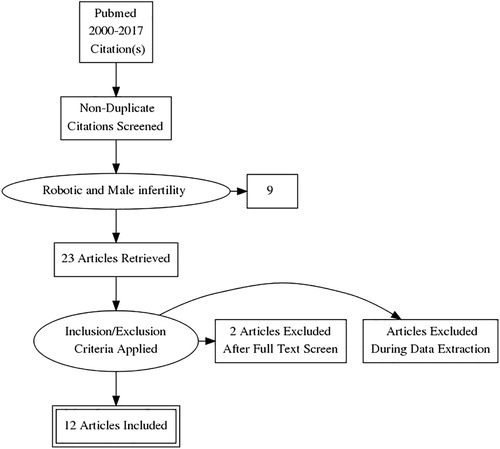
Materials and methods The search strategy in this review was conducted in accordance with Cochrane guidelines and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). A search strategy was conducted in MEDLINE, PubMed and the Cochrane electronic databases (from 2000 to present) to identify studies that included both robotic and male infertility.
Results In all, 23 studies were found, 12 of which met our inclusion criteria. Articles were excluded if the study did not include both male infertility and robotics.
Conclusions Robotic assistance for microsurgical procedures in male infertility appears to be safe and feasible. It has several advantages including elimination of tremor, multi-view magnification, additional instrument arms, and enhanced dexterity with articulating instrument arms. It also has a short learning curve with a small skin incision. However, larger, prospective studies are needed to establish the clinical benefits over standard microsurgery.
Abbreviations:
- ART
- assisted reproductive technology
- 3D
- three-dimensional
- FDA
- USA Food and Drug Administration
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- MeSH
- Medical Subject Heading
- TESE
- testicular sperm extraction
- RAVV
- robot-assisted vasovasostomy
- RAVE
- robot-assisted microsurgical vasoepididymostomy
- RAVx
- robot-assisted microsurgical varicocelectomy
- RCT
- randomised controlled trial
- US
- ultrasonography
Introduction
In 1970s, the operative microscope was introduced into male infertility procedures. Since then, several developments have occurred in assisted reproductive technology (ART) [Citation1,Citation2]. The technology in infertility procedures has evolved substantially since the incorporation of the da Vinci® robotic platform (Intuitive Surgical, Inc., Sunnyvale, CA, USA) into microsurgical procedures [Citation3].
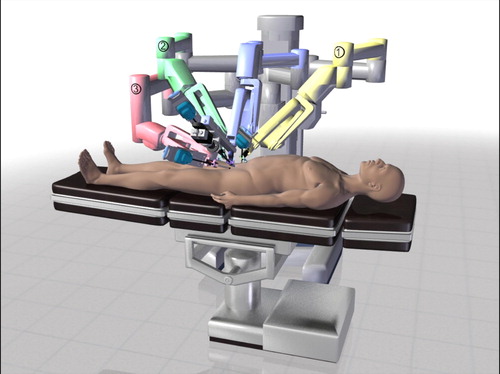
The da Vinci surgical system is currently the only commercially available USA Food and Drug Administration (FDA) approved robotic platform. Today all types of microsurgical procedures for male infertility can be performed using this robotic platform [Citation3]. The latest version of the da Vinci robot features a high-resolution three-dimensional (3D) view (with up-to × 10–15 magnification) and three robotic instrument arms. These instruments are capable of six degrees-of-freedom, thus mimicking the surgeon’s hand, wrist and finger movements with 180° articulation and 540° rotation. It enhances the ability of the surgeon to rotate instruments to a wider range than the human hand and provides a new capability in microsurgery. The robotic instrument arms also eliminate physiological tremors and provide motion scaling. The surgeon console provides a comfortable, ergonomic interphase to minimise surgeon fatigue. Having an extra third robotic instrument arm also allows the surgeon to control one additional instrument and be less reliant on the surgical bedside assistant. This extra arm can also hold adjunctive imaging or sensing tools, e.g. a Doppler ultrasonography (US) probe and provide additional real-time inputs to aid the surgeon [Citation4].
Abbou et al. [Citation5] first reported the use of robot-assisted laparoscopic radical prostatectomy in 2000 to help alleviate some of the surgeon fatigue and technical limitation issues of laparoscopy.
As robot-assisted laparoscopic procedures became more widespread, the potential for using this platform for robot-assisted microsurgery was also explored in animal studies [Citation6–Citation8]. These studies were then followed by early human trials [Citation9–Citation11]. Further exploration of the use of this platform in larger studies is ongoing [Citation12].
The present article reviews the latest literature in robot-assisted microsurgical procedures in male infertility: microsurgical vasectomy reversal, microsurgical subinguinal varicocelectomy, and microsurgical testicular sperm extraction (micro-TESE).
Material and methods
The search strategy was conducted in accordance with Cochrane guidelines and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [Citation13]. A search strategy was conducted in MEDLINE, PubMed and the Cochrane electronic databases (from 2000 to present) to identify studies that included both robotic and male infertility. The search was conducted using the following keywords; ‘robotic’, ‘robot-assisted’ and ‘male infertility’. Medical Subject Heading (MeSH) phrases included: (‘Robotic’ [MeSH]) AND (‘male infertility’ [MeSH]), (‘Robotics’ [Mesh]) AND (‘Andrology’ [MeSH]), (‘Varicocelectomy’ [MeSH]) AND (‘Robotics’ [MeSH]). Both retrospective and comparative studies were included ( ). The language of the articles was restricted to English and articles were excluded if the study did not include both male infertility and robotics.
Results
After excluding duplicate articles, eligible articles were assessed by their full text and 23 articles were eventually included in the systematic review. In all, 12 articles met our inclusion criteria and nine were excluded as they did not meet our inclusion criteria. After full text screening two more articles were excluded as they did not contain complete male infertility data in the manuscript. These 12 studies discussed the role of the robotic in male infertility as regards vasectomy reversal, varicocelectomy, and TESE.
Robot-assisted microsurgical vasectomy reversal
Vasectomy is the method of contraception chosen by >500,000 American men annually, and by upwards of 8% of married couples worldwide. About 2–6% of American men will ultimately undergo vasectomy reversal [Citation14].
Vasectomy reversal was one of the most uniquely difficult challenging procedures in urology until the introduction of the operating microscope, which improved outcomes and performance of these procedures [Citation15]. However, these techniques require dedicated training, experience, and a skilled microsurgical assistant. Robot-assisted microsurgical approaches with the da Vinci robotic platform can provide some advantages to overcome some of these challenges. Parekattil and Gudeloglu [Citation12] reported comparable outcomes for robot-assisted microsurgical vasectomy reversal (110 patients) compared with the pure microsurgical technique (45 patients). The median clinical follow-up was 17 months. The median (range) duration from vasectomy in the robot-assisted vasovasostomy (RAVV) group was 7 (1–21) years and 6.5 (1–19) years in the microscopic group. The median age of the patients in the RAVV group was 41 years and 39 years in the microscopic group. A significantly better patency rate of 96% was achieved in the RAVV cases vs 80% in microscopic group. Pregnancy rates (within 1 year postoperatively) did not differ significantly between the two groups: 65% for the RAVV group and 55% for the microscopic group. Operative duration (skin to skin) started at 150–180 min initially for the first 10 cases of RAVV. However, the median (range) operative duration for RAVV overall was significantly decreased at 97 (40–180) min compared with microscopic group at 120 min. The median (range) operation duration for robot-assisted microsurgical vasoepididymostomy (RAVE), at 120 (60–180) min, was also significantly faster than the microscopic group at 150 min. Kavoussi [Citation16] also reported similar outcomes when he compared both groups.
Santomauro et al. [Citation17] reported a 93% patency rate in 20 patients who underwent RAVV. In this study, surgical residents (novice surgeons) were allowed to perform RAVV on one side, and the staff surgeon (experienced surgeon) performed the anastomosis on the contralateral side. The operative time between the experienced and novice surgeons was not statistically significantly different. This study illustrated that the robotic platform could potentially be used to decrease the learning curve for microsurgery.
Technique and outcomes
Both robotic and pure microsurgical approaches are performed with the same surgical principles [Citation12,Citation18]. The two ends of the vas deferens are prepared through a scrotal incision and the proximal (testicular) vas fluid is assessed to see if any sperm are present. RAVV is performed if sperm are found in the proximal vas deferens. If no sperm are found in the proximal vas deferens, a RAVE is then performed. The da Vinci robotic platform is docked on the right side with the patient supine. Black diamond micro-forceps are used as needle drivers in the left and right arms, and the Potts scissors in the fourth arm are used to cut tied sutures (). This configuration allows the surgeon to control three instruments, thus obviating the need for a skilled microsurgical assistant.
Suture materials and surgical techniques are similar to those used in standard microsurgery. Eight to 10 9-0 nylon sutures are used for the muscularis anastomosis. Five to six double-arm 10-0 nylon sutures are used for mucosal lumen anastomosis ( ). The two posterior 9-0 sutures are first placed to anastomose the posterior muscularis plate. Two 10-0 posterior sutures are then used to anastomose the posterior mucosal plate. Four to five 10-0 anterior sutures are placed to complete the mucosal lumen anastomosis. Six to eight 9-0 nylon sutures are used to complete the anterior muscularis anastomosis.
Fig. 3 View from surgeon console during RAVV. Main view from the camera system of the da Vinci robotic platform in the middle, the real-time image from the right side with the andrology optical microscope (×100), and the view from the left side with the VITOM® (Karl Storz GmbH & Co. KG, Tuttlingen, Germany) camera view for enhanced magnification.
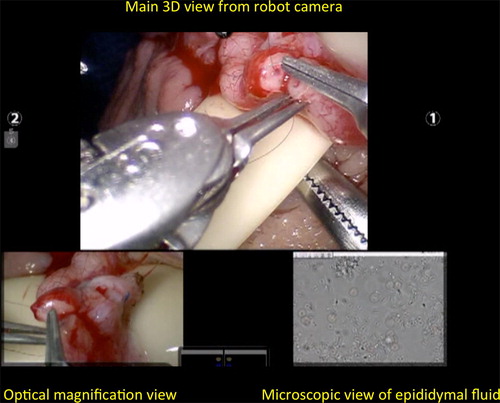
In RAVE, two double-arm 10-0 sutures are used for vasal mucosal lumen to epididymal tubule anastomosis ( ) using a longitudinal intussusception technique. The vasal muscularis layer is sutured to the epididymal tunica using six to eight 9-0 nylon sutures.
Fig. 4 View from surgeon console during RAVE. Main view from the camera system of the da Vinci robotic platform in the middle, the real-time image from the left side with the andrology optical microscope (×100), and the view from the right side with the VITOM camera view for enhanced magnification.
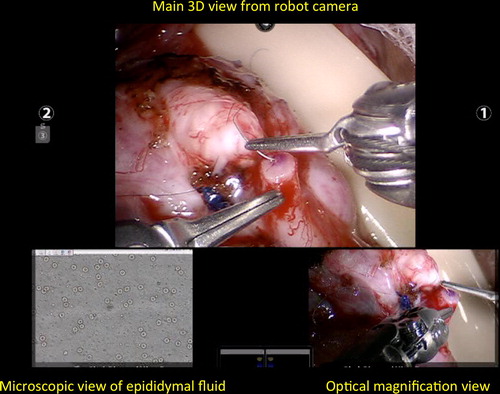
The 0° camera of the da Vinci robotic platform provides up to × 12–15 magnification. This five-arm robotic approach enables microsurgeons to perform challenging manoeuvres, including ultrafine suture placement and knot tying at two different focal lengths (two different camera views, each at a different magnification), without needing to zoom in and out. The simultaneous viewing capabilities also allow microsurgeons to evaluate seminal fluid or tissues without having to stop operating.
Robot-assisted microsurgery also allows for novel microsurgical approaches; it allows microsurgery to be performed in locations of the body that would otherwise be difficult to access with open and standard microscopic techniques. Trost et al. [Citation18] described the first bilateral intracorporeal RAVV in a patient who had bilateral iatrogenic vasal obstruction from prior bilateral inguinal hernia repair. They reported a successful minimally invasive bilateral intracorporeal anastomosis. This procedure requires a very large abdominal incision with standard microsurgical and open approaches but with the robotic approach it can be performed with only four small skin incisions (port sites, <1 cm each). Barazani et al. [Citation19] reported the first case of intra-abdominal RAVV used to repair obstructive azoospermia resulting from prior laparoscopic vasectomy.
Our group reported outcomes for 180 vasectomy reversal procedures (106 RAVV, 74 RAVE), with 97% and 55% success rates in the RAVV and RAVE procedures, respectively. The median operative durations (skin to skin) were also reasonable, at 120 min for RAVV and 150 min for RAVE [Citation20].
Robotics in the management of varicocele
The presence of a varicocele leads to a two-fold increase in the likelihood of having abnormal semen analysis parameters in men seeking infertility treatment [Citation21]. Varicocelectomy can lead to significant improvements in semen analysis parameters and a meta-analysis showed significant improvements in sperm count and motility regardless of the varicocelectomy technique [Citation22].
Results from a prospective, randomised controlled trial (RCT) from Saudi Arabia compared subinguinal microsurgical varicocele repair to observation [Citation23]. A total of 145 participants had follow-up within 1 year; spontaneous pregnancy was achieved in 13.9% of controls compared with 32.9% of treated men (odds ratio 3.04). This study provided evidence of the superiority of varicocelectomy over observation in infertile men with palpable varicoceles and impaired semen quality.
The subinguinal microsurgical varicocelectomy approach has higher spontaneous pregnancy rates, lower postoperative recurrence and lower complication rates when compared to other techniques [Citation24].
The initial study showing the safety, feasibility and comparable outcomes of robotic assistance in subinguinal microsurgical varicocelectomy was published by Shu et al. [Citation10] in 2008. They described elimination of tremor and the stable, ergonomic platform as benefits of the robotic approach. Parekattil et al. [Citation4], further explored this technique in a canine spermatic cord as they performed a prospective RCT of microscopic varicocelectomy vs robot-assisted microsurgical varicocelectomy (RAVx) in a canine varicocele model. In all, 12 canine varicocelectomies were randomised into two arms of six: standard microscopic varicocelectomy vs RAVx. There were no vessel injuries or knot failures in either group. There was no significant difference in set-up duration between the robot and operative microscope. They found a significantly faster operative time with RAVx when compared to the standard microsurgical approach (RAVx mean duration 9.5 min, whilst in standard microscopic varicocelectomy the mean duration was 12 min).
Mechlin and McCullough [Citation25] reported results of their initial experience with RAVx. They retrospectively reviewed surgical outcomes for patients who underwent varicocelectomy either by a standard microsurgical approach (34 patients) or RAVx (33 patients) by a single surgeon at an academic centre. They reported no significant difference in operative time when comparing RAVx to standard microsurgical varicocelectomy (57 min for RAVx vs 49 min for the microscopic group). They concluded also that the learning curve and operative time were progressively diminishing in their most recent cases. Ellen et al. [Citation26] reported a similar conclusion when they compared both groups and found that their operative time decreased in their recent cases.
Technique and outcomes
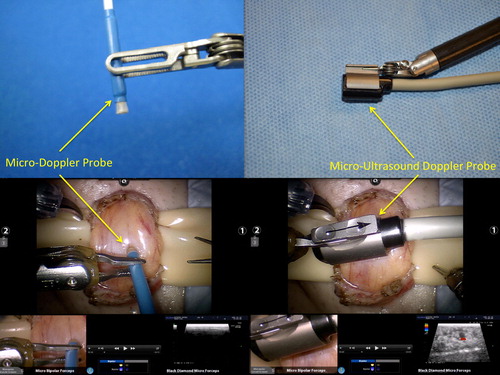
A subinguinal approach is used to access the spermatic cord beyond the external inguinal ring. The cord is then brought up to the skin and held in place using a tongue blade platform. The cremasteric muscle layer is then separated and dilated veins are found and ligated with 3-0 silk ties using robotic microsurgical instruments [Citation12].The Black diamond micro-forceps are used in the right arm, the micro-bipolar forceps in the left arm, and the curved monopolar scissors in the fourth arm. Previous studies have shown that 75% of patients have multiple testicular arteries in the spermatic cord and at the subinguinal level 95% of these arteries are surrounded by adherent veins [Citation27]. Thus, to avoid any accidental injury to the testicular arteries during the varicocelectomy, we routinely use a micro-Doppler US probes to assess the location of the arteries and veins. The use of the robotic platform allows surgeons to use this probe real-time with the additional arm to sense the flow in the artery whilst performing vein ligation simultaneously with the other two arms. Currently, there are two available micro-Doppler US probes: VTI (Vascular Technology Inc., Nashua, NH, USA) provides an easy to use, audible so disposable micro-Doppler probe ( ) and Aloka (Hitachi-Aloka, Tokyo, Japan) has a micro-Doppler US probe () that provides full depth US imaging of the spermatic cord with Doppler flow sensing as well. The output from this probe can be sent directly to the surgeon console to provide real-time simultaneous imaging whilst the surgeon is operating.
Fig. 5 Intraoperative Doppler US systems (left side audible micro-Doppler, right side visual micro-Doppler).
In our group we have a total of 319 patients that have undergone targeted robot-assisted microsurgical denervation of the spermatic cord and varicocelectomy for varicocele with pain. The median patient age was 34 years and 65% of the patients had improvement in their sperm parameters (sperm count and motility), and 73% had a significant reduction in pain.
Robot-assisted micro-TESE
Micro-TESE has the highest sperm retrieval rates amongst various sperm retrieval techniques in patients with non-obstructive azoospermia [Citation28]. The use of robotic assistance for micro-TESE provides the surgeon with real-time simultaneous imaging of the testicular tissue and evaluation by the embryologist whilst the surgeon is operating. This is helpful for identifying areas or tubules that may be more likely to harbour sperm. As future sperm imaging detection techniques evolve (such as probe-based confocal laser endomicroscopy and multiphoton microscopy), integration of this technology will probably be easier with the robotic platform than with standard microsurgery.
Technique and outcomes
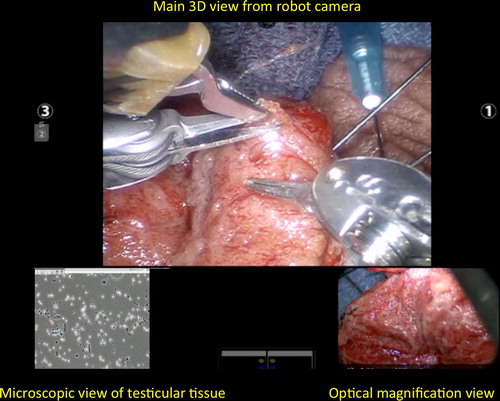
The procedure is performed with the patient supine. The testicles are delivered through a midline scrotal incision and the da Vinci robotic platform is docked from the patient’s right side after the testicular tunica is incised. Black diamond micro-forceps, bipolar micro-forceps, and the Potts scissors are loaded into the right, left, and the fourth arms, respectively. The surgeon view on the robotic console is seen in . The microsurgeon can easily identify dilated seminiferous tubules with the da Vinci 3D-camera and the extra magnified VITOM® (Karl Storz GmbH & Co. KG, Tuttlingen, Germany) image, and simultaneously evaluate the tissues sampled by the embryologist using the × 100 phase-contrast microscope.
Fig. 6 View from surgeon console during robot-assisted micro-TESE. Main view from robotic camera. Real-time image from andrology laboratory microscope on the left-hand corner. VITOM camera view for enhanced magnification on the right-hand corner.
Parekattil and Gudeloglu [Citation12] performed 12 robotic TESE procedures without any complications. It was a safe and feasible procedure for sperm retrieval and subjectively appears to make tissue handling and dissection slightly easier and ergonomic compared to micro-TESE.
New imaging technology is being developed that may better identify tubules that harbour sperm during micro-TESE [Citation29,Citation30] The robotic platform would provide an ideal platform for the integration of these types of adjunctive tools.
Conclusions
Robotic assistance for microsurgical procedures in male infertility appears to be safe and feasible. It has several advantages including elimination of tremor, multi-view magnification, additional instrument arms, and enhanced dexterity with articulating instrument arms. It also has a short learning curve with small skin incisions. However, larger, prospective studies are needed to establish the clinical benefits over standard microsurgery.
Conflicts of interest
The authors have no conflicts of interest to declare.
Acknowledgement
None.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- S.J.SilberMicrosurgery in clinical urologyUrology61975150153
- P.C.SteptoeR.G.EdwardsBirth after the reimplantation of a human embryoLancet21978366
- C.FlemingRobot-assisted vasovasostomyUrol Clin North Am312004769772
- S.J.ParekattilJ.V.BrahmbhattRobotic approaches for male infertility and chronic orchialgia microsurgeryCurr Opin Urol212011493499
- C.C.AbbouA.HoznekL.SalomonA.LobontiuF.SaintA.Ciccoet alRemote laparoscopic radical prostatectomy carried out with a robot. Report of a caseProg Urol102000520523
- W.KuangP.R.ShinS.MatinA.J.ThomasJr.Initial evaluation of robotic technology for microsurgical vasovasostomyJ Urol1712004300303
- W.KuangP.R.ShinM.OderA.J.ThomasJr.Robotic-assisted vasovasostomy: a two-layer technique in an animal modelUrology652005811814
- J.SchiffP.S.LiM.GoldsteinRobotic microsurgical vasovasostomy and vasoepididymostomy: a prospective randomized study in a rat modelJ Urol171200417201725
- S.J.ParekattilM.S.CohenRobotic surgery in male infertility and chronic orchialgiaCurr Opin Urol2020107579
- T.ShuS.TaghechianR.WangInitial experience with robot-assisted varicocelectomyAsian J Androl102008146148
- G.De NaeyerP.Van MigemP.SchattemanP.CarpentierE.FonteyneA.MottrieRobotic assistance in urological microsurgery: initial report of a successful in-vivo robot-assisted vasovasostomyJ Robot Surg12007161162
- S.J.ParekattilA.GudelogluRobotic assisted andrological surgeryAsian J Androl1520136774
- D.MoherA.LiberatiJ.TetzlaffD.G.AltmanPRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementInt J Surg82010336341
- E.W.KirbyM.HockenberryL.I.LipshultzVasectomy reversal: decision making and technical innovationsTransl Androl Urol62017753760
- S.J.SilberH.E.GrotjanMicroscopic vasectomy reversal 30 years later: a summary of 4010 cases by the same surgeonJ Androl252004845859
- P.K.KavoussiValidation of robot-assisted vasectomy reversalAsian J Androl172015245247
- M.G.SantomauroC.H.ChoeJ.O.L'EsperanceB.K.AugeRobotic vasovasostomy: description of technique and review of initial resultsJ Robot Surg62012217221
- L.TrostS.ParekattilJ.WangW.J.HellstromIntracorporeal robot-assisted microsurgical vasovasostomy for the treatment of bilateral vasal obstruction occurring following bilateral inguinal hernia repairs with mesh placementJ Urol191201411201125
- Y.BarazaniJ.KaoukE.S.SabaneghJr.Robotic intra-abdominal vasectomy reversal: a new approach to a difficult problemCan Urol Assoc J82014E439E441
- A.GudelogluJ.V.BrahmbhattS.J.ParekattilRobotic microsurgery in male infertility and urology-taking robotics to the next levelTransl Androl Urol32014102112
- World Health OrganizationThe influence of varicocele on parameters of fertility in a large group of men presenting to infertility clinicsFertil Steril57199212891293
- I.SchauerS.MadersbacherR.JostW.A.HübnerM.ImhofThe impact of varicocelectomy on sperm parameters: a meta-analysisJ Urol187201215401547
- T.A.Abdel-MeguidA.Al-SayyadA.TayibH.M.FarsiDoes varicocele repair improve male infertility? An evidence-based perspective from a randomized, controlled trialEur Urol592011455461
- S.CayanS.ShavakhabovA.KadiogluTreatment of palpable varicocele in infertile men: a meta-analysis to define the best techniqueJ Androl3020093340
- C.MechlinA.V.McCulloughRobotic microsurgical varicocele repair: initial experience and surgical outcomes from a single academic centerJ Urol189Suppl.2013e652e653
- J.EllenC.WelliverA.McCulloughA review of the robot assisted microsurgical varicocelectomy at Albany Medical CenterFertil Steril104Suppl.2015e291
- C.V.HoppsM.L.LemerP.N.SchlegelM.GoldsteinIntraoperative varicocele anatomy: a microscopic study of the inguinal versus subinguinal approachJ Urol170200323662370
- P.N.SchlegelNonobstructive azoospermia: a revolutionary surgical approach and resultsSemin Reprod Med272009165170
- B.B.NajariR.RamasamyJ.SterlingA.AggarwalS.ShethP.S.Liet alPilot study of the correlation of multiphoton tomography of ex vivo human testis with histologyJ Urol1882012538543
- M.TrottmannH.SteppR.SrokaM.HeideB.LiedlS.Reeseet alProbe-based confocal laser endomicroscopy (pCLE) – a new imaging technique for in situ localization of spermatozoaJ Biophotonics82015415421