Abstract
Background
The practice of airway management has become more advanced in recent years. This advancement is demonstrated by the introduction of many new airway devices, several of which have been included in the American Society of Anesthesiology (ASA).
The most recently developed is air-Q which has special features and benefits that make it characteristic.
The success rate of blind intubation versus fiberoptic intubation through air-Q was investigated in this study. Success rate and quality of fiberoptic guided intubations were assessed.
Method
This study was conducted on 80 patients who underwent urosurgical operations under general anesthesia. Patients were randomly allocated into two equal groups (n = 40): group I in which intubation was done blindly through air-Q, and group II in which intubation was done by FO through air-Q. All the patients were meticulously assessed by El Ganzouri score. Patients taking points from 0 to 4 were only allowed to be included in this study to avoid the use of the awake technique if the score was 5 or more. After induction of anesthesia patients were primarily ventilated with the air Q. Then the endotracheal tube was inserted either blindly or by FO through the air Q. Successful intubation was confirmed by chest wall movement, auscultation, and capnogram. After three trials of intubations the procedure was abandoned. Twenty-four hours post-intubation, patients were questioned on the occurrence of sore throat and hoarseness.
Results
The success rate in blind intubation was 70% while in FO intubation was 97.5%.and this difference was statistically significant (p < 0.05). The total time to intubate in seconds was longer in group I than in group II and this difference was statistically significant (p < 0.05).
Conclusion
In our patients the air Q appeared to be a safe supraglottic airway in general anesthesia with a low potential for trauma of the airway. It is used as a facilitator for blind intubation. It allowed successful blind intubation in 70% of the patients versus 97.5% using fiberoptic technique. Backed up by the presence of a flexible fiberscope, this device might be a useful alternative for the handling of difficult airway.
1 Introduction
Classic laryngeal mask airway (LMA) has been the cornerstone in the management of difficult airway [Citation1].
In 2005, Daniel Cookgas (St. Louis, MO, USA) has invented the new supraglottic device (air Q). It is used for efficient ventilation or endotracheal intubation and it was designed for smoother and easier insertion of the tube.
The air-Q was designed primarily to allow for the passage of conventional cuffed tracheal tubes when used for blind tracheal intubation [Citation2].
The air Q intubating laryngeal airway (ILA) has undergone several refinements in design since its original introduction to the market. Importantly, the posterior portion or ‘heel’ of the cuff was enlarged based on post-market clinical experience indicating that air leaks were typically occurring between the posterior portion of the cuff and the base of the tongue [Citation3].
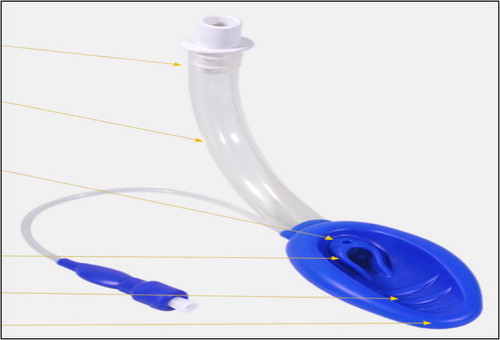
The laryngeal mask air Q has special features and benefits which make it characteristic: Innovative tip design which prevents mask from folding, allowing a smarter insertion, an auxiliary hole that improves air flow and helps prevent epiglottic down-folding, an oval-shaped, hyper-curved airway tube which better approximates the anatomy for easy insertion, and a keyhole-shaped airway outlet to direct the ETT midline toward the laryngeal inlet facilitate intubation and mask ridges to improve anterior mask seal.
The success rate of blind intubation versus using fiberoptic laryngoscopy as a guide for intubation was investigated in this study.
2 Methods
This randomized controlled study was carried out in Kasr El Ainy Hospital. This study was conducted on 80 patients with ASA (I–II) who underwent urosurgical operations after the approval of institutional review board and obtaining the consent of the patients who were asked to receive general anesthesia, our patients were randomly assigned (by closed envelope) to two equal groups according to the used technique of endotracheal intubation as follows:
Group I: consisting of 40 patients who underwent blind endotracheal intubation using laryngeal mask air-Q.
Group II: consisting of 40 patients who underwent fiberoptic endotracheal intubation through air Q from the start.
Patients were meticulously assessed preoperatively by El Ganzouri score which includes seven criteria: Mallampati classification, body weight, head and neck movement, interincisor gap, Buck teeth, thyromental distance, and history of difficult intubation.
El Ganzouri scoring system was used according to those criteria to assess the expected difficulty of intubation [Citation4].
2.1 Technique of insertion
2.1.1 Preparation of the air Q
Insertion of the proper size previously deflated and well lubricated endotracheal tube through the air Q to a depth of approximately 8–20 cm, depending on the air Q size. This will place the distal tip of the endotracheal tube at or just proximal to the opening of the air Q airway tube within the mask cavity. It is very important to lubricate the endotracheal tube and the air Q airway tube completely to ensure easy passage of the endotracheal through the air Q. The endotracheal connector must be removed and loosely reattached to its place, this will facilitate the removal during the application of the removal stylet.
The air Q balloon is deflated by suctioning the pilot balloon until two dimples on the under surface of the cuff appear.
2.1.2 Anesthesia technique
After administration of 100% oxygen for 3 min, atropinization of the patient using 0.1 mg atropine, anesthesia was conducted using fentanyl 1–2 mg/kg followed by propofol 2 mg/kg and atracurium 0.5 mg/kg. The patient is mechanically ventilated using a face mask aided with inhalation anesthetic isoflurane until a full relaxation is established after about 3–5 min.
The air Q is held by the right hand, and a wooden tongue depressor is used by the left hand to facilitate introduction of the mask. Drive the mask by applying continuous pressure over the shaft until it stops. Flexion of the head may facilitate the application.
In another way tongue depression may be done using pressure of the left thumb. Tongue holding and jaw thrust may also be used.
The cuff of the air Q was inflated according to the manufacturer’s instructions. 5–10 cm3 of air is sufficient to inflate the cuff of the air Q. Our goal was to achieve a minimum leak (seal pressure or oropharyngeal leak pressure) of less than 40 cm H2O. Leak pressures can be assessed by auscultation over the anterior neck and chest while observing the ventilator manometer during positive pressure ventilation. It can be measured by closing the expiratory valve of the circle system at a fixed gas flow of 3 l/min and noting the airway pressure.
Mechanical ventilation of about 10 ml/kg was established.
Time of insertion; is the time in seconds from touching the patients mouth with the air Q until capnographic confirmation.
2.1.3 Insertion of the ETT
For endotracheal intubation the ventilator is disconnected and the mask adaptor is also disconnected.
2.1.3.1 Blind tube insertion
It was tried aided by cricoid pressure until the tube passed into its place. The cuff of the tube was inflated and the cuff of the air Q was deflated. Then the tube is connected to the ventilator. Verification of tracheal intubation was done by capnogram. The depth of the tube was assessed either by auscultation or by fiberscope to ensure that its place is above the carina.
Scoring of the trial according to the time it lasts until capnographic confirmation is either score 2: time less than 50 s, score 1: time more than 50 s.
2.1.3.2 Fiber optic technique
Using a fiberoptic endoscope, pass the scope through the ETT and into the trachea under direct visualization using the scope as a guide. The scope was then removed and the ETT cuff was inflated and the tube connector was replaced, connection to the ventilator was established, and check for adequate ventilation was assessed.
2.1.4 Air Q removal procedure
Removing the air Q following the ETT intubation is easily accomplished with the aid of the air Q removal stylet. Three sizes are available. It consists of an adaptor connected to a rod. The adaptor is tapered from bottom to top to allow the stylet to accommodate multiple sizes of the ETT, and has horizontal ridges which engage the ETT in a firm secure grip for a good control of the user during the removal process and vertical grooves to facilitate the spontaneous breathing in spontaneously breathing patients.
2.2 Statistical methods
Data management and analysis were performed using SigmaStat program, version 3.5 (Systat Software Inc., USA). The graphs were done using Microsoft Excel 2007. The numerical data were statistically presented in terms of range, mean, standard deviation, median and interquartile range (IQR). Categorical data were summarized as percentages.
Comparisons between numerical variables of two groups were done by unpaired Student’s t-test for parametric data or Mann–Whitney Rank Sum test for non-parametric data. Comparing categorical variables were done by χ2-test or Fisher exact test for small sample size. Z-test (at a confidence interval of 95%) was used for comparing single proportions.
All p-values were considered significant when p-values less than 0.05.
3 Results
This study was conducted on total of 80 patients. The study group consisted of 54 (67.5%) males and 26 (32.5%) females; with a male to female ratio (2.1:1). Mean patient age was 44.087 ± 15.201 (range: 18–70 years) and mean patient weight 75.025 ± 13.956 (range: 50–120 kg) ().
Table 1 Comparison of the baseline demographic characteristics between group I and group II.
There were no statistically significant differences in age, weight and gender characteristics of patients between the two groups (p > 0.05) ().
Frequency distribution of the studied cases according to the airway score is showed in .
Table 2 Comparison of the frequency distribution to the air way score between group I and group II.
The median airway score of group I was statistically higher than that of group II, and difference was statistically significant (p = 0.007) ().
Table 3 Comparison of the characteristics between group I and group II.
As regards the insertion technique; insertion by jaw thrusting and tongue holding was more common in group I (62.5%), while jaw elevation was more common in group II (72.5%); this difference was statistically significant (p = 0.003) ().
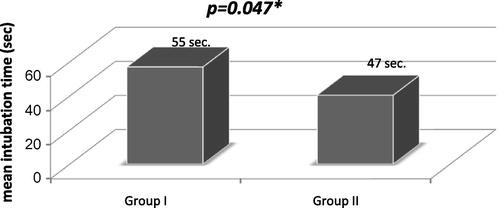
The total time to intubate in seconds was longer in group I than in group II and this difference was statistically significant (p < 0.05) ( and ).
In group I, 28 out of the total 40 patients (70%) had a successful intubation; where 22/28 (78.6%) were intubated in the first attempt but in one of them extraction during the removal of air Q occurred, three (10.7%) were intubated in two attempts and other three (10.7%) patients needed a 3rd attempt. 12/40 (30%) patients had failed the three attempts.
Regarding the total time to intubate in group I; 18/28 (64.3%) patients were intubated within less than 50 s (score 2) and 10/28 (35.7%) patients were intubated within more than 50 s (score 1) ().
In group II, 39/40 (97.5%) were successfully intubated; 34/40 (85%) were intubated successfully in the first attempt while five (12.5%) cases needed a second attempt that succeeded after deflation of the cuff or slight upward traction of the air Q in an attempt to visualize the glottis opening. The remaining one (2.5%) failed to be intubated in one of the three trials due to excessive secretions and blood resulted from multiple trials.
Regarding the total time to intubate in group II; 30/40 (75%) patients were intubated within less than 50 s (score 2) and 10/40 (25%) patients were intubated within more than 50 s (score 1).
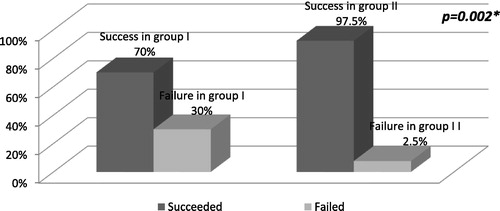
The frequency distribution of successes and failures among group I was statistically significant from that of group II (p = 0.002) ( and ).
Table 4 Comparison of success rate of intubation between group I and group II.
The number of attempts taken for intubation was statistically insignificant between the two groups (p = 0.066) ().
Table 5 Comparison the number of successful attempts taken.
The first time success rate using laryngeal mask air Q was 22/40 (55%); while with the fiberoptic it reached 34/40 (85%); and the difference was statistically significant (p = 0.03) ().
Table 6 Comparison of 1st attempt success rate between group I and group II.
The fate was known for 16/40 patients of group I (40%) with no complications reported. 37/40 patients of group II (92.5%) had a non-complicated course. The data about the rest of the patients were not available.
4 Discussion
Classic LMA is the most widely used supraglottic device all over the world and considered the cornerstone in the management of difficult airway, however, there are some limitations when it is used as a conduit for intubation.
The air-Q intubating laryngeal airway (Cookgas LLC, Mercury Medical, Clearwater, FL) is a new supraglottic airway device ().
The special features of air Q ILA makes it superior to the classic LMA; therefore, it has the potential to overcome the limitations of the classic LMA. The shaft of this airway is much shorter and curved, enough of proximal TT is still above the shaft, allowing for removal of the air Q without the aid of a stabilizing rod [Citation5]. The more curved shaft prevents tube kinking, lack of grills in ventilatory orifice. The airway connector of the air Q ILA is easily removable eliminating this potential area where the pilot balloon of the TT can get stuck [Citation6]. And, the most important is that intubation can be done with a standard normal size tube for age.
Air-Q fulfills the criteria of ideal supraglottic devices which are: ease of placement, reliable alignment of the glottis opening, ability to continuously oxygenate and ventilate, minimize disconnection time from the breath circuit.
There are, however, some limitations to the air Q ILA. It may not improve the view when it is used in conjunction with a flexible fiberscope in the presence of blood and secretions. Even in these situations, the alignment with the glottis anatomy may allow for increased success in the use of ‘light guided’ or blind techniques for intubation. The air Q ILA is of limited value in nasotracheal intubations and patients with no mouth opening [Citation2].
Air Q is available in six sizes (1, 1.5, 2, 2.5, 3.5, 4.5) in disposable single use.
And in four sizes (2, 2.5, 3.5, 4.5) for reusable use.
When looking at complete airway management, the exit strategy can sometimes be just as important as airway placement. There are three sizes of the stabilizing rods.
The air Q offers us a removal stylet. The stylet stabilizes the previously inserted oral endotracheal tube and allows controlled removal of the air Q without dislodging the tube from the trachea.
The taper allows the stylet to accommodate standard endotracheal tubes in multiple sizes (4–8.5).
The ridges engage the endotracheal tube in a firm, secure grip, giving the user control of the endotracheal tube during removal.
The struts allow for a more secure grip on the stylet during the rotational movement of insertion.
Our study was the first to be done in Egypt using air-Q. This study was designed to discover the main differences in intubation using the blind or the fiberoptic technique through the new air Q LMA.
This study was conducted on a total of 80 patients. Our patients were randomly assigned to two equal groups according to the used technique of intubation as follows:
Group I: consisting of 40 patients who underwent blind endotracheal intubation using laryngeal mask air-Q.
Group II: consisting of 40 patients who underwent fiberoptic endotracheal intubation through air Q from the start.
The main findings in our study are that the success rate was 70% in group I compared to 97.5% in group II and this difference was statistically significant.
The total time to intubate in seconds was longer in group I (55.375 ± 19.228) than in group II (47.250 ± 16.678) and this difference was statistically significant (p = 0.047∗).
The overall failure rate within group I was 30%. The failure rate in group II was 2.5%. It was due to excess secretion, and the difference was statistically significant.
The success rate of intubation using fiberoptic is higher and less traumatic compared to blind intubation. With several trials of blind intubation the chance of success of following fiberoptic is limited due to excessive secretion.
The fate was known for 16 (40%) patients of group I where no complications were reported. Thirty-seven patients (92.5%) of group II had a non-complicated course. The data about the rest of the patients were not available.
Erlacher et al. also studied the air Q ILA as a facilitator for blind intubation. He found that the air Q appeared to be a safe supra glottic airway in general anesthesia with a low potential for traumatization. Used as a facilitator for blind intubation it allowed endotracheal intubation in 60% of the patients. Backed up by the presence of a flexible fiberscope this device might be a useful alternative for the handling of difficult airway [Citation7].
The available studies are limited so further studies are needed to confirm our outcome and results.
As conclusion, air-Q is a new supraglottic device which can be used as an excellent ventilatory device as well as conduit for endotracheal intubation with the standard tube either blindly or by aid of fiberoptic.
This device can be used safely in the management of patients with difficult airway.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- David E.SwansonA comparison of the intubating laryngeal airway (ILM) with the laryngeal mask airwayAnesthesiology1052006A1283
- N.JagannathanA.G.RothL.E.SohnT.Y.PakS.AminS.SureshThe new air-Q intubating laryngeal airway for tracheal intubation in children with anticipated difficult airway: a case seriesPaediatr Anaesth192009618622
- E.J.BakkerM.ValkenburgE.M.GalvinPilot study of the air-Q intubating laryngeal airway in clinical useAnaesth Intensive Care382010346348
- A.R.El-GanzouriR.J.McArthyPreoperative airway assessment: predictive value of a multivariate risk indexAnesth Analg82199611971204
- M.YamashitaLonger tube length eases tracheal intubation via the LMA in infants and childrenJ Clin Anesth91997432433
- M.WeissK.GoldmannCaution when using cuffed tracheal tubes for fiberoptic intubation through paediatric-sized LMAActa Anesthesiol Scand482004523
- WolfgangErlacherThe Cookgas air Q, a new supraglottic airway as a facilitator for blind intubationAnesthesiology1092008A293