 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Gastrectomy patients are commonly unable to maintain nutritional status. The aim of the current study was to examine the impact of a designed dietary protocol on postoperative outcome of cancer patients undergoing gastrectomy.
Methods
Sixty adult male and female cancer patients was included, and divided into two equal and matched groups (study & control). Four data collection tools were used: sociodemographic data sheet, postgastrectomy complications assessment sheet, nutritional assessment sheet and wound assessment sheet. The study group patients received specially tailored total parenteral nutrition (TPN) within a nutritional/dietary protocol focussing on six small dry daily feeding meals (low carbohydrate, moderate protein, low fat).
Results
The mean anthropometric measurements did not differ significantly from admission to the last follow up time (23.7 ± 4.5 & 22.2 ± 1.1 for Body Mass Index (BMI), 14.4 ± 6.2 & 13.06 ± 6.0 for Triceps Skin Fold (TSF) and 21.5 ± 3.0 & 20.6 ± 2.9 for Mid Arm Muscle Circumference (MAMC), respectively), as compared to that of the control group who showed statistically significant differences (22.5 ± 4.3 & 18.8 ± 3.4 for BMI, 10.8 ± 8.1 & 10.2 & 7.8 for TSF, and 20.4 ± 1.9 & 19.4± 1.8 for MAMC, respectively). The mean laboratory investigations as well did not differ significantly from admission to the last follow up time (11.3 ± 2.2 & 10.5 ± 1.1 for hemoglobin, 3.6 ± 0.5 & 3.7 ± 0.2 for serum albumin, 6.7 ± 0.7 & 6.4 ± 0.5 for serum total protein, 135.9 ± 4.0 & 137 ± 5.9 for serum sodium, and 3.7 ± 0.6 & 3. 5 ± 0.3 for serum potassium, respectively) as compared to that of the control group who showed statistically significant differences (11.1 ± 2.1 & 7.9 ± 2.5 for hemoglobin, 3.7 ± 0.6 & 2.9 ± 1.3 for serum albumin, 6.4 ± 0.5 & 4.9 ± 0.5 for serum total protein, 137.9 ± 3.9 & 133 ± 4.7 for serum sodium, and 3.8 ± 0.3 & 3.3 ± 0.2 for serum potassium, respectively). Dumping syndrome affected the control group subjects more frequently than the study group ones.
Conclusion
Specially tailored TPN within a nutritional/dietary protocol was associated with less prevalence of significant weight loss, malnutrition and dumping syndrome in cancer patients undergoing gastrectomy as compared to control group.
1 Introduction
Dumping syndrome is a set of unpleasant vasomotor gastro-intestinal symptoms that occur after meals as a direct result of surgical removal of all or part of the stomach and the pyloric sphincter or cutting the nerve that controls stomach contractions. These changes drastically reduce the reservoir capacity of the stomach [Citation1,Citation2]. It is experienced by approximately one-half of patients after stomach surgery for 1–6 months. Substantially patients suffered more from early than late dumping syndrome after gastrectomy. Two clinical factors, surgical procedures and amount of body weight loss, are considerably related to the occurrence of both early and late dumping syndrome [Citation3]. After surgery, the size of the stomach is much smaller. Eating a regular size meal, meals of hyperosmolar composition or a bolus of hypertonic fluids cause the food /fluid to be “dumped” too quickly in the small intestine acting like sponges, resulting in extra cellular fluids (ECF) shift or fluid drawing to dilute food decreasing plasma and blood volume with secondary distention of the bowel lumen which stimulates intestinal motility with the urge to defecate, this in addition to a very high rise in blood sugar [Citation3] and manifestations of early dumping such as cramping pain, bloating, borborygmi, explosive diarrhea, low blood pressure, dizziness, fainting, sweating, irregular or rapid heart beat, shortness of breath, feelings of weakness, nausea, and vomiting. The late phase (dumping) is attributed to reactive hypoglycemia following over production of insulin in response to rapid absorption of glucose with manifestations of profuse sweating, fatigue, anxiety, tremors, exhaustion, faintness, headache and nausea. These manifestations usually last for no longer than an hour after meals [Citation1]. Subtotal gastrectomy is now a feasible treatment for early gastric cancer with improved postoperative quality of life with no decrease in operative curability [Citation4]. Subtotal gastrectomy carries a lower incidence of late complications with most patients recovered from them within one year after surgery, although the occurrence of postprandial abdominal fullness was not uncommon [Citation5].
Treatment as stated by Rivera et al. [Citation2] is to never allow a large amount of food to enter the stomach, avoid foods that cause a high rise in blood sugar, take medications that keep the food longer in the stomach, e.g. anticholinergics to block the dumping syndrome reflex, pectin to reduce the severity of diarrhea, in addition to vitamin and mineral supplements to compensate for poor absorption.
Patient-specific tailored total parenteral nutrition (TPN) is a well established nutritional modality of delivering nutrients in an individualized mode according to each patient needs and medical condition in certain circumstances when caloric demand cannot be fulfilled or oral and enteral intake is not tolerated i.e. gastrointestinal intolerance to feeds [Citation6,Citation7].
Thereafter, dietary counseling is important to focus on having six small dry feedings daily that are low in carbohydrates, restricted in refined sugar; and contain moderate amount of protein and fat with fluid never taken with the meal but may be between meals. The patient should plan rest periods of at least 30 min after each meal. The recumbent position is the most beneficial if the patient can arrange for it [Citation3,Citation4].
Early dumping syndrome usually lasts 3–4 months, however, late dumping syndrome usually lasts one year, but it may persist for many years [Citation1].
The aim of the current study was to examine the impact of a designed dietary protocol with specially tailored TPN on post-operative outcome among cancer patients undergoing gastrectomy at Cairo University Hospitals as regards nutritional status, frequency of dumping syndrome symptoms and wound healing.
2 Patients and methods
A quasi-experimental research design (non-randomized clinical trial) was followed in this study. Quasi-experimental studies are conducted to examine the effect of specific interventions on patients’ outcome [Citation8].
A convenient sample of 60 hospitalized adult male and female cancer patients; 20–60 years old, operable i.e. having no metastasis and willing to participate in the study; undergoing total or subtotal gastrectomy were included in the current study and divided into two equal homogenous groups: study and control (30 subjects each), with the following matching criteria: age group, co-morbidity diseases, and type of surgery.
The study was conducted at the different surgical units of the National Cancer Institute, and the general surgical wards of El-Manial University Hospital. Four tools were utilized to collect data pertinent to the study. Two tools were designed, tested and piloted by the study team to examine their applicability, clarity, reliability, and feasibility for data collection. These tools are:
| (1) | Socio-demographic () and medical data sheet, | ||||
| (2) | Nutritional assessment sheet [Citation9] ( and ), | ||||
| (3) | Dumping syndrome assessment sheet ( and ), and | ||||
| (4) | Wound healing assessment sheet [Citation10] (). | ||||
Table 1 Frequency distribution of the two studied groups as regards socio-demographic characteristics (n = 30 in each group) expressed as number of patients in each group.
Table 2 Comparison between the two studied groups as regards anthropometric measurements throughout the assessment periods (n = 30 in each group).
Table 3 Comparison between the two studied groups as regards laboratory investigations (n = 30 in each group).
Table 4 Comparison between the studied groups as regards dumping syndrome symptoms (n = 30 in each group) expressed as number of patients in each group.
Table 5 Timing of dumping syndrome symptoms among the two studied groups (n = 30 in each group) expressed as number of patients in each group.
Table 6 Comparison between the study and control group subjects as regards wound assessment, on the fifth post-operative day and before discharge (n = 30 in each group).
Nutritional assessment sheet and wound healing assessment sheet were adopted, modified, then piloted by the study team. Percent of weight change was defined as percent of weight change each assessment relative to the previous assessment and on admission weight change was calculated relative to 6 months ago according to history taking which was performed. Significant (rapid) rate of weight loss was defined as weight loss greater than 2% per week, 5% per month, 7.5% per 3 months, or 10% per 6 months. Patient was categorized as at actual risk of Malnutrition if he had any of:
| (1) | Marked over weight (20% > Ideal body weight). | ||||
| (2) | Marked under weight (20% < Ideal body weight). | ||||
| (3) | Unintentional weight loss (10% of usual body weight). | ||||
| (4) | Presence of three or more risk factors affecting nutritional status which are recent unintentional weight loss or gain, appetite change, taste alteration, difficulty in chewing or swallowing, recent surgery/or sepsis/trauma, GIT disturbances such as diarrhea, and constipation, food allergy, multiple medications, decreased income, immobility and social isolation. | ||||
| (5) | Serum albumin ⩽3.5 g/dl. | ||||
An official permission to conduct the study was obtained from the Vice Dean for Higher Education and Research, the Head of the general surgical wards of the National Cancer Institute, the Director of El Manial University Hospital, and Directors of general surgical units. In addition, patients’ agreements to be included in the study were obtained.
A designed dietary protocol in the first, second, and third post operative weeks was given to the hospitals dietitians and nurses enrolled in the study team to implement it on the study group. It comprised of six small dry feedings daily that are low in carbohydrates, restricted in refined sugar; and contain moderate amount of protein and fat with fluid never taken with the meal but may be between meals . The patient should plan rest periods of at least 30 min after each meal. The recumbent position is the most beneficial if the patient can arrange for it. Nurses also explained to the patients how to feed after discharge from the hospital.
A pilot study was carried out on six patients who undergone total and subtotal gastrectomy who fulfilled the inclusion criteria from different surgical units of the National Cancer Institute and El-Manial University Hospital Cairo University to test clarity, reliability, and feasibility of data collection tools.
Based on the results of the pilot study, needed refinement or modifications were done in the data collection tools.
Post-operatively, both the study and control group subjects were exposed to the traditional intensive care unit (ICU) care. During their presence in the ICU, the study group patients received TPN through an inserted CVP. Monitoring the received volume of TPN was done guided by CVP measurement, vital signs, and urine output. TPN was designed on an individual basis (tailored), according to age, nutritional assessment data, and other associated diseases such as liver, or renal diseases and diabetes. Preparation of TPN was done utilizing the hospital resources of intravenous fluids such as aminosteril KE 10% or nephrosteril 7% (in renal patients) or aminosteril N-hepa 8% (in hepatic patients), intralipid 20%, trace elements (addamel), Fat soluble vitamins (vitalipid) and water soluble vitamins (soluvit) which are all products of Fresenius Kabi, Uppsala, Sweden as well as dextrose 25% and electrolytes. 2500 ml of TPN all-in-one admixture were administered daily, for each 70 Kg of body weight, to each patient in the study group. Each 1000 ml of the TPN formula, delivering 925 Kcal, consisted of 444 ml of dextrose 25%, 185 ml of intralipid 20%, 370 ml of aminosteril KE 10% or nephrosteril 7% or aminosteril N-hepa 8%, with the following eletrolytes (32 mmol Na+, 15 mmol K+, 2 mmol , 2 mmoll Mg+, 47 mmol Cl−, 2 mmol
). In addition, one vial of addamel, one vial of soluvit and one vial of vitalipid, which are all products of Fresenius Kabi, Uppsala, Sweden, were added to the whole daily volume of TPN for each patient. TPN was prepared under the laminar flow of the clinical pharmacy at the National Cancer Institute respecting admixing ranges and stability standards. TPN was administered using continuous intravenous method of administration using IV blood transfusion sets (over 18 h). Blood glucose level was monitored every 4 h, vital signs and urine output were monitored at least every 8 h. Laboratory investigations for serum electrolytes and albumin were performed every 24 h. Both the study and control groups parenteral bags were prepared and delivered from the hospitals admixing unit.
Total parenteral nutrition was administered starting from the first post-operative day and for 4 days postoperatively, then the physicians were contacted to check if patients were going to start oral fluids or not. Patients were informed regarding dumping syndrome manifestations, how to prevent their occurrence and how to handle them if happened. The assessors of the results where blinded as to which group each patient was enrolled. The ICU resident, not involved in the research, ordered fluids to the control patients which were prepared in covered bags in the hospitals admixing unit under laminar flow similar to the covered TPN bags of the study group. Both groups were encouraged to eat once the surgeon allows them to.
As regards the control group subjects, the same previously mentioned actions were done for them except for provision of dietary protocol regimen and specially tailored TPN. However, for ethical reasons, patients in the control group who had problems associated with eating and did not know what to eat were answered for any questions. There was a continuous contact with patients and their care givers, through phone calls to monitor their conditions at home on regular basis.
Each patient either in the study or the control group was assessed on admission, during hospitalization (at the end of the fourth day) and one, two, and three months after discharge (Follow up I–III respectively) utilizing the four study tools. Laboratory data were obtained on admission, during hospitalization (6 h after end of : the TPN, in study group, or the parenteral fluid bags, in the control group, of fourth postoperative day) and one, two, and three months after discharge (Follow up I–III, respectively). Wound healing assessment was done on the fifth postoperative day and before discharge. Wound description (length, width depth and for how long it is present) was also investigated. Both the study and control group subjects were exposed to the routine hospital care.
The sample size calculations were performed using the nQuery Advisor software package (version 4.0; Statistical Solutions, Boston, MA). A power analysis indicated that a minimum sample size of 40 patients randomly assigned to the treatment groups would provide 80% power for detecting a significant difference between the groups.
Data of the current study were verified prior to computerized entry. The Statistical Package for Social Sciences (SPSS version. 11) was used for that purpose followed by data analysis and tabulation. Descriptive statistics were applied (e.g. mean, standard deviation, frequency, percentage). Tests of significance were performed to test the study results (i.e. paired and unpaired t-test, and chi square test). Pearson's correlation coefficient was applied between quantitative variables. A significant level value was considered when p < 0.05.
3 Results
describes the study and control group subjects as regards their socio-demographic characteristics. No statistically significant differences were evidenced between the study and control groups in relation to their socio-demographic variables. As regards the patients medical condition, the majority of both groups (86.7%) were free from chronic diseases. Approximately two thirds (70%) of both the study and control group subjects had undergone partial gastrectomy, while less than one third (30%) undergone total gastrectomy. No statistically significant difference was found between the two groups as regards the type of surgery. The mean total length of hospital stay among the control group was 20.1 ± 8.1 as compared to 17.6 ± 6.2 of the study group with no evident significant difference.
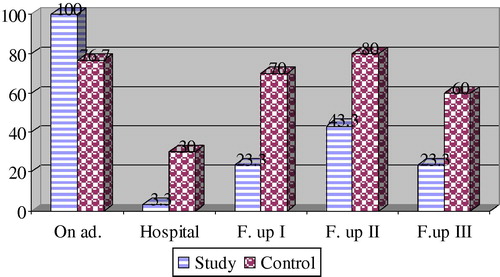
shows comparison between the two studied groups as regards anthropometric measurements. shows comparison between the study and control group subjects as regards rate of weight loss. It clarifies that the whole study group and slightly more than three quarters of the control group subjects (100% & 76.7%, respectively), had a significant weight loss (rapid weight loss) on admission. During hospitalization weight loss affected both groups, but was only significant among approximately one third (30%) of the control group, and a minority (3.3%) of the study group, indicating a statistically significant difference between the two groups (χ2 = 7.68, at p ⩽ 0.01). During the three follow up assessment periods weight loss significantly affected the control group more than the study group (70% & 23.3%, 80% & 43.3%, and 60% & 23.3%, respectively). Chi square test showed statistically significant differences between the two groups as follows (13.12, 8.52 & 10), at p ⩽ 0.01.
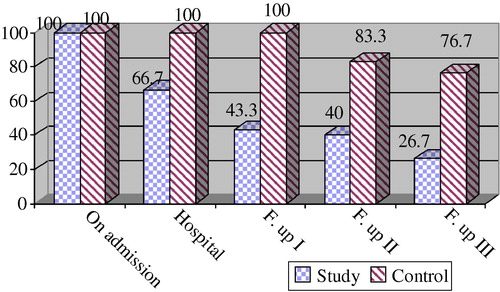
shows comparison between the study and control group subjects as regards laboratory investigations. shows that, both the study and control group subjects (100%) were admitted with a risk of malnutrition (malnourished). This proportion reduced gradually during different assessment periods among the study group subjects (66.7%, 43.3%, 40% & 26.7%, respectively), as compared to the control group ones (100%, 100%, 83.3%, & 76.7%, respectively), who remained at risk of malnutrition. Chi square test showed statistically significant differences between the two groups during different assessment periods (χ2 = 12, 23.8, 12 & 15.02, respectively) at p values ⩽0.001.
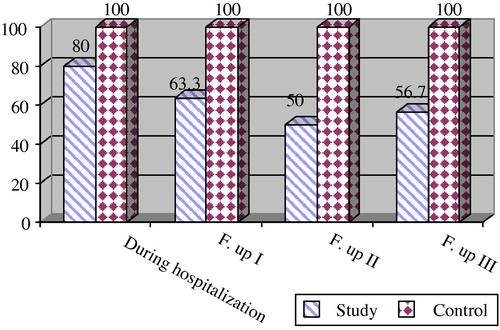
shows frequency of dumping syndrome among the studied group subjects. It indicates that dumping syndrome was experienced by the control group subjects most frequently than the study group ones all over the different assessment periods (100 & 80%, 100% & 63.3%, 100% & 50%, and 100% & 56.7%, respectively). No statistically significant differences were found between the two groups during hospitalization (χ2 = 0.68). However, highly statistically significant differences were found between the two studied groups in the follow up assessment periods (13.46, 20, & 16.59 respectively, at p ⩽ 0.001). shows dumping syndrome symptoms experienced by the studied groups subjects. As regards timing of the experienced dumping syndrome symptoms, shows the experienced symptoms during hospitalization and in the different follow up assessment periods.
displays a comparison between the two studied groups as regards wound assessment in the fifth postoperative day and before discharge as regards wound status before discharge. It clarifies that approximately two thirds of the study and control group subjects needed up to two weeks for sutures to be removed (66.6% & 70%, respectively). A tendency to delayed wound healing was noticed among the control group subjects more than the study group ones (40% & 23.3%, respectively). However, no statistically significant differences were found between the two groups in this regard.
No correlations were found between age and anthropometric measurements among the study group subjects all over the different assessment periods. However, only a positive correlation was found between age and mid arm muscle circumference among the control group subjects on admission, during hospitalization, and in the second and third follow up assessments as follows (r = 0.45, 0.425, 0.431 & 0.532, respectively at p ⩽ 0.01), indicating that the greater the age, the more the muscle loss ().
Table 7 Studied groups’ anthropometric measurements in relation to age all through the assessment periods (n = 30 in each group).
On admission, all the study group subjects’ males and females (100%), the majority of the control group males (81%), and two thirds of the females (66.7%) had a significant weight loss. During hospitalization minorities of the study group males (18.75%) and females (7.1%), had significant weight loss, as compared to the control group males (33.3%) and females (22.2%). In the different follow up assessment periods, stability in body weight was noticed among most of the study group males and females (81.25%, 43.3%, & 31%, and 78.6%, 42.8% & 35.7%, respectively), as compared to the control group females and males (76.2%, 76.2% & 90.5% and 55.5%, 77.8% & 77.8%, respectively), whose body weight changed significantly. However, no statistically significant differences were found regarding the significance of weight loss in relation to gender.
Regarding laboratory data changes, reveals that only serum cholesterol level was found to be positively correlated with age only among the study group subjects in different assessment times. The proportion of patients with mild to moderate hypo-albuminemia did not differ significantly in relation to gender among both the study and control groups subjects. However, a statistically significant difference was found between males and females of the control group subjects during the second follow up assessment (χ2 = 5.5 at p ⩽ 0.05) (). No correlations were between laboratory investigations and hospital stay among the study group subjects. Only serum albumin and serum cholesterol levels were found to be negatively correlated with hospital stay among the control group subjects (r = −0.396 at p ⩽ 0.05 & r = −0.553 at ⩽0.001, respectively) ().
Table 8 Correlation between the studied groups’ laboratory investigations and age (n = 30 in each group).
Table 9 Studied groups’ serum albumin level in relation to gender (n = 60).
Table 10 Correlations between the studied groups’ laboratory investigations and hospital stay (n = 30 in each group).
During hospitalization, no statistically significant difference was found between the type of surgery (total or partial gastrectomy) and dumping syndrome symptoms among the study group subjects. However, a significant statistical difference was found among the control group subjects. In the first follow up assessment, a statistically significant difference (at p ⩽ 0.001) was found among the study group subjects, indicating that all subjects with total gastrectomy (100%) and half of those with partial gastrectomy (50%) suffered from different dumping syndrome symptoms. However, no statistically significant difference was found among the control group subjects in this respect. In the second and third follow up assessments, no statistically significant differences were found between those with total or partial gastrectomy among both groups ().
Table 11 Dumping syndrome symptoms in relation to the type of surgery expressed as number of patients in each group (n = 30 in each group).
4 Discussion
The current study findings showed that, males represented the major segment of both the study and control groups, with a proportion of 1:0.62. In this regards, Ergor [Citation11] revealed that there is a male predominance in cancer incidence world wide, with a ratio of two males: one female.
Specially tailored TPN within a nutritional/dietary protocol comprising six small dry feedings daily that are low in carbohydrates, and contain moderate amount of protein and fat was associated with less prevalence of significant weight loss, malnutrition and dumping syndrome in cancer patients undergoing gastrectomy as compared to the control group.
Significant (rapid) rate of weight loss is weight loss greater than 2% per week, 5% per month, 7.5% per 3 months, or 10% per 6 months. Patient is categorized as at actual risk of malnutrition if he had any of : marked over weight (20% > Ideal body weight), marked under weight (20% < Ideal body weight), unintentional weight loss (10% of usual body weight), serum albumin ⩽3.5 g/dl or presence of three or more risk factors affecting nutritional status which are recent unintentional weight loss or gain, appetite change, taste alteration, difficulty in chewing or swallowing, recent surgery/or sepsis/trauma, GIT disturbances such as diarrhea, and constipation, food allergy, multiple medications, decreased income, immobility and social isolation. The incidence of emaciation and dumping syndrome was revealed to be lower in patients who undergone functional jejunal interposition [Citation12]. The results also delineated that, malnutrition was a significant problem among both groups on admission. During the first, second, and third follow up assessments, approximately one third of the study group subjects remained in the category of being malnourished as compared to the great majority of the control group subjects. Similarly, Lutz and Przytulski [Citation13], and Williams and Botti, [Citation14] clarified that malnutrition occurs due to different circumstances such as, the stress of trauma or surgery. They added that it occurs in institutional settings where care givers fail to provide adequate nourishment, to monitor patients’ food intake, and to make sure that they have help in eating. This is also in agreement with what described by Pertkiewicz [Citation15].
In the current study, the percentage of weight loss experienced by the control group subjects was greater as compared to that of the study group ones. They had higher percentage of weight change, and mean difference in their body weight which approximately doubled that of the study group subjects, indicating a statistically significant difference between the two studied groups. Therefore, an individual who has undergone a major surgery, including subtotal gastrectomy [Citation5] requires using a five day rule. If feeding has not resumed after five days, nutritional support should begin. If significant malnutrition is present on admission, seven days of specifically tailored nutritional repletion should be strongly considered prior to surgery, and restarted in the early post-operative period.
Considering laboratory investigations in the present study, the TPN group (the study group) showed significant improvement in their laboratory data results as compared to the control group ones. However, they showed in common prevalence of mild to moderate degree of anemia, hypoalbuminemia, and altered serum electrolyte levels during certain periods of assessment for the study group, and all through assessment periods for the control group subjects, indicating statistically significant differences between the two groups in this respect. Serum albumin level was negatively correlated to length of hospital stay among the control group subjects. Hypoalbuminemia was reported by Mathus-Vliegen [Citation16] to be correlated with severity of illness rather than the degree of malnutrition.
The current study showed decline in GIT complications, caused by dumping syndrome among the study group subjects as compared to the control group ones, indicating a statistically significant difference between both groups. The experienced GIT symptoms were that of early and late dumping, with greater frequency among the control group subjects than the study group ones, indicating statistically significant differences. In the present study the designed dietary protocol with knowledge provision was expected to decrease frequency of dumping syndrome symptoms. However, this did not seem to affect the frequency of dumping symptoms among those who suffered in the study group. The noticed benefit was decreased severity of their experienced symptoms as compared to the control group subjects, who showed greater frequency and severity. In a study to investigate the incidence of dumping syndrome after partial or total gastric resection and its relation with patient's preoperative nutritional status as well as the clinical behavior with dietary management during a short-term follow-up period, it was revealed that, the incidence of dumping syndrome was 45%. Patient's preoperative nutritional status affected the presence of clinical symptoms. Adequate dietary management reduced dumping manifestations in 53% of the patients during a short-term follow-up period [Citation17]. This comes in agreement with the current study results. In another study where results with distal gastric resections were analyzed, rate of dumping-syndrome was 12.3%. Original surgical methods for improvement of early and delayed functional results have been developing and applied in the clinical practice [Citation18].
The current study denoted that subjects in the study and control groups had moderate to extensive degree of wound inflammation, and purulent discharge accounting for one third of the study group as compared to more than one half of the control group, indicating a statistically significant difference, and delayed wound healing, with greater frequency among the control group subjects.
The current study demonstrated finding of many nutritional problems such as anemia, hypoalbuminemia, and hypoproteinemia. These problems can be held responsible about predisposing to wound infection [Citation19]. However, the noticed stability in the study group's nutritional status did not correct the level of hemoglobin to be up to the normal value. That is why its effect was not proved to be statistically different between the both groups in relation to wound healing in the current study. Therefore, one can deduce that the effect of nutritional problem is not the sole one affecting wound healing [Citation19] especially, where the hypothesis which suggest that the group who will receive nutritional support have better wound healing was not supported. Therefore, other factors unrelated to nutrition may affect wound healing. These factors may be the type of surgery, surgeon's technique and length of hospital stay. Preoperative shaving increases the risk of infection due to multiplication of bacteria in microabrasions caused by the razor on the surface of the skin [Citation19]. Nevertheless, inspite of denoting no direct cause-effect relationship between nutritional status and occurrence of wound infection, preoperative as well as postoperative nutritional support are needed to restore nutrient loss after surgery [Citation16,Citation20]. These findings could rationalize what was noticed in the current study, where the study subjects received TPN only post operatively and for a period not exceeding several days. So, the effect on postoperative wound healing did not prove to be a significant one.
Some limitations were present in the present study; the findings of the current study cannot be generalized because of the small sample size and the control group which was examined regarding the routinely provided information from the hospital staff. It is also recommended to perform further studies to investigate the effect of preoperative nutritional support on patients’ nutritional status and to compare between different nutritional protocols in relation to their effects on wound healing and between total and subtotal gastrectomy patients as regards frequency of dumping syndrome with nutritional interventions.
The present study supports the important role of the intensivist in the area of patients nutrition through assessing nutritional status, calculating individualized caloric requirements and teaching patients about the required diet and how to prevent, as well as handle, the experienced dietary problems. It might also generate an attention and motivation for further researches in this area. Based upon findings of the present study, one can conclude that, nutritional care using a designed (tailored) TPN regimen, as well as dietary instructions (dietary counseling), tended to improve nutritional status and reduce frequency and symptoms of dumping syndrome. However, wound healing was not found to be affected by the nutritional intervention in the current study.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- V.P.AkimovL.G.DvaladzeT.D.ShengeliaI.u.E.VeselovA new view on pathogenesis of dumping-syndromeVestn Khir Im I I Grek167620082225 [Russian]
- I.RiveraC.I.Ochoa-MartinezJ.M.Hermosillo-SandovalDumping syndrome in patients submitted to gastric resectionCir Cir.7562007429434 [Spanish]
- S.MineT.SanoK.TsutsumiY.MurakamiK.EharaM.SakaK.HaraT.FukagawaH.UdagawaH.KataiLarge-scale investigation into dumping syndrome after gastrectomy for gastric cancerJ Am Coll Surg21152010628636
- K.IshikawaT.AritaS.NinomiyaT.BandohN.ShiraishiS.KitanoOutcome of segmental gastrectomy versus distal gastrectomy for early gastric cancerWorld J Surg3111200722042207 Epub 2007, Aug 24
- C.PedrazzaniD.MarrelliB.RamponeA.De StefanoG.CorsoG.FotiaE.PintoF.RovielloPostoperative complications and functional results after subtotal gastrectomy with Billroth II reconstruction for primary gastric cancerDig Dis Sci528200717571763
- ASPEN Board of Directors, Clinical Guidelines Task Force. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enteral Nutr 2002;26:Suppl:1SA-138SA[Erratum, JPEN J Parenter Enteral Nutr 2002;26:144].
- P.SingerM.M.BergerG.Van den BergheESPEN guidelines on parenteral nutrition: intensive careClin Nutr282009387400
- G.LoBiondoJ.HaberNursing Research, Methods, Critical Appraisal, and Utilization5th ed.2002Mosby Co.USAp.211
- C.JarvisPhysical examination and health assessment1996WB Saunders Co.Philadelphiap.126–51
- M.FlanaganAccess to clinical education: wound management1997Churchill living stone Co.Singaporep.43–5
- Ergor G. Stomach Cancer. In: Freedman LS, Edwards BK, Reis LAG, Young JL, editors. Cancer incidence in four member countries, 2006, p. 1–167.
- Y.B.ChenY.F.LiX.Y.FengZ.W.ZhouY.Q.ZhanW.LiComparison of two types of digestive tract reconstruction after total gastrectomy in patients with gastric carcinomaZhonghua Zhong Liu Za Zhi3322011126129
- C.A.LutzK.R.PrzytulskiNutrition and diet therapy3rd ed.2001F.A. Davis Co.Philadelphiap.319–22
- S.A.WilliamsL.BottiIssues concerning the ongoing care of patients with comorbidities in acute care and post discharge in Australia: a literature reviewJ Adv Nur3172002131140
- M.PertkiewiczPrevalence and consequences of malnutrition on admission to hospital in Poland, the multicenter studyClin Nutr21120029196
- E.M.Mathus-VliegenNutritional status, nutrition and pressure ulcerNutr Clin Pract1632001286291
- I.RiveraC.I.Ochoa-Martı´nezJ.M.Hermosillo-SandovalJ.M.Morales-AmezcuaC.Fuentes-OrozcoA.González-OjedaDumping syndrome in patients submitted to gastric resectionCirCir7562007429434
- TShMorgoshiiaBilroth-I subtotal resection and its efficacy in the treatment of distal gastric cancerKhirurgiia (Mosk)720061030
- K.ManleyL.BellmanSurgical nursing: advancing practice2000Churchill Livingstone Co.Londonp.605–36
- C.W.ThompsonNutrition and immune function, APIC text of infection control and epidemiologyMosby20022735