Abstract
Background
In this study we tested the new, single-use supraglottic airway device; i-gel with a non-inflatable cuff as an effective airway as conventional endotracheal tube. Gas leak was measured and compared with that of cuffed tracheal tube during volume controlled ventilation in elective laparoscopic cholecystectomy.
Methods
Sixty patients, ASA I–II, were randomly selected to the study. Standard anaesthetic technique was used for all patients. The i-gel was then inserted. The lungs were ventilated at three different tidal volumes (6, 8 and 10 ml kg−1) using volume controlled ventilation (VCV). The leak volume was calculated as the difference between the inspired and expired tidal volumes. The leak fraction was also calculated as the leak volume divided by the inspired tidal volume. These observations were recorded with every tidal volume before and after pneumoperitoneum with the i-gel and the conventional tracheal tube.
Results
Before pneumoperitoneum there was no significant difference in leak fraction between i-gel and tracheal tube at 6 and 8 ml kg−1 tidal volume. Significant differences were found after pneumoperitoneum at 8 and at 10 ml kg−1 before and after pneumoperitoneum.
Conclusion
We suggest that i-gel can be used as an alternative device to endotracheal tube during VCV for laparoscopic cholecystectomy provided that peak pressure does not exceed leak pressure.
1 Introduction
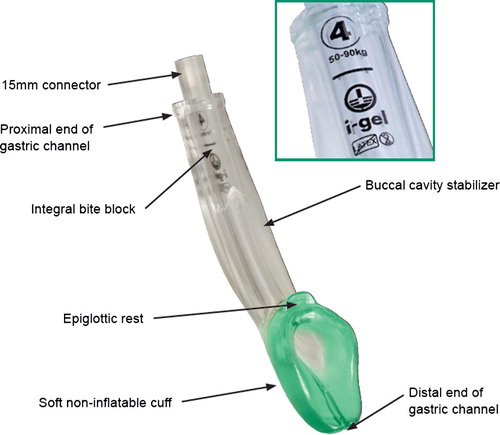
Supraglottic airway devices are used now for airway control during spontaneous and controlled ventilation under general anesthesia. The i-gel (Intersurgical Ltd., Wokingham, UK) is a new supraglottic airway device (SAD) made of thermoplastic elastomer which is soft, gel-like and transparent [Citation1]. The i-gel™ is an anatomical device achieving a mirrored impression of those structures without causing multidirectional forces of compression or displacement trauma to the tissues and structures in the vicinity. A drain tube is placed laterally to the airway tube that allows the insertion of a gastric tube (maximum 14 F gauges). Studies on Cadaver showed that i-gels effectively conformed to the perilaryngeal anatomy and consistently achieved proper positioning for supraglottic ventilation [Citation2]. Manikins studies and patients have shown that the insertion of the i-gel was significantly easier when compared with insertion of other SADs [Citation3,Citation4]. Few studies had been done to evaluate the use of i-gel during controlled ventilation but they did not evaluate its use during procedures with airway pressure more than 25 cm H2O [Citation5]. Our study was designed to evaluate the i-gel sealing pressure and as effective airway as cuffed tracheal tube during volume controlled ventilation in laparoscopic cholecystectomy.
2 Method
After ethics committee of New Jeddah Clinic Hospital (Jeddah, Saudi Arabia) approval and written informed consent 60 patients, 18–60 years old, ASA I–II, Mallampati class I or II, male and female were selected for elective laparoscopic cholecystectomy. Patients were randomly selected for airway management by either i-gel (I-group) or cuffed endotracheal tube (T-group) and data reading done before (B) and after (A) pneumoperitoneum to 14 mmHg in supine position. Patients with body mass index >35 kg m−2, difficult airway possibility, cervical spine problems, mouth opening <2.5 cm, full stomach and gastroesophageal reflux disease, were excluded. All patients received premedication midazolam 1 mg, ranitidine 50 mg and dansetron 4 mg intravenously, 45 min before surgery. We used Datex-Ohmeda; Aisys (GE healthcare) with standard monitor. Anesthesia protocol was made the same for all patients. Preoxygenation then induction of anesthesia was done by propofol 2–2.5 mg kg−1, fentanyl 1–1.5 μg kg−1 and neuromuscular relaxation achieved by rocuronium 0.8 mg kg−1 with increments of 0.15 mg kg−1 boluses to maintain TOF >1. Ventilation by face mask was done till adequate depth of anesthesia and relaxation. Anesthesia was maintained by oxygen/nitrous oxide, sevoflurane mixture.
I-gel device () was carefully selected according to manufacturer recommendations. Patient weighing 50–90 kg, size 4 was used and patients weighing above 90 kg, size 5 was appropriate for them. Proper preparation, lubrication with water soluble lubricant was done. Senior anesthetist inserted the i-gel by continuous introduction into the mouth against hard palate till resistance felt as recommended by the manufacturer. Correct placement of the device was confirmed by observation of proper chest expansion, square shape of end tidal CO2 waveform and absence of audible leak sounds. In case the airway and ventilation were not established properly; gentle pushing, pulling, head extension, jaw thrust, or neck flexion manipulations were tried before considering failed attempt. Failed attempt was recorded when the device removed from the mouth. Three attempts were allowed before considering failed attempt. Device was then tapped over the chin and connected to anesthesia machine. Gastric tube is lubricated and inserted down the gastric drainage port.
In T-group the trachea of the participant was intubated with an appropriate size tracheal tube: size 8.5 was used for the male participants and size 7.5 was used for the female participants.
Fresh gas flow was adjusted at 3 l min−1. Leak pressure then measured by closing the expiratory valve and recording airway pressure (not allowed to be more than 40 cm H2O) at which equilibrium was achieved. Equilibrium point was identified by either: (1) plateau on pressure–time curve or digitally displayed pressure gauge. (2) Pressure at which audible gas was heard by auscultation of lateral aspect of thyroid cartilage. The patient was then ventilated by volume controlled ventilation with three tidal volumes (6, 8 and 10 ml kg−1), inspiratory to expiratory ratio 1:2 without positive end expiratory pressure. Respiratory rate was adjusted to maintain 35–45 mmHg EtCO2. Gastric distension was detected by auscultation of epigastrium or as noted by surgeon intra-operative. Inspiratory (ITV) and expiratory (ETV) tidal volumes were recorded and leak volume (LV) was calculated as the difference between both volumes (LV = ITV − ETV). The leak fraction was calculated as leak volume divided by ITV (i.e. leak fraction LV/ITV).
Ventilation was started by tidal volume 6 ml kg−1 for 3 min with data recording then the tidal volume increased to 8 and 10 ml kg−1 for the same period with same data recording. After pneumoperitoneum same ventilation and data collection was repeated. Ventilation was maintained at the parameters that achieve best oxygenation and ventilation. Goals were to maintain SpO2 > 95% and EtCO2 < 45 mmHg. Oxygenation was considered sub-optimal if SpO2 was 90–94% and failed if SpO2 < 90%. Suboptimal ventilation was considered when EtCO2 45–53 mmHg and failure if EtCO2 > 53 mmHg. Peak airway pressure was recorded pre- and post-pneumoperitoneum. If oxygenation or ventilation failed during procedure, surgeons were asked to hold and release of pneumoperitoneum then preoxygenation and endotracheal tube insertion.
The primary outcome of our study was difference in the leak fraction between two airway devices under investigation before and after pneumoperitoneum (B and A), with different tidal volumes. Secondary outcomes include: number of insertion attempts; presence of gastric insufflations; leak pressure; leak volume; and ventilatory variables. Also complications occurring during insertion, and removal were noted for each patient. Sore throat, coughing, gastric distension, regurgitation, aspiration, and dysphonia were evaluated after recovery.
The sample size was determined by considering a difference in the leak fraction of more than 20% for the i-gel when compared with the tracheal tube to be significant. Previous studies had used a difference of 20% and 25% in the leak fraction for power calculation according to their institute’s anesthetist concepts [Citation5]. Parametric data were analyzed by paired and unpaired t-tests. Non-parametric data were analyzed with the χ2-test. Data are mean (SD, range) or number of patients unless otherwise mentioned. A standard deviation value of (0.15) was used for the leak fraction from a previous study performed with conventional laryngeal mask airways (LMAs) [Citation1].
A two-sample study design, used a t-test for comparison of group means, would therefore require a total of 60 patients for 90% power at a significance level of 5%.
3 Results
Sixty patients were selected for the study; as regarding demographic data, there was no statistically significant difference between groups. The mean (SD) age, sex, weight, height and BMI of the participant are shown in . The median airway leak (sealing) pressure with i-gel was 25.75 (20–31.5) cm H2O.
Table 1 Demographic data (mean ± SD or n).
I-gel was inserted without failure in all cases within three attempts and four patients required manipulations.
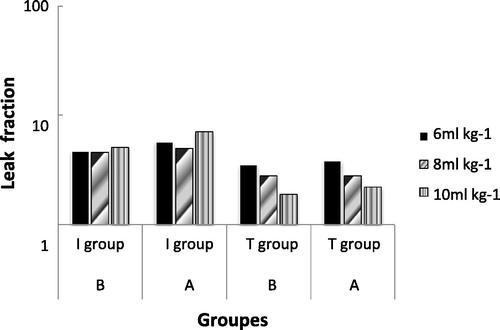
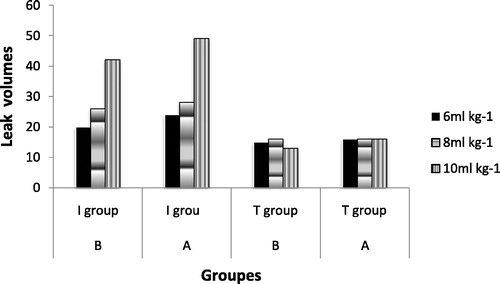
Before pneumoperitoneum there was no statistically significant difference in leak fraction () between i-gel (I group B) and tracheal tube (T group B) at tidal volume 6 and 8 ml kg−1 (P = 0.59 and 0.60), respectively. The mean difference in leak fraction was significant between (I group A) and (T group A) after pneumoperitoneum at 8 ml kg−1 tidal volume (P = 0.03). At 10 ml kg−1 there was statistically significant difference between i-gel and tracheal tube both before and after pneumoperitoneum (P = 0.002 and 0.006).
Leak volume at 6 and 8 ml kg−1 showed no significant difference before pneumoperitoneum but we found statistically significant difference after pneumoperitoneum at 8 ml kg−1 (P < 0.05). Median difference in leak volume () showed significance both before and after pneumoperitoneum at 10 ml kg−1. The median differences in leak volume at 10 ml kg−1 tidal volume were 28.5 and 33.5 ml before and after pneumoperitoneum, respectively. Four cases were found to have leak volumes of more than 200 ml at the three set tidal volumes. Their leak fractions were more than 20%.
At 6 ml kg−1 ventilation was optimum in all cases of both groups. Before pneumoperitoneum, ventilation was also optimum in all cases of both I and T groups at 8 ml kg−1. It was suboptimal in seven cases in I-group A, of which three cases ventilation failed and required tracheal intubation. The remaining four cases ventilation improved after increasing respiratory rate. At 10 ml kg−1 ventilation was sub-optimum in three and nine cases of I-group B and A, respectively. Five cases ventilation failed and required tracheal intubation of I-group A. Oxygenation was optimum in all cases.
None of our patients was positive for gastric distension by auscultation over epigastric area. The i-gel was inserted within three attempts without failure. Only four patients of I-group needed minor manipulations after insertion. None of the cases needed more than one manipulation. On removal, no visible blood was noticed. Two cases had a minor trauma to the lip. After recovery, there was no hoarseness, spasm or regurgitation ().
Table 2 Comparison of other parameters.
4 Discussion
Supra glottic airway devices have several advantages including lower incidence of sore throat [Citation6], less hemodynamic upset during induction and maintenance of anesthesia [Citation7,Citation8] and better oxygenation during emergence [Citation9]. I-gel is a relatively new disposable supraglottic airway device that has no inflatable cuff. It has an integral bite block, wide bore lumen, and an additional distal lumen that allows for the passage of a gastric tube. These features may give the i-gel an advantage over the LMA and even the ProSeal LMA.
In our study we found that i-gel airway can be used safely and effectively during volume controlled ventilation with low and moderate tidal volumes. There was too much debate between anesthesiologists about using these devices during procedures requiring positive pressure ventilation. During high tidal volume ventilation and laparoscopic procedures peak airway pressure rises and exceeds airway sealing (leak) pressure leading to increase in leak volume and fraction. These findings explain difficulties found to maintain optimum ventilation. Uppal et al. [Citation5] found leak pressure for i-gel 28 (20–35) cm H2O by both auscultation and manometer stabilization methods. In our study we concluded that airway leak pressure for i-gel was 25.75 cm H2O. Ishwar et al. [Citation10] concluded that airway leak pressure for i-gel was 25.27 cm H2O using same methods. Lopez-Gil et al. [Citation11] compared four kinds of measurements of the airway sealing pressure, which involved detection of audible noise by listening over the mouth, detection of exhaled carbon dioxide by placing a gas sampling line for the capnograph inside the mouth, detection of a steady value airway pressure while occluding the expiratory valve of the circle system and detection of an audible noise using a stethoscope placed just lateral to the thyroid cartilage. They concluded that all four tests were excellent.
We suspected from previous study, Uppal et al. [Citation5], that there may be some cases with laryngeal anatomical variation that may lead to high leak volumes and leak fraction. This leads to unequal distribution of data. Therefore data were analyzed using non-parametric tests. The four cases with high leak volume with all tested tidal volumes, were included in T group. In our study we wanted to evaluate the i-gel during procedures with higher pressure like laparoscopic procedures. Lu et al. [Citation12] compared ProSeal laryngeal mask airway (PLMA) with Classic laryngeal mask airway (LMA) for positive pressure ventilation during laparoscopic cholecystectomy. They concluded that PLMA is more effective ventilator device for laparoscopic cholecystectomy than classic LMA. This was attributed to higher leak pressure due to large cuff size (leak pressure was 29 ± 6 cm H2O). We thought that i-gel could be used during such procedures but unfortunately during our study we found leak pressure for i-gel was 25.75 cm H2O which is less than peak pressure during pneumoperitoneum especially at moderate and high tidal volumes [Citation13].
Donaldson and Michalek [Citation14] had inserted i-gel airway to control airway during laparoscopic cholecystectomy with volume controlled ventilation in patient with subglottic stenosis. They ventilated the patient with 500 ml tidal volume and a rate of 12 b min−1. The peak pressures were 14 and 18 cm Hg before and after pneumoperitoneum, respectively. We considered 10 ml kg−1 as a high tidal volume because more that 10 ml kg−1 are probably seldom used during anesthesia [Citation15].
We did not correlate anatomical position of i-gel with clinically evident leaks by using fibreoptic bronchoscope [Citation16]. No gastric distension, regurgitation, or aspiration while using the i-gel for VCV during our study. There were no cases of failed insertions. Visible blood was observed on the i-gel after removal, in our study, was 12% (4/30). This is similar to those reported with other SAD. The occurrence of visible blood with the use of other SAD has been reported from 12% to 18%, depending upon the type of SAD, technique of insertion, and ease of insertion [Citation17,Citation18].
Our study supports the use of i-gel during VCV in elective laparoscopic cholecystectomy using low to moderate tidal volumes provided that peak airway pressure not more than device leak pressure. Although leak volume was significant, ventilation and oxygenation were optimal in most cases. Tracheal tube should be inserted if failed ventilation and oxygenation.
Notes
Available online 18 February 2011
References
- J.H. Devitt R. Wenstone A.G. Noel M.P. O’Donnell The laryngeal mask airway and positive-pressure ventilation Anesthesiology 80 1994 550 555
- R.M. Levitan W.C. Kinkle Initial anatomic investigations of the i-gel™ airway: a novel supraglottic airway without inflatable cuff Anesthesia 60 2005 1022 1026
- K.M. Jackson T.M. Cook Evaluation of four airway training manikins as patient simulators for the insertion of eight types of supraglottic airway devices Anaesthesia 62 2007 388 393
- N.M. Wharton B. Gibbison D.A. Gabbott G.M. Haslam N. Muchatuta T.M. Cook i-gel insertion by novices in manikins and patients Anaesthesia 63 2008 991 995
- V. Uppal G. Fletcher J. Kinsella Comparison of the i-gel with the cuffed tracheal tube during pressure-controlled ventilation Br J Anaesth 102 2 2009 264 268 ISSN: 0007-0912
- P.P. Higgins F. Chung G. Mezei Postoperative sore throat after ambulatory surgery Br J Anaesth 88 2002 582 584
- R.A. Dyer R.L. Llewellyn M.F. James Total i.v. anaesthesia with propofol and the laryngeal mask for orthopaedic surgery Br J Anaesth 74 1995 123 128
- R.C. Cork R.M. Depa J.R. Standen Prospective comparison of use of the laryngeal mask and endotracheal tube for ambulatory surgery Anesth Analg 79 1994 719 727
- A.C. Webster P.K. Morley-Forster S. Dain Anaesthesia for adenotonsillectomy: a comparison between tracheal intubation and the armoured laryngeal mask airway Can J Anaesth 40 1993 1171 1177
- S. Ishwar G. Monika T. Mansi Comparison of clinical performance of i-gel™ with LMA–ProSeal™ in elective surgeries Indian J Anaesth 53 3 2009 302 305
- M. Lopez-Gil J. Brimacombe C. Keller A comparison of four methods for assessing oropharyngeal leak pressure with the laryngeal mask airway (LMA) in paediatric patients Paediatr Anaesth 11 2001 319 321
- P.P. Lu J. Brimacombe C. Yang M. Shyr ProSeal versus the Classic laryngeal mask airway for positive pressure ventilation during laparoscopic cholecystectomy Br J Anaesth 88 6 2002 824 827
- J. Brimacombe C. Keller B. Fullekrug A multicenter study comparing the ProSeal and Classic laryngeal mask airway in anesthetized, nonparalyzed patients Anesthesiology 96 2002 289 295
- W. Donaldson P. Michalek The use of an i-gel supraglottic airway for the airway management of a patient with subglottic stenosis, a case report Minerva Anesthesiol 76 2010
- M.J. Schultz J.J. Haitsma A.S. Slutsky O. Gajic What tidal volumes should be used in patients without acute lung injury? Anesthesiology 106 2007 1226 1231
- A. Van Zundert J. Brimacombe R. Kamphuis M. Haanschoten The anatomical position of three extraglottic airway devices in patients with clear airways Anaesthesia 61 2006 891 895
- M.R. Parker C.J. Day Visible and occult blood contamination of laryngeal mask airways and tracheal tubes used in adult anaesthesia Anaesthesia 55 2000 388 390
- S.G. Tordoff S. Scott Blood contamination of the laryngeal mask airways and laryngoscopes—what do we tell our patients? Anaesthesia 57 2002 505 506