Abstract
Objective:
To evaluate the efficacy of silodosin therapy, as a new α-adrenergic receptor (α-AR) blocker, on the success rate of semi-rigid ureteroscopy (URS) for the management of large distal ureteric stones.
Patients and methods:
This prospective study recruited 127 adult patients with single distal ureteric stone of ≥1 cm. The patients were randomly allocated to two groups: the first group included 62 patients who received silodosin (8 mg) for 10 days before URS (Silodosin group), whilst the second group included 65 patients who received placebo, in the form of multivitamins, for 10 days before URS (Placebo group). All patients underwent URS and a pneumatic lithoclast was used for stone fragmentation.
Results:
The mean (SD) operative time was shorter in the Silodosin group compared with the Placebo group, at 41.61 (4.67) vs 46.85 (4.6) min, respectively. Furthermore, advancing the ureteroscope to access the stone failed in a statistically significant number of patients in the Placebo group compared with the Silodosin group (13 vs two, respectively). The complication rate was significantly higher in the Placebo group compared with the Silodosin group (20% vs 6.4%, P = 0.036). Additionally, the need for postoperative analgesia was significantly lower in the Silodosin group compared with the Placebo group (8.1% vs 26.2%, P = 0.009).
Conclusion:
Silodosin therapy prior to URS management of large distal ureteric stones seems to be associated with better advancing of the ureteroscope to access the stone, shorter procedure time, higher stone-free rate, lower incidence of complications, and lesser need for postoperative analgesia.
Introduction
One of the most common causes for visiting an emergency department is ureteric stones, which affect ∼12% of males and ∼6% of females during their lifetime [Citation1,Citation2]. Distal ureteric stones represent ∼70% of these stones, which are mostly symptomatic [Citation3–Citation6]. Semi-rigid ureteroscopy (URS) has been shown to have high success rates for treating distal ureteric stones in many studies [Citation7,Citation8]. However, URS is associated with some drawbacks, which may be risky and sometimes problematic [Citation9]. The distal part of the ureter is rich with α-adrenergic receptors (α-ARs) [Citation10], which are responsible for phenylephrine-induced ureteric smooth muscle contraction [Citation11]. In some cases, advancing the ureteroscope towards the stone after passing the ureteric orifice is found to be difficult or impossible. In such situations, a JJ stent is inserted for ureteric dilatation and the URS is postponed to another later session. The present study was designed based on this observation and the fact that α-AR blockers inhibit basal tone and peristalsis leading to dilatation of the ureteric lumen [Citation12]. In the present study, we prospectively investigated the efficacy of silodosin therapy, as new α-AR blocker molecule, pre-URS for the management of large distal ureteric stones, with the hypothesis that it would increase the chance of advancing the ureteroscope to access the stone, and make it easier and safer.
Patients and methods
Study design
This prospective randomised study was carried out at Benha University Hospitals between October 2015 and January 2017. Written informed consent was obtained from all recruited patients and performed according to the local ethics of our institutes. The inclusion criteria comprised adult patients with a single distal ureteric stone of ≥1 cm who accepted to participate. Patients with prior medical expulsive therapy, a single kidney, bilateral ureteric stones, history of previous ureteric surgery, high-grade hydronephrosis, ureteric pathology, pregnancy, history of stone passage, and prior long-term α-AR blocker use for the management of BPH, were excluded. For all patients, preoperative radiological investigations were done in the form of plain abdominal radiograph of the kidneys, ureters and bladder (KUB), pelvi-abdominal ultrasonography (US), and non-contrast CT (NCCT). Stone size was calculated by measuring the largest dimension on KUB or NCCT. Urine culture, complete blood count, serum creatinine, bleeding profile, and hepatitis markers were assessed as routine preoperative laboratory tests. Using a closed-envelopes method, patients were randomly allocated to two groups. The first group included 62 patients who received silodosin (8 mg) for 10 days before URS (Silodosin group), whilst the second group included 65 patients who received placebo, in the form of multivitamins supplementation, for 10 days before URS (Placebo group). All patients stopped taking silodosin or placebo immediately postoperatively. Urologists who carried out the operations were blinded to both groups.
Operative technique
Under spinal anaesthesia, patients were put in lithotomy position and cystourethroscopy was performed to examine the urethra and the bladder, and to detect the intended ureteric orifice. A 0.089 cm (0.035 in.) guidewire was introduced through the intended ureteric orifice under fluoroscopic guidance until reaching the kidney. Next, the ureteroscope (8/9.5 F, Karl Storz GmbH & Co. KG, Tuttlingen, Germany) was introduced to the ureteric orifice. Whenever necessary, hydrodilatation with the help of the hand irrigation pump or balloon dilatation, was used to dilate the ureteric orifice to facilitate ureteroscope entrance. After this, the ureteroscope was advanced into the ureter to access the stone and disintegration was performed using a pneumatic lithoclast. The fragments were then removed using a Dormia basket and/or forceps. At the end of the procedure, a 6-F ureteric catheter was inserted [Citation13]. The patients were assessed for stone clearance at 24–48 h after the procedure using KUB and pelvi-abdominal US, and the ureteric catheter was removed at 24 or 48 h. All patients were asked to attend clinic 4 weeks later to undergo follow-up assessment using KUB and pelvi-abdominal US. Patients were considered stone-free if there were either no significant stone fragments (≤0.2 cm) or no signs of hydronephrosis. The procedure was considered to have failed when there was an inability to forward the ureteroscope to access the stone and in this situation a JJ stent was inserted for more ureteric dilatation, and the URS was postponed for a later session. Fever was considered whenever the body temperature was ≥38 °C. Mucosal injury that required ureteric stenting intraoperatively or resulted in haematuria postoperatively was considered significant. Also, haematuria requiring i.v. fluids for >12 h was considered significant. The data of both groups, including, age, sex, stone size, operation time, results of advancing the ureteroscope to access the stones, need for dilatation of the ureteric orifice, complications, stone-free rate, and need for postoperative analgesia, were recorded and analysed.
Statistical analysis
The G* Power 3.1.9.2 was used for sample size calculation and the Statistical Package for the Social Sciences (SPSS®), version 20 for Windows (SPSS Inc., IBM Corp., Armonk, NY, USA), was used for data analysis. Descriptive data were presented as means ± standard deviations (SDs) or numbers and percentages. Fisher’s exact test was used to compare categorical variables, whilst the Student’s t-test was used to compare continuous variables. Statistical significance was considered for a two-tailed P value of <0.05.
Results
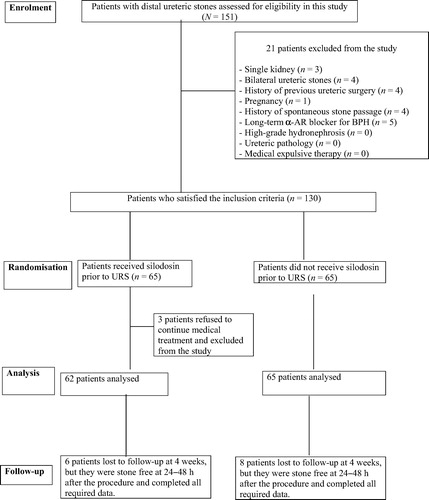
The total number of patients analysed was 62 and 65 in the Silodosin group and the Placebo group, respectively (). The patients’ and stone characteristics are given in . The mean (SD) age of patients was 38.27 (9.37) years in the Silodosin group and 39.67 (9.54) years in the Placebo group. In the Silodosin group, 62.9% of patients were male and 37.1% were female, whilst in the Placebo group, 60% were male and 40% were female. There were no statistically significant differences between the groups for the age and sex distribution of the patients. Also, there was no statistically significant difference between the groups for stone size, side, and density. The mean (SD) stone size was 1.26 (0.125) cm in the Silodosin group and 1.29 (0.129) cm in the Placebo group. There was no statistically significant difference between the Silodosin group and the Placebo group for the body mass index, at a mean (SD) of 27.55 (2.28) vs 27.8 (3.5) kg/m2, respectively. Operative and postoperative data are presented in . The operative time was significantly shorter in the Silodosin group than in the Placebo group, at a mean (SD) of 41.61 (4.67) vs 46.85 (4.6) min, respectively (P < 0.001). Advancing the ureteroscope to access the stones was successful in 60 patients (96.8%) in the Silodosin group compared with 52 (80%) in the Placebo group (P = 0.005). The need for ureteric orifice dilatation was significantly higher in the Placebo group compared with the Silodosin group, at 52.3% vs 19.35%, respectively (P < 0.001). The overall complication rate was significantly higher in the Placebo group compared with the Silodosin group, at 20% vs 6.4%, respectively (P = 0.036). In the Silodosin group, there was one case (1.6%) with stone migration up to the kidney, which was managed by shockwave lithotripsy (SWL) under spinal anaesthesia (Clavien–Dindo Grade IIIa). In the Placebo group, there were two cases of stone migration; in the first case the stone was removed by URS from the middle part of the ureter in the same session, so this case was not considered as a complication, whilst in the other case (1.5%), the stone migrated up to the kidney and was managed by SWL under spinal anaesthesia (Clavien–Dindo Grade IIIa). Fever occurred in one case in the Silodosin group and in three cases in the Placebo group. In all cases the fever abated within 48 h with antibiotic and antipyretic management (Clavien–Dindo Grade I). Haematuria occurred in one cases in the Silodosin group and five cases in the Placebo group, which was treated by i.v. fluid continuation for 24–48 h (Clavien–Dindo Grade I). In cases with haematuria, the ureteric catheter was removed after 48 h. There was mucosal injury intraoperatively in one case (1.6%) in the Silodosin group and four (6.2%) in the Placebo group (Clavien–Dindo Grade I). The need for postoperative analgesia was significantly lower in the Silodosin group than the Placebo group, at 8.1% vs 26.2% (P = 0.009). The stone-free rate was significantly higher in the Silodosin group (57/62) compared with the Placebo group (48/65) at 24–48 h (91.94% vs 73.85%, P = 0.009). After 4 weeks, 56 patients in the Silodosin group and 57 patients in the Placebo group attended follow-up. The stone-free status was confirmed in 53/56 in the Silodosin group compared with 43/57 in the Placebo group (94.64% vs 75.43%, P = 0.007).
Table 1 Patients’ and stone characteristics.
Table 2 Operative and postoperative data.
Discussion
In recent years, URS has become established as the optimal treatment for distal ureteric stones. Nevertheless, it is not risk free [Citation14]. Despite the fact that α-ARs are located in the proximal and the middle ureter, these receptors are more concentrated in the distal ureter [Citation15]. The α1a- and α1d-ARs are the most expressed subtypes in the distal ureter [Citation16]. Sasaki et al. [Citation17] reported that the α1a-AR subtype is responsible for the majority of the contraction process in the human ureter. Therefore, inhibition of these receptors should result in relaxation of ureteric smooth muscles and dilatation of the ureteric lumen [Citation18,Citation19]. The benefit of α-AR blockers as medical expulsive therapy for ureteric stones is established in the literature, as they increase the stone passage rate and minimise expulsion time [Citation20,Citation21]. Recently, silodosin was introduced as a highly selective α1a-AR blocker [Citation22,Citation23].
From our practice, we observed that in some cases of distal ureteric stones the ureteroscope failed to access the stone after passing the ureteric orifice. Based on this observation and the pharmacological characters of the silodosin molecule, we prospectively designed our present study to assess the efficacy of preoperative silodosin therapy on the outcome of semi-rigid URS for large distal ureteric stones.
In the literature, the mean time for the distal ureteric stone passage with silodosin therapy, as medical expulsive therapy, was 8.3 days [Citation24]. Therefore, patients in the Silodosin group received silodosin for 10 days before URS, as we suspected that 10 days was an adequate duration to relax the ureteric smooth muscles, thus facilitating the advancing of the ureteroscope.
To the best of our knowledge, the present study is the first limited to distal ureteric stones, as we thought that the results would be more apparent for distal ureteric stones than proximal and middle ureteric stones because α-AR are more concentrated in the distal part of the ureter.
Ahmed et al. [Citation25] reported that the use of tamsulosin (an α-AR blocker) as adjunctive therapy prior to semi-rigid URS for the management of proximal ureteric stones increased the success rate and minimised the rate of complications. Aydin et al. [Citation26] showed that administration of silodosin before URS for managing stones located at all levels of the ureter achieved a higher access rate with lower complications.
Ahmed et al. [Citation25] and Aydin et al. [Citation26] reported that access to the stone failed in 12.1% and 17% of cases, respectively. In the present study, advancing the ureteroscope to access the stones succeeded in 60/62 cases in the Silodosin group, whilst in the Placebo group success was achieved in 52/65 cases. This supports the finding that blocking of α-ARs located in the distal ureter leads to ureteric smooth muscle relaxation and decreases the force and frequency of the peristalsis [Citation10,Citation15].
There was a need for ureteric orifice dilatation in 12 patients (19.35%) in the Silodosin group compared with 34 (52.3%) in the Placebo group (P < 0.001). We suspect this significant difference is related to the effect of silodosin.
In the present study, the mean operative time was shorter in the Silodosin group than the Placebo group. This significant difference may be due to the time taken for ureteric orifice dilatation and for advancing the ureteroscope to access the stone, which was easier and faster in the Silodosin group. This result is congruent with Ahmed et al. [Citation25], who reported that operative time was shorter in patients who received tamsulosin (an α-AR blocker). However, Aydin et al. [Citation26] did not find a significant difference in the operative time between the studied groups.
In the present series, the stone-free rate was higher in the Silodosin group than in the Placebo group at 24–48 h (91.94% vs 73.85%, P = 0.009) and after 4 weeks (94.64% vs 75.43%, P = 0.007). This was close to the rates reported in various studies for URS management of distal ureteric stones, which range from 77.5% to 94.6% [Citation27,Citation28]. In the literature, the reported overall complication rates for URS range from 9% to 25% [Citation29–Citation31]. In the present study, the overall complication rate was higher in the Placebo group than the Silodosin group (20% vs 6.4%). Mucosal injury and haematuria were obvious complications in the Placebo group. This supports the notion that silodosin facilitates the advancing of the ureteroscope to the stone by relaxing the ureteric smooth muscles. In the literature, administration of α-AR blockers reduced the need for analgesia [Citation32,Citation33]. This is congruent with the results reported in the present study, as the need for postoperative analgesia was significantly lower in the Silodosin group than in the Placebo group. We consider that the success of advancing the ureteroscope to access the stones with ease, swiftly, and with less complications, as the cornerstone of the present study.
The fact that the procedures were performed by multiple surgeons could be considered a limitation of the present study. However, all the surgeons were consultants and had previously performed >100 semi-rigid URSs. We hope to see future randomised studies from other institutions for further confirmation of the efficacy of silodosin therapy prior to URS for the management of large distal ureteric stones.
Conclusion
Silodosin therapy prior to ureteroscopic management of large distal ureteric stones seems to be associated with better advancing of the ureteroscope to access the stone, shorter procedure time, higher stone-free rate, lower incidence of complications, and lesser need for postoperative analgesia.
Acknowledgement
The authors would like to thank all patients who participated in this study.
Notes
Peer review under responsibility of Arab Association of Urology.
References
- C.W.FwuP.W.EggersP.L.KimmelJ.W.KusekZ.KirkaliEmergency department visits, use of imaging, and drugs for urolithiasis have increased in the United StatesKidney Int832013479486
- G.C.CurhanEpidemiology of stone diseaseUrol Clin North Am342007287293
- V.RomeroH.AkpinarD.G.AssimosKidney stones: a global picture of prevalence, incidence, and associated risk factorsRev Urol122010e86e96
- A.A.KetabchiG.A.AziziolahiPrevalence of symptomatic urinary calculi in Kerman, IranUrol J52008156160
- A.TrinchieriEpidemiology of urolithiasis: an updateClin Cases Miner Bone Metab52008101106
- K.BensalahM.PearleY.LotanCost-effectiveness of medical expulsive therapy using alpha-blockers for the treatment of distal ureteral stonesEur Urol532008411418
- O.M.AboumarzoukS.G.KataF.X.KeeleyNabi G. Extracorporeal shock wave lithotripsy (ESWL) versus ureteroscopic management for ureteric calculiCochrane Database Syst Rev122011CD006029
- F.YencilekK.SaricaS.ErturhanF.YagciA.ErbagciTreatment of ureteral calculi with semirigid ureteroscopy: where should we stop?Urol Int842010260264
- M.IslamA.MalikUreteroscopic pneumatic versus extracorporeal shock wave lithotripsy for lower ureteral stonesJ Coll Physicians Surg Pak222012444447
- S.SigalaM.DellabellaG.MilaneseS.FornariS.FaccoliF.Palazzoloet al.Evidence for the presence of alpha1 adrenoceptor subtypes in the human ureterNeurourol Urodyn242005142148
- C.J.WangP.C.TsaiC.H.ChangEfficacy of silodosin in expulsive therapy for distal ureteral stones: a randomized double-blinded controlled trialUrol J13201626662671
- C.D.RicharsonC.F.DonatucciS.O.PageK.H.WilsonD.A.SchwinnPharmacology of tamsulosin: saturation binding isotherms and competition analysis using cloned alpha 1-adrenergic receptors subtypesProstate3319975559
- A.MoheyM.AlhefnawyM.MahmoudR.GomaaT.SolimanS.Ahmedet al.Fluoroless-ureteroscopy for definitive management of distal ureteral calculi: randomized controlled trialCan J Urol25201892059209
- N.R.Netto JúniorA.Claro JdeS.C.EstevesE.F.AndradeUreteroscopic stone removal in the distal ureter. Why change?J Urol157199720812083
- J.M.MalinJr.R.F.DeaneS.BoyarskyCharacterisation of adrenergic receptors in human ureterBr J Urol421970171174
- Y.ItohY.KojimaT.YasuiA.OkadaK.TozawaK.KohriExamination of alpha 1 adrenoceptor subtypes in the human ureterInt J Urol142007749753
- S.SasakiY.TomiyamaS.KobayashiY.KojimaY.KubotaK.KohriCharacterization of a (1)-adrenoceptor subtypes mediating contraction in human isolated uretersUrology772011e13e17
- A.UenoT.KawamuraA.OgawaH.TakayasuRelation of spontaneous passage of ureteral calculi to sizeUrology101977544546
- F.PorpigliaD.VaccinoM.BilliaJ.RenardC.CraccoG.Ghignoneet al.Corticosteroids and tamsulosin in the medical expulsive therapy for symptomatic distal ureter stones: single drug or association?Eur Urol502006339344
- M.S.GriwanS.K.SinghH.PaulD.S.PawarM.VermaThe efficacy of tamsulosin in lower ureteral calculiUrol Ann220106366
- M.A.SayedA.AbolyosrM.A.AbdallaA.S.El-AzabEfficacy of tamsulosin in medical expulsive therapy for distal ureteral calculiScand J Urol Nephrol4220085962
- D.J.MartinP.LluelE.GuillotA.CosteD.JammesI.AngelComparative alpha-1 adrenoceptor subtype selectivity and functional uroselectivity of alpha-1 adrenoceptor antagonistsJ Pharmacol Exp Ther2821997228235
- S.TatemichiK.KobayashiA.MaezawaM.KobayashiY.YamazakiN.ShibataAlpha1-adrenoceptor subtype selectivity and organ specificity of silodosin (KMD-3213)Yakugaku Zasshi1262006209216 [Article in Japanese]
- W.HuangP.XueH.ZongY.ZhangEfficacy and safety of silodosin in the medical expulsion therapy for distal ureteral calculi: a systematic review and meta-analysisBr J Clin Pharmacol8120161322
- A.F.AhmedA.MaaroufE.ShalabyS.AlshahraniM.El-FekyS.Khaledet al.Semi-rigid ureteroscopy for proximal ureteral stones: does adjunctive tamsulosin therapy increase the chance of success?Urol Int982016411417
- M.AydinM.F.KilinçA.YavuzG.BayarDo alpha-1 antagonist medications affect the success of semi-rigid ureteroscopy? A prospective, randomised, single-blind, multicentric studyUrolithiasis201710.1007/s00240-017-1026-6 [Epub ahead of print]
- L.Dell’AttiS.PapaTen-year experience in the management of distal ureteral stones greater than 10 mm in sizeG Chir372016273010.11138/gchir/2016.37.1.027
- O.M.ElashryA.M.ElgamasyM.A.SabbaM.Abo-ElenienM.A.OmarH.H.Eltatawyet al.Ureteroscopic management of lower ureteric calculiBJU Int102200810101017
- G.M.PremingerH.G.TiseliusD.G.AssimosP.AlkenC.BuckM.Gallucciet al.2007 guideline for the management of ureteral calculiJ Urol178200724182434
- P.GeavleteD.GeorgescuG.NiţăV.MirciulescuV.CauniComplications of 2735 retrograde semirigid ureteroscopy procedures: a single center experienceJ Endourol202006179185
- E.Perez CastroP.J.OstherV.JingaH.RazviK.G.StravodimosK.Parikhet al.Differences in ureteroscopic stone treatment and outcomes for distal, mid-, proximal, or multiple ureteral locations: the Clinical Research Office of the Endourological Society ureteroscopy global studyEur Urol662014102109
- I.CervenakovJ.FilloJ.MardiakSpeedy elimination of ureterolithiasis in lower part of ureters with the alpha 1 blockers – tamsulosinInt J Urol Nephrol3420022529
- S.K.SinghD.S.PawarM.S.GriwanJ.M.IndoraS.SharmaRole of tamsulosin in clearance of upper ureteral calculi after extracorporeal shock wave lithotripsy: a randomized controlled trialUrol J820111420