Abstract
Objectives
To evaluate the predictability of intracranial pressure (ICP), cerebral perfusion pressure (CPP) and hemodynamic monitoring for outcome of children with severe traumatic brain injury (TBI).
Patients and methods
The study included 53 children with severe TBI. All the patients were immediately admitted to Neurosurgical Intensive Care Unit (NICU) for determination of baseline data and to receive first aid management and assessment of head injury severity according to post-resuscitation Glasgow coma scale (GCS) and patients were enrolled if they had GCS of ⩽8. All the patients had insertion of the intraventicular ICP sensor either at the end of surgery if indicated or through Kocher's pathway and were maintained for a maximum of 5 days. All the patients had non-invasive monitoring for heart rate (HR), blood pressure measures and CPP. Glasgow outcome scale (GOS) was determined at discharge time and 6 months thereafter.
Results
Thirty-seven patients continued their ICU stay and were discharged alive for a survival rate of 75.8% and 28 of survivors (75.7%) had favorable outcome. Hemodynamic parameters estimated at the time of catheter removal showed significant changes in survivors compared to their levels estimated at the time of catheter insertion and to non-survivors. Patients having favorable outcome showed more stable hemodynamic changes, while those who had unfavorable outcome showed autonomic instability manifested as significantly lower SBP, DBP and MAP with non-significantly lower ICP and CPP. Statistical analysis defined CPP as the highly significant predictor of outcome with CPP as the significant predictor for survival and favorable outcome. Analysis of the variability of estimated hemodynamic parameters, as predictors for survival defined disturbed ICP as the significant sensitive predictor and disturbed SBP as a significant predictor.
Conclusion
Hemodynamic stability for children had TBI mandatory for improvement of their outcome with high and low CPP with concomitant large range of SBP variability which could be considered as predictors for bad outcome.
1 Introduction
Secondary brain insult of traumatic brain injured patients is a challenging problem best managed through early prediction and prevention rather than treatment. Secondary brain damage is a major factor in determining patient outcome following traumatic brain injury. Cerebral hypoxia caused by cerebral ischemia—through impaired autoregulation, systemic hypotension, hypoxia, and intracranial hypertension—has been identified as a principal cause of secondary brain damage. In addition, blood pressure and cerebral perfusion pressure (CPP) are kept at higher levels than normal in order to provide sufficient cerebral blood flow and avoid cerebral ischemia in the presence of impaired autoregulation. However, despite maintaining a CPP of >70 mmHg, cerebral ischemia and hypoxia may still occur, worsening the patient's chances of a satisfactory outcome [Citation1–Citation3].
The brain is enclosed in a rigid cage of bone and that the volume of its contents must remain constant if intracranial pressure (ICP) is to remain constant. An increase in the volume of one of the components of the intracranial cavity (e.g., brain) requires a compensatory reduction in another (e.g., CSF) to maintain a constant pressure. Brain tissue is essentially incompressible, so any increase in ICP due to brain swelling initially results in extrusion of CSF and (mainly venous) blood from the intracranial cavity, a phenomenon known as “spatial compensation”. CSF plays the largest role in spatial compensation because it can be expelled from the intracranial cavity into the “reservoir” of the spinal theca [Citation4,Citation5].
A number of studies have shown that high ICP is strongly associated with poor outcome, particularly if the period of intracranial hypertension is prolonged. Increased ICP can also cause actual shift of brain substance resulting in structural damage to the brain and to herniation through the tentorial hiatus or foramen magnum. The latter results in pressure on the brainstem causing bradycardia and hypertension (the classic Cushing reflex) and, if untreated, respiratory depression and death [Citation6–Citation8].
The present study aimed to evaluate the predictability of ICP, CPP and hemodynamic monitoring for outcome of children with severe traumatic head injury.
2 Patients and methods
The present study was conducted at Neurosurgical Intensive Care Unit (NICU), Kasr Al-Eini University Hospital since January 2009 till 2010 so as to allow at least 6-months follow-up for the last enrolled case. All severe traumatic head injury patients younger than 14 years were enrolled in the study, after obtaining parents’ fully informed written consent.
All the patients were immediately admitted to NICU for determination of baseline data and to receive first aid management. The severity of head injury was categorized according to post-resuscitation Glasgow coma scale and patients were enrolled if they had GCS of ⩽8 [Citation9]. General management included intubation, ventilation, oxygenation, head elevation, fluid resuscitation with normal saline with fluid restriction up to 75% of physiological fluid requirement afterwards, sedation, analgesia, muscle relaxation, normoventilation, and normothermia. Vasoactive agents (dopamine and norepinephrine) were used if needed in order to maintain optimal mean arterial pressure that was determined by continuous non-invasive monitoring. Throughout the patients’ stay at the ICU Pao2, Paco2, pH, and serum sodium levels were recorded three times daily at ICU lab and body temperature every 6 h and ICP was monitored 8-h.
After general condition stabilization, all the patients underwent radiological workup for evaluation of the extent of skull and brain injuries and patients had definite intracranial pathology necessitating surgical interference with the insertion of the intraventicular ICP sensor (Codman Microsensor™, ICP Transducer, Codman & Shurtleff, Raynham, MA) at the end of the surgery. Patients free of definite intracranial pathology had intraventricular ICP sensor insertion through Kocher's pathway at the right frontal lobe. All the patients were maintained under the umbrella of broad spectrum antibiotics. Catheters were removed on occurrence of hemorrhage during application or development of complications as infection, obstruction; otherwise the catheters were maintained for a maximum of 5 days.
All the patients had non-invasive monitoring for heart rate (HR), systolic and diastolic blood pressures and calculation of both mean arterial pressure (MAP) and pulse pressure (PP). Both ICP and CPP were monitored throughout the patients’ stay at the ICU with the designed levels assigned to be consistent with guidelines for the acute medical management of severe traumatic brain injury in children [Citation10], raised ICP was defined as a level higher than 20 mmHg throughout ICU stay and CPP was defined as CPP = MAP − ICP and minimal CPP was considered to be at a level of 40 mmHg.
Raised ICP management included mannitol, hypertonic saline (maintaining serum sodium level ⩾140 mmol/l), mild hyperventilation and barbiturates and decompressive craniotomy for refractory intracranial hypertension. In resistant cases, about 3–5 cc of CSF were withdrawn through the catheter.
2.1 Evaluated parameters and outcome
The mean hemodynamic variables estimated at the time of catheter insertion and removal and variability between both measurements was calculated and the mean ICP and CPP levels were evaluated for the prediction of outcome defined as favorable or unfavorable. Glasgow outcome scale (GOS) was determined at the time of discharge from hospital and 6 months thereafter using the Jennett five-point GOS classification: GOS 1¼ dead; GOS 2¼ vegetative state; GOS 3¼ alive but functionally impaired; GOS 4¼ minimal handicap; and GOS 5¼ pre-morbid level of functioning. A GOS of <4 reflected poor outcome, whereas good outcome was defined as a GOS of 4 or 5. Patients were divided into groups of “favorable” and “unfavorable” outcome. Patients with moderate disability and good recovery were regarded as having “favorable” outcome, while severe disability, vegetative survival, or deaths were considered to be an “unfavorable” outcome [Citation11].
2.2 Statistical analysis
Obtained data were presented as mean ± SD, ranges, numbers and ratios. Results were analyzed using paired t-test for inter-group comparisons and Wilcoxon signed ranks test for unrelated data for comparisons between groups of patients categorized according to survival and receiver operating characteristic (ROC) curve analysis, judged by area under curve (AUC), was used for evaluation of the predictability of mean measured hemodynamic parameters and ICP as predictors for outcome with AUC was compared versus the null hypothesis that AUC = 0.5. Multiple regression analysis was used for verification of predictors for outcome using stepwise method. Hemodynamic variability was calculated as measurements at the time of catheter removal minus those at the time of catheter insertion divided by the latter and presented as percentage of change. Statistical analysis was conducted using the SPSS (Version 10, 2002) for Windows statistical package. P value <0.05 was considered statistically significant.
3 Results
Through the study period 53 children with severe traumatic brain injury (TBI) were admitted to NICU; however, two children died immediately on arrival at the hospital and were excluded of the study. The patients’ characteristics and admission data were shown in .
Table 1 At admission baseline data of studied children.
Twenty-five patients (49%) required surgical interference for hematoma evacuation and intraoperative catheter application was conducted at the end of the surgery, while in the other 26 patients (51%) catheter was applied through Kocher's pathway. Bleeding during catheter insertion was encountered in three patients (5.9%) and the catheter was removed immediately and these three patients were excluded of the study. Catheter-related infection was the only complication that occurred during the patients’ stay at the ICU and was encountered in five patients (9.8%) and catheter was removed on the third day in two patients and on the fourth day in three patients and these five patients were excluded from the study. The catheter was maintained till the fifth day without complications in 43 patients (84.3%). Seven patients (13.7%) had ICP resistant to decrease and about 5 ml of CSF was withdrawn through the catheter and so considered as therapeutic modality in addition to monitoring of these seven patients.
Throughout NICU stay 37 patients continued their ICU stay and were discharged alive for a survival rate of 75.8%. At the time of their discharge, 28 of the survivors (75.7%) had favorable outcome; 24 patients (64.9%) had good recovery and four patients (10.8%) had moderate disability, while six patients (16.4%) had severe disability and three patients (8.1%) had vegetative survival. At 6-months follow-up, three patients at discharge with unfavorable outcome showed improved disability to be moderate and increased favorable outcome rate among survivors was 83.8%, ().
Table 2 Patients’ distribution according to outcome throughout the study period.
Hemodynamic parameters estimated at the time of catheter removal showed significant changes in survivors compared to their levels estimated at the time of catheter insertion with significantly higher PP and CPP and significantly lower ICP. Also, mean DBP, MAP and CPP were significantly higher and mean ICP levels were significantly lower in survivors compared to non-survivors with non-significantly higher SBP and lower PP. Moreover, survivors showed more hemodynamic stability compared to non-survivors and a significantly lower percentage of change of SBP, DBP manifested with significantly higher percentage of change of DBP and ICP when compared to non-survivors, ().
Table 3 Mean levels of hemodynamic parameters estimated at time of catheter insertion and removal in studied patients categorized according to outcome.
Among survivors, patients who had favorable outcome showed more stable hemodynamic changes manifested as non-significant difference between measures recorded at the time of catheter removal compared to that at the time of catheter insertion, apart from significantly lower ICP and non-significantly higher CPP. On the contrary, patients who had unfavorable outcome showed autonomic instability manifested as significantly lower SBP, DBP and MAP with non-significantly lower ICP and CPP. Moreover, the percentages of changes were significantly lower in patients who had favorable outcome compared to those who had unfavorable outcome, ().
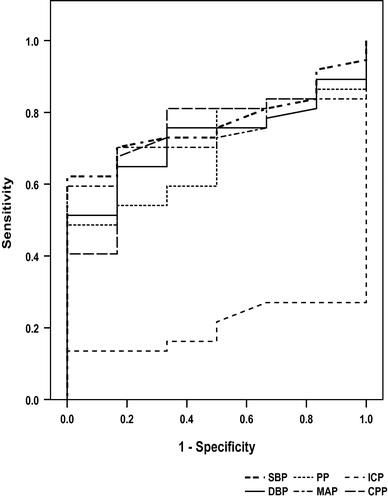
Analysis of estimated hemodynamic parameters, at the time of catheter removal, as predictors for survival and favorable outcome using ROC analysis comparing the resultant area under curve (AUC) versus the null hypothesis that AUC = 0.5, defined CPP as the highly significant predictor of both modes of outcome, despite the significance of other parameters. Using regression analysis to define the best predictor defined CPP as the only significant predictor for survival with highly significant variance compared to other parameters (F = 15.302, p < 0.001) and for favorable outcome CPP was the significant predictor in two models with highly significant variance versus other parameters followed by DBP in one model, ().
Table 4 Regression analysis of evaluated hemodynamic parameters evaluated at time of catheter removal as predictors for survival and favorable outcome.
Analysis of the impact of variance of the estimated hemodynamic parameters at the time of catheter removal versus at the time of catheter insertion using ROC curve analysis as predictors for survival as a primary favorable outcome defined disturbed ICP as the significant sensitive predictor (AUC = 0.203, p = 0.021) and disturbed SBP as a significant predictor (AUC = 0.768, p = 0.037), ()
4 Discussion
The present study recorded hemodynamic variability between survivors and non-survivors and between those progressed favorably compared to patients who had an unfavorable outcome. These data indicated the value of the evaluation of hemodynamic instability as a measure for body-trauma response and for evaluation of autonomic instability. However, statistical analyses defined the hemodynamic measures at the time of catheter removal, i.e., 5 days after trauma inflection as the significant time for evaluation other than at the time of catheter insertion; this was manifested as the persistent significance of CPP as a predictor for outcome in two regression analysis models and DBP in one model versus other parameters.
Considering CPP as the numerical difference between MAP and ICP and MAP as the resultant of equation including both SBP and DBP, thus estimated CPP could be considered as a reflection of these systemic and local hemodynamic parameters. These data go in hand with Kapapa et al. [Citation12] who analyzed the effect of CPP-orientated management and who tried to find factors that influence outcome and found that MAP, central venous pressure, and heart rate alone do not correlate with outcome and at least one occurrence of MAP and central venous pressure below the lower limits resulted in a poor outcome, while CPP-guided therapy seems to prevent further brain damage and results in outcome scores that are comparable to those children with head trauma exhibiting symptoms of mild brain edema.
The reported significantly higher CPP in survivors and in those having favorable outcome indicated both stable MAP that showed significant lower variability compared to non-survivors and survivors with unfavorable outcome and significantly lower ICP that showed significantly lower levels in survivors compared to non-survivors. These findings indicated the fact that well maintained cerebral and CSF circulation allowed minimization of the impact of inflected trauma and resumption of normal brain function and could be attributed to the fact that normalization of ICP will minimize brain edema and together with improving cerebral perfusion through adequate CPP allows withdrawal of edema fluid and edema resolution. Such finding goes in hand with Nujaimin et al. [Citation13] who found a statistically significant relationship between ICP as well as CPP with both states of basal cistern and the degree of diffuse injury and edema based on the Marshall classification system, and ICP was higher while CPP and compliance were lower whenever the basal cisterns were effaced in cases of cerebral edema with Marshall III and IV.
Also, improved cerebral perfusion allowed proper cerebral oxygenation and provision of nutrients, and anti-inflammatory cytokines. Such attribution supported that previously reported by Meixensberger et al. [Citation14] who found cerebral hypoxic events can be reduced significantly by increasing CPP and by Stiefel et al. [Citation15] who reported immediate and sustained decrease in ICP and an increase in CPP with improvement of cerebral oxygenation up to a 114.8% increase and the change in brain tissue O2 and the change in ICP demonstrated a relationship after decompressive hemicranectomy. Moreover, Figaji et al. [Citation16] found low CPP and/or high mean ICP to >20 affects brain tissue oxygen tension in pediatrics severe traumatic brain injury.
Evaluation of the diagnostic yield of hemodynamic variability determination using ROC curve analysis defined variability of ICP as the significant sensitive and SBP variability as specific predictors for favorable general outcome. Also, considering DBP was defined as predictor for outcome using regression analysis, these data indicated the role played by hemodynamic stability for achieving favorable general outcome. In hand with these results, Chaiwat et al. [Citation17] examined the relationship between cerebral hemodynamic predictors, including cerebral autoregulation, and long-term outcome after severe pediatric TBI and found impaired cerebral autoregulation and SBP <5th percentiles were independent risk factors for poor outcome. Kahraman et al. [Citation18] found increased ICP up to 40 mmHg (actual or impending brain death) evoked an increase in HR and PP variability, but both were suppressed with CPP <50 mmHg and ICP >40 mmHg and mean HR and PP variability predicted in-hospital mortality.
The current study relied on intraventricular insertion of ICP sensor either during operative interference or insertion through Kocher's pathway, no catheter was inserted intraparenechymal, epidural or subdural depending on the previously stated by Kinoshita et al. [Citation19] who compared the intraparenchymal ICP versus ventricular ICP monitoring and observed high systemic vascular resistance index and low cardiac index in the intraparenchymal group, while ventricular ICP group exhibited a significant reduction in the total fluid infusion volume of crystalloid and a reduction in the frequency of hypotensive episodes after the mannitol infusion.
Concerning feasibility and safety of intraventricular catheter insertion, only three patients had hemorrhage and five patients had infection necessitating catheter removal for a complication rate of 15.7%. Similarly, Zeng and Gao [Citation20] reported that the complications associated with intraventricular ICP monitoring included hemorrhage and infection that occurred in one patient and five patients, respectively, but there were no unacceptable complications related to ICP monitoring.
5 Conclusion
It could be concluded that hemodynamic stability for children had TBI which is mandatory for the improvement of their outcome with high ICP and low CPP with concomitant large range of SBP variability which could be considered as predictors for bad outcome and must be monitored throughout ICU stay. Intraventicular catheter ICP monitoring is feasible and a safe procedure with minimal complication rate.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- G.PortellaM.CormioG.CiterioContinuous cerebral compliance monitoring in severe head injury: its relationship with intracranial pressure and cerebral perfusion pressureActa Neurochir81Suppl.2002173175
- V.H.GraciasO.D.GuillamondeguiM.F.StiefelE.M.WilenskyS.BloomR.GuptaJ.P.PryorP.M.ReillyP.D.LerouxC.W.SchwabCerebral cortical oxygenation: a pilot studyJ Trauma5632004469474
- N.StocchettiL.LonghiE.R.ZanierIntracranial pressure monitoring for traumatic brain injury: available evidence and clinical implicationsMinerva Anestesiol7452008197203
- A.MarmarouS.SignorettiG.AygokP.FatourosG.PortellaTraumatic brain edema in diffuse and focal injury: cellular or vasogenic?Acta Neurochir96Suppl.20062429
- A.MarmarouPathophysiology of traumatic brain edema: current conceptsActa Neurochir86Suppl.2003710
- O.L.CremerG.W.van DijkE.van WensenG.J.BrekelmansK.G.MoonsL.P.LeenenC.J.KalkmanEffect of intracranial pressure monitoring and targeted intensive care on functional outcome after severe head injuryCrit Care Med3310200522072213
- M.BalestreriM.CzosnykaP.HutchinsonL.A.SteinerM.HilerP.SmielewskiJ.D.PickardImpact of intracranial pressure and cerebral perfusion pressure on severe disability and mortality after head injuryNeurocrit Care412006813
- N.StocchettiA.ColomboF.OrtolanoW.VidettaR.MarchesiL.LonghiE.R.ZanierTime course of intracranial hypertension after traumatic brain injuryJ Neurotrauma248200713391346
- D.GrinkevièiûtëR.KëvalasÐaferisA.MatukevièiusV.RagaiðisA.TamaðauskasPredictive value of scoring system in severe pediatric head injuryMedicina (Kaunas)43112007861869
- P.D.AdelsonS.L.BrattonN.A.CarneyR.M.ChesnutH.M.du CoudreyB.GoldsteinGuidelines for the acute medical management of severe traumatic brain injury in infants, children and adolescentsPediatr Crit Care Med4Suppl.2003S171
- B.JennettDevelopment of Glasgow Coma and Outcome ScalesNepal J Neurosci220052428
- T.KapapaK.KönigU.PfisterM.SasseD.WoischneckH.HeisslerE.RickelsHead trauma in children, part 2: course and discharge with outcomeJ Child Neurol2532010274283
- U.NujaiminA.SaufiA.G.RahmanI.BadrisyahS.SaniI.ZamzuriM.KamarulA.JafriPost traumatic cerebral oedema in severe head injury is related to intracranial pressure and cerebral perfusion pressure but not to cerebral complianceAsian J Surg3232009157162
- J.MeixensbergerM.JaegerA.VäthJ.DingsE.KunzeK.RoosenBrain tissue oxygen guided treatment supplementing ICP/CPP therapy after traumatic brain injuryJ Neurol Neurosurg Psychiatry7462003760764
- M.F.StiefelG.G.HeuerM.J.SmithS.BloomE.Maloney-WilenskyV.H.GraciasM.S.GradyP.D.LeRouxCerebral oxygenation following decompressive hemicraniectomy for the treatment of refractory intracranial hypertensionJ Neurosurg10122004241247
- A.A.FigajiE.ZwaneC.ThompsonA.G.FieggenA.C.ArgentP.D.Le RouxJ.C.PeterBrain tissue oxygen tension monitoring in pediatric severe traumatic brain injury Part 2: Relationship with clinical, physiological, and treatment factorsChilds Nerv Syst2510200913351343
- O.ChaiwatD.SharmaY.UdomphornW.M.ArmsteadM.S.VavilalaCerebral hemodynamic predictors of poor 6-month Glasgow Outcome Score in severe pediatric traumatic brain injuryJ Neurotrauma2652009657663
- S.KahramanR.P.DuttonP.HuL.StansburyY.XiaoD.M.SteinT.M.ScaleaHeart rate and pulse pressure variability are associated with intractable intracranial hypertension after severe traumatic brain injuryJ Neurosurg Anesthesiol2242010296302
- K.KinoshitaA.SakuraiA.UtagawaT.EbiharaM.FurukawaT.MoriyaK.OkunoA.YoshitakeE.NodaK.TanjohImportance of cerebral perfusion pressure management using cerebrospinal drainage in severe traumatic brain injuryActa Neurochir96Suppl.20063739
- T.ZengL.GaoManagement of patients with severe traumatic brain injury guided by intraventricular intracranial pressure monitoring: a report of 136 casesChin J Traumatol1332010146151