Abstract
Objective
To evaluate the effect of general anaesthesia with either continuous i.v. opioids (G/O) or thoracic epidural analgesia (G/EP) on postoperative transient myocardial ischaemia (TMI) in type 2 diabetic patients undergoing open cholecystectomy.
Methodology
This randomised controlled study was conducted on 50 patients with D.M. Patients were divided into G/O group or G/EP group. All patients had negative stress exercise test and at least two cardiac risks preoperatively. Epidural analgesia was established by 15 ml of ropivacaine 0.2% with fentanyl 2 μg/ml followed by 5–8 ml/h of ropivacaine 0.1% with fentanyl 1 μg for 24 h postoperatively. Both studied groups received same general anaesthesia. Continuous i.v. fentanyl 100 μg/h was given intraoperatively in group G/O followed by i.v. morphine PCA. Primary outcome measured postoperative TMI using 24 h continuous ST segment analysis, endothelin-1(ET-1), troponin T, creatine kinase MB (CK-MB), and CKMB/CK preoperatively, 8 h and 24 h postoperatively. Second outcome measured dynamic stress (perioperative heart rate, blood pressure and postoperative pain).
Results
Endothelin-1 was above cutoff level preoperatively and rose up dramatically postoperatively in both studied groups. G/EP attenuated ET-1 elevation than G/O. Troponin T and CK-MB did not rise postoperatively in both studied groups. Postoperative CK-MB/ CK ratio was higher than 10% in 12 and eight patients in group G/O and G/EP, respectively. Twelve cardiac ischaemic events were noticed in four patients in group G/O and four events in two patients in group G/EP without significant difference in total duration of ischaemia between groups. G/EP lowered HR more significantly intraoperatively and gave better pain control for 4 h postoperatively. In conclusion, D.M was associated with high ET-1 level. Upper abdominal surgery increased ET-1 release. G/EP attenuated ET-1 release more than G/O and produced more stable haemodynamic parameters and less postoperative pain. No superior cardioprotective effect was noticed in G/EP over G/O.
1 Introduction
The incidence of patients with diabetes mellitus (D.M) undergoing surgical procedures increases each year. This incidence is going to rise as prevalence of diabetes is predicted to be 300 million by the end of 2025. Diabetes mellitus is a major risk factor for perioperative cardiac complications and death. Myocardial ischaemia in particular is the most frequent complication in patients with diabetes and accounts for approximately 1.4% in patients undergoing noncardiac surgery. It is often lethal, increases cost of hospital stay and compromises a patient’s quality of life after surgery [Citation1,Citation2].

Attempts to improve perioperative outcome of diabetic patients with risk for developing coronary artery disease (CAD) have focused on two main approaches. The first is deep understanding to the pathogenesis of D.M and its impact on cardiovascular disease. This can help in early diagnosis and better management of cardiovascular sequence. The second is to attenuate deleterious effect of surgical stress in those patients using a preventive anaesthetics [Citation2].
The persistent hyperglycemia is a risk factor for developing endothelial dysfunction that enhances atherosclerotic cardiovascular complications in patients with diabetes [Citation3]. It stimulates cytokines production that decreases the new synthesis of collagen by vascular smooth muscle cells. So it alters vascular smooth muscle function and favouring atherosclerosis formation. Furthermore, diabetes enhances the release of some protolytic enzymes that lead to breakdown of collagen. When collagen breakdown increases and synthesis decreases, atheromatous plaques may rupture more easily, triggering thrombus formation [Citation4].
Diabetes mellitus enhances endothelin-1 (EL-1) release. It is a potent vasoconstrictor deriving from endothelium cells and stimulated by several stimuli such as renal failure, ischaemic heart disease, systemic or pulmonary hypertension [Citation5]. It is suggested that increased endothelin in diabetes is responsible for development of its cardiovascular sequel. Recent investigations [Citation6,Citation7] reported higher concentrations of ET-1 in serum of patients with ischaemic heart disease, particularly its unstable character. High values were observed in patients with myocardial infarction and heart failure. Although it has high sensitivity towards cardiovascular disease (CVD), its low specificity could not make it a standard predictor of postoperative cardiovascular outcome in diabetics.
Lastly, diabetes is frequently associated with silent ischaemia. Autonomic neuropathy is suggested to be the main factor for relatively high incidence of painless ischaemia in diabetics [Citation8]. So patients do not report chest pain and myocardial infarction may be suddenly discovered at preoperative time. Accordingly, pathogenesis of diabetes makes careful preoperative assessment of cardiovascular to be very essential.
Surgery is characterised by a hypercoagulable response due to increased platelet number and function, diminished fibrinolysis, decreased natural anticoagulants and increased procoagulants. Hypercoagulable response in addition to sympathetic activation caused by intra and postoperative stress is an important factor mediating the increased incidence of perioperative coronary insufficiency [Citation9,Citation10]. Therefore, types of anaesthesia delivered to patients with diabetes should target to reduce neuro-hormonal surgical stress and improve overall outcome after surgery. Considerable debate still remains over the advantages and disadvantages of combined regional–general anaesthesia compared with general anaesthesia in prevention of cardiovascular dysfunction in the patient with diabetes undergoing noncardiac surgery [Citation11].
2 Aim of the work
The aim of the current study was to investigate the effect of general anaesthesia with intraoperative and postoperative i.v. opioid analgesia or thoracic epidural analgesia on some clinical and biochemical predictors of postoperative transient myocardial ischaemia in patients with D.M type 2 undergoing upper abdominal surgery.
3 Participants and methods
After obtaining Ethical Committee approval of Medical Research Institute and taking patients’ consents, the current randomised controlled parallel-group study was conducted on 50 patients with diabetes mellitus type 2 scheduled for open cholecystectomy.
3.1 Inclusion criteria
All patients were American Society of Anesthesiologists physical status II (ASA 11), scheduled for open cholecystectomy at Medical Research Institute hospital, Alexandria University, Egypt. They all have D.M type 2, glycosylated haemoglobin was <8.5%, negative stress exercise test to exclude preoperative ischaemic coronary disease therefore helping in evaluating the preventive role of the two analgesic techniques on postoperative ischaemic insult. All patients have at least two risk factors for developing coronary artery disease: in addition to D.M and abdominal surgery, Age >60 years, sedentary lifestyle, total cholesterol ⩾240 mg/dl, LDL ⩾ 160 mg/dl, or HDL <35 mg/dl, current smoking, family history of premature CAD[Citation12].
3.2 Exclusion criteria
Any patient with history of coronary artery disease, heart failure, hypertension, respiratory, renal or hepatic insufficiency, having any contraindications for epidural anaesthesia was excluded from the study.
3.3 Randomisation and blinding of the study
A block-wise balanced randomisation procedure was used. The allocation to general anaesthesia with either opioid analgesia or thoracic epidural analgesia was done on cards that were sealed into opaque and consecutively numbered envelopes. These envelopes were opened after taking decision for operation. Data collection and analysis were conducted by a neutral researcher who was blinded with anaesthetic and analgesic techniques.
3.4 Anaesthesia and patients’ grouping
Patients were divided according to types of perioperative analgesia into general anaesthesia with continuous opioid analgesia (Group G/O) or thoracic epidural analgesia (Group G/EP).
3.5 Epidural block
After preparation of skin and while patient was in sitting position, 19 G epidural catheter was inserted through Toughy needle and advanced 3 cm in epidural space between 7th and 8th thoracic vertebra using loss of resistance to air technique. Epidural blockade was established with initial bolus of 15 ml of ropivacaine 0.2% with fentanyl 2 μg/ml then an infusion pump started to provide a continuous mixture of 5–8 ml/h of ropivacaine 0.1% and fentanyl 1 μg/ml epidural for 24 h postoperatively.
3.6 General anaesthesia
All patients were premedicated with midazolam 0.03 mg/kg and fentanyl 0.5 μg/kg intravenously just before transfer to operative theatre. Induction of general anaesthesia in both studied groups was carried out using: fentanyl 2 μg/kg, propofol 1–2 mg/kg, and atracurium 0.5 mg/kg for tracheal intubation. Anaesthesia was maintained with isoflurane1-2%, air–oxygen mixture and atracurium 0.3 mg/kg. Atracurium was given to maintain one twitch of train of four of nerve stimulation.
3.7 Analgesic requirement
Intraoperative analgesic requirement in group G/O was achieved with continuous i.v. fentanyl 100 μg/h. Postoperative analgesia was maintained by i.v. morphine patient control analgesia (PCA) (Master PCA, Fresenius-KABI) at concentration of 1 mg/ml using 1 ml/h basal rate and 1 ml PCA with lock out time 6 min and 10 ml maximum dose/hour for the first 6 h then 1 ml PCA bolus doses was used without continuous basal rate infusion for the entire 24 h postoperative.
3.8 Measurements
Plasma lipid profile including triglyceride, total cholesterol (TC) concentration, high density lipoprotein cholesterol (HDL-C) and low density lipoprotein cholesterol (LDL-C) were analysed by an autoanalyser (Hitachi 7170, Tokyo, Japan) [Citation13]. It was measured preoperatively to recognise diabetic patient with high risk to develop coronary artery disease.
Cardiac ischaemia was evaluated biochemically and clinically. Biochemical evaluation measured plasma endothelin-1 and serum cardiac biomarkers; creatine kinase (CK), MB fraction (CK-MB) and cardiac troponin T (cTnT). They were assessed preoperatively, 8 h and 24 h postoperatively. Estimation of EDTA plasma ET-1 level was done using noncompetitive sandwich immunosorbance assay (R&D systems kit (catalog#BBE5) Minneapolis, MN, USA). After the extraction procedure for plasma samples, the standards, controls and extracted plasma were added into the wells that pre-coated with ET-1 antibodies. Then any ET-1 present was sandwiched by the horseradish peroxidase enzyme-linked to specific ET-1 antibody conjugate. After an incubation and washing steps, a substrate solution (tetamethyl benzidine) was added to the wells and the intensity of the colour was stopped by acid solution after the second incubation. The intensity of the colour was measured using microplate reader set at 450 nm and 620 nm. Subtraction of reading at 620 from that 450 nm to correct for optical imperfections in the plate. The concentrations of ET-1 in the samples were obtained from standard curve drawn on semi logarithmic paper, where the concentration of standard on the X-axis and mean absorbance of each standard on the Y-axis. The cutoff EDTA plasma ET-1 value was 0.6 ± 0.2 pg/ml. CK and CK-MB fraction were measured by autoanalyser technique. The upper limit of normal for CK total was 170 U/l [Citation13]. The CK-MB increase was considered positive (CKMB+) when total CK elevation was twice baseline, with the ratio of CK-MB to total CK >10% of total CK, as determined from serial samples at 8 h and 24 h postoperatively [Citation14]. Troponin T enzyme immunoassay (Boehringer Mannheim, Germany, and ELISA (ES-300) analyser) were used for cTnT assay. Normal cTnT reading ranged 0.0–0.1 ng/ml, values of >0.1 ng/ml were therefore considered to be positive [Citation15].
Clinical evaluation was done by ST segment analysis using 24 h continuous postoperative digital ambulatory 3 leads ECG recorder (VX3-E 2710, USA) with compact flash ELITE 512 PROE. ST Segment was analysed by expert cardiologist who was blinded to research design. Transient myocardial ischaemia (TMI) was defined as an elevation or a depression in the ST level from baseline in one or more leads lasting one or more minutes. Total numbers of ischaemic events per 24 h and their duration were calculated [Citation16].
Stress of surgery was assessed clinically. Clinical parameters included perioperative heart rate (HR) and mean arterial blood pressure (MABP) that was measured 10 min interval intraoperatively and at postanaesthetic care unit (PACU) admission then every 4 h for 24 h postoperatively. In addition visual analogue scale (VAS) (0–10 cm) for assessment of postoperative pain was recorded every 4 h postoperatively. Total morphine and ropivacaine fentanyl mixture were calculated for 24 h postoperatively.
Postoperative complications including excessive sedation, nausea, vomiting pruritus and/or motor paresis were recorded.
3.9 Statistical analysis
Data were analysed using SPSS software version 18.0. The sample size was calculated using NCSS 2003. Twenty-five patients in each studied group achieved 91% power at alpha 0.05 and detected the difference between groups based on previous study [Citation17] on ET-1 (mean = 2.0 ± SD = 0.2) as biomarker of biomechanical stress after surgery and cardiac troponin T [Citation18] as a diagnostic biomarker of ischaemia under the influence of epidural analgesia using two sided Mann–Whitney. Quantitative data were expressed as mean ± SD and analysed using Student t test for comparing two studied groups and Paired t test for comparing values in same group. When multiple comparisons were made in same group, the Bonferroni correction was applied. Qualitative data (sex, number of ischaemic events and association of ischaemic events, CK-MB and ET-1) were representing in frequency, percent and analysed using Chi square test and Fisher exact test. P value was assumed to be significant at 0.05 or less.
4 Results
Demographic data were matching in both studied groups. Preoperative risk factors for developing perioperative myocardial ischaemia and duration of diabetes did not show significant difference between the studied groups ().
Table 1 Demographic data and patients’ characteristic in the studied groups.
Plasma endothelin-1 was above cutoff level at preoperative time and rose up dramatically at postoperative time in both studied groups. But its rise was less in group G/EP than group G/O. Troponin T and CK-MB did not show significant rise at postoperative time compared to preoperative values in both studied groups. In spite of that, CK-MB/CK total was noticed to be higher than 10% in twelve patients in group G/O and eight patients in group G/EP postoperatively ().
Table 2 Cardiac biomarkers (endothelin-1, troponin T and creatine kinase) in both studied groups (mean ± SD).
Analysis of postoperative cardiac ischaemic events showed 12 cardiac ischaemic events (mostly ST segment depression) in four patients in group G/O with mean duration of 7.25 min and four events in two patients in group G/EP with mean duration of 7.50 min. Number and duration of these ischaemic insults did not significantly differ between the studied groups (). All patients with ischaemic events did not report clinical cardiac symptoms except one in group G/O reported brief chest tightness. Three of four patients (75%) with cardiac events have positive CK-MB/CK ratio (>10%) in group G/O and two of two (100%) in group G/EP. No significant association between ischaemic events and CK-MB ratio in both studied groups. All patients with ischaemic insult in both groups (100%) have elevated ET-1 but none of them got high troponin level ().
Table 3 Cardiac ischaemic events in both studied groups (mean ± SD).
Table 4 Association of cardiac ischaemic events, CK-MB/CK, and endothelin-1.
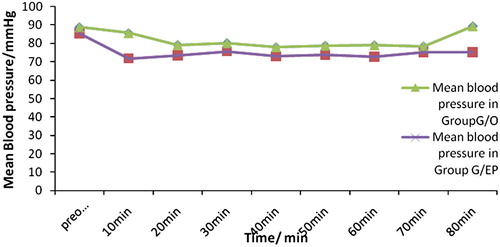
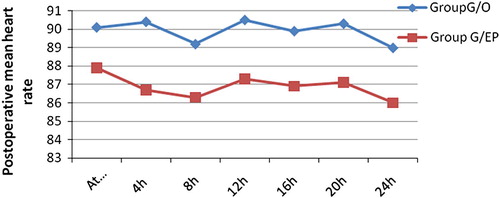
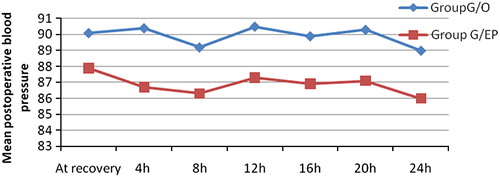
Intraoperative heart rate and blood pressure showed steady decline compared with preoperative reading in both groups. Addition of epidural analgesia to general anaesthesia lowered HR significantly intraoperatively but it did not decrease blood pressure dramatically than general anaesthesia intraoperatively or postoperatively ().
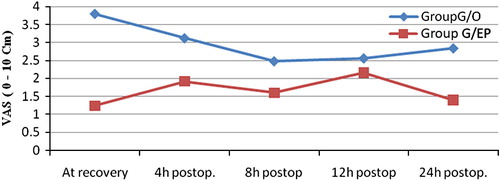
Visual analogue scale was significantly less in group G/EP immediately and 4 h postoperative compared with group G/O. After that time there was no significant difference in VAS between the two groups .
Mean morphine consumption in 24 h postoperatively was 15.2 mg ± 4.052 in group G/O and ropivacain/fentanyl mixture was 128 mg ropivacaine/128 μg fentanyl ± 17.32 in group G/EP.
With regard to postoperative complications seven patients in group G/O and two patients in group G/EP complained of nausea, vomiting. Five patients have drowsiness in group G/O and one in group G/EP. There was no significant difference in postoperative complications between the studied groups.
5 Discussion
All anaesthetists are aware that diabetic patients undergoing abdominal surgery may be at a risk for developing perioperative myocardial ischaemia. Sustained stress and increased metabolic demand during perioperative period in addition to diabetes associated endothelial dysfunction and autonomic neuropathy increase the chance of postoperative cardiovascular complications. Therefore, screening of preoperative cardiovascular risk, administration of prophylactic medications and balanced anaesthesia may achieve better cardiovascular outcome [Citation19].
All diabetic patients included in the current study have cardiovascular risks at preoperative time. Seven patients had cholesterol level above 240 mg/dl in group G/O and nine patients in group G/EP. Twelve patients in group G/O and 10 patients in group G/EP had LDL higher than 160 mg/dl. HDL less than 35 mg/dl was observed in 12 and nine patients in group G/O and G/EP, respectively. Triglycerides level more than 200 mg/dl was noticed in nine patients in group G/O and seven patients in group G/EP. Smoking and family history of ischaemic heart disease were reported by 10 patients in group G/O and 15 patients in group G/EP.
Dyslipidaemia is a common pathogenesis associated with D.M. It may precede signs and symptoms of D.M by several years and may be the primary factor in developing both D.M and atherosclerotic cardiovascular disease (CVD) [Citation20]. The positive correlation between hypercholesterolaemia (core stone of atherosclerotic plaque) and CVD had been evident in previous studies [Citation21,Citation22]. Hypertriglyceridaemia as a risk promoting CVD has been debated. Earlier studies [Citation23,Citation24] failed to find strong association of triglyceride and coronary artery disease after adjustment of either total cholesterol and LDL (univariate analysis). However, latter meta-analysis [Citation25] showed that, hypertriglyceridaemia in combination with low HDL-C was considered unique risk for CVD (multivariate analysis). Miller et al. [Citation26] supported strong link between high triglyceride and CVD in people with lower levels of HDL-C and LDL-C with type 2 diabetes. Smoking is another cardiac risk factor producing severe vascular spasm [Citation27]. All previous cardiovascular risks were recommended to be screened by American Diabetes Association and Société Française de Cardiologie/Association de Langue Française pour l’Etude du DIAbète et des Maladies métaboliques (SFC/ALFEDIAM) for early diagnosis and better management [Citation28].
Endothelin-1 is a 21-amino-acid peptide released from endothelial cells and exerts diverse actions in the cardiovascular system. It is a powerful vasoconstrictor and has direct positive inotropic and chronotropic effects in the heart [Citation29].
In the current study, the mean basal value of endothelin-l was above cutoff level in the studied groups preoperatively under the influence of diabetes. Surgical stress stimulates ET-1 release and doubled its value postoperatively in both studied groups. G/EP attenuated ET-1production more than G/O. The attenuation of ET-1 production in G/EP may explain in a part the decreased HR in this group. In addition, it could exert more obvious protective role and give better cardiovascular outcome if it was evaluated in larger sample size.
The present result was consistent with the finding obtained by Schneider et al. [Citation30] who denoted that, diabetic patients often have endothelial dysfunction and elevated ET-1 level which was partly responsible for developing atherosclerotic vascular insufficiency. Tsai et al. [Citation17] reported that, ET-1 associated D.M may lead to coronary vascular tone abnormality and inappropriate coronary blood flow in response to increasing myocardial demand during and after surgery. Shirakami et al. [Citation31] investigated the effect of major and minor surgery on perioperative ET-1 activity and reported a significantly increased plasma ET-1 level under major surgical stress. However no significant change was observed in minor surgery. ET-1 activity was evaluated under the effect of inhaled anaesthetics in a previous study [Citation32] which demonstrated that isofluranee inhibited ET-1 vascular contraction at 1 minimal alveolar concentration. It also denoted that vasodilatation and hypotension induced by inhaled anaesthetic may be attributed to interaction with ET-1 at vascular endothelium cells. Taking this finding in concern, attenuation of ET-1 under the influence of combined general epidural anaesthesia could provide more protection on cardiovascular system by lowering HR and reducing after load.
Although troponin T and CK-MB did not significantly change postoperatively in the present study, CK total was significantly increased and CK-MB/CK total was noticed to be higher than 10% in 12 patients in group G/O and eight patients in group G/EP postoperatively. Postoperative troponin and CK-MB readings showed that no irreversible cardiac ischaemic insult occurred at postoperative time. Cardiac troponin and CK-MB are good biomarkers for diagnosing a myocardial infarction. Troponin is more sensitive and more specific than CK-MB. However, their release in response to reversible injury has been debated for years [Citation33]. In animal experiments, increased CK in blood was associated with evidence of irreversible cardiac injury [Citation34].
Carlson et al. [Citation35] and Babuin et al. [Citation36] confirmed that troponin elevations were not detected in humans after reversible ischaemia.
Increased CK and ratio of CK-MB/CK total in the current study may be as a result of surgical trauma. CK-MB is a good marker strongly suggestive of acute coronary infarction in acute medical condition. But it is difficult to be as so good after surgical procedure. Surgical trauma stimulated CK-MB release from skeletal muscle and gave a false-positive CK-MB value for MI. The specificity of CK-MB could be enhanced by the calculation of the CK-MB/CK total ratio. However, the use of this ratio markedly reduced sensitivity in patients with concurrent skeletal muscle injury [Citation37,Citation38].
In the present study, continuous cardiac ischaemic monitoring revealed 12 transient cardiac ischaemic events (mostly ST segment depression) in four patients in group G/O and four events in two patients in group G/EP. There was no significant difference in number or duration of ischaemic events between the studied groups. This finding reported that G/EP was not superior than G/O in prevention of cardiac ischaemia in the present research. Although, epidural analgesia provided some benefits over opioid analgesia in controlling postoperative pain during the first 4 h postoperatively, postoperative pain was tolerable (VAS < 4 cm) in both studied groups.
Proposed mechanisms for postoperative myocardial infarction are either neurohormonal–metabolic stress, endothelium dysfunction and/or the release of inflammatory mediators. The protective effect of general and regional anaesthesia on decreasing stress response that could be reflected positively on cardiovascular outcome was investigated in several previous studies [Citation39–Citation42]. All concluded that high dose opioid based general anaesthesia and high thoracic epidural general anaesthesia can attenuate endocrine-metabolic effect in upper abdominal surgery and could reduce perioperative myocardial ischaemia. The role of volatile anaesthetics in reducing myocardial infarction size by preconditioning effect on coronary artery was reported in one study [Citation43]. In spite of these encouraging results, a lot of debate still exists as use of high dose opioid needed postoperative mechanical ventilation which increased the health care cost. High epidural analgesia even very high up to C 6 failed in obtunding neurohormonal axis completely in upper abdominal operation. Furthermore, none of previous anaesthetic techniques can suppress most of inflammatory mediators or vasoconstrictor endothelial driving factors in response to surgery [Citation10].
In conclusion, type 2 D.M was associated with high ET-1 level at preoperative time. Surgical stress related to upper abdominal operation increased ET-1 release postoperatively. Patients with uncomplicated D.M type 2 underwent upper abdominal surgery have a risk for developing TMI. G/EP attenuated ET-1 release more than G/O and produced more stable haemodynamic parameters and less postoperative pain. No superior cardiovascular protective effect for G/EP over G/O. Further investigations are recommended to evaluate the effect of continuous perioperative epidural analgesia in prevention of new cardiac ischaemia or re-ischaemia in patients with or without complications in D.M type 2, done on large sample size and for more prolonged period (more than 24 h).
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- H.KingR.E.AuburtW.HermanGlobal burden of diabetes 1995–2025. Prevalence, numerical estimates and projectionDiabetes Care21200014141421
- Ellis EJ, Illinois C. Myocardial ischemia and postoperative monitoring; 2007. http://www.csaol.cn/img/2007asa/RCL_src/314_Ellis.
- R.KleinB.E.KleinS.E.MossGlycosylated hemoglobin predicts the incidence and progression of diabetic complicationsJAMA234199828642871
- R.H.EckelM.WassefA.ChaitPrevention conference in diabetes and cardiovascular disease. Writing group II: Pathogenesis of atherosclerosis in diabetesCirculation1052002e138e143
- B.SármánM.TóthA.SomogyiRole of endothelin-1 in diabetes mellitusDiabetes Metab Rev141998171175
- R.CelińskiUsefulness of endothelin-1 determinations in the diagnosis of cardiovascular diseasesPol Merkuriusz Lek282010220222
- T.OmlandR.T.LieA.AakvaagPlasma endothelin determination as a prognostic indicator of 1-year mortality after acute myocardial infarctionCirculation114200615731579
- D.ZieglerCardiovascular autonomic neuropathy: clinical manifestations and measurementDiabetes Rev172000300315
- J.P.DesboroughThe stress response to trauma and surgeryBr J Anaesth852000109117
- G.NicholsonHormonal and metabolic responses to traumaAnaesth Intensive Care Med62005313314
- B.DrengerRisk evaluation and anaesthetic strategy in perioperative myocardial ischaemiaAnaesth Pain Intensive Care Emerg92006551558
- O.BarthelemyL.C.FeuvreJ.TimsitSilent myocardial ischemia screening in patients with diabetes mellitusArq Bras Endocrinol Metab512007285293
- C.BurtisE.AshwoodD.BrunsZ.TietFundamentals of clinical chemistry6th ed2008Saunders ElsevierUSA
- R.G.IrvinF.R.CobbC.R.RoeAcute myocardial infarction and MB creatine phosphokinaseArch Intern Med1401980329334
- R.ShaveE.DawsonG.WhiteThe cardio specificity of the third generation troponin T assay after exercise induced muscle damageMed Sci Sports Exerc342002651654
- J.K.BookerK.HolmJ.BarbaraFrequency and outcomes of transient myocardial ischemia in critically ill adults admitted for noncardiac conditionsAm J Crit Care122003508517
- H.P.TsaiJ.J.LiuY.S.ChouEffect of lower extremity bypass surgery on inflammatory reaction and endothelial dysfunction in type 2 diabetic patientsMediators Inflamm20092009417301417304
- S.SuttnerK.LangN.SwenContinuous intra- and postoperative thoracic epidural analgesia attenuates brain natriuretic peptide release after major abdominal surgeryAnesth Analg1012005896903
- L.A.FleisherK.A.EagleLowering cardiac risk in noncardiac surgeryN Engl J Med345200116771682
- S.M.HaffnerH.MiettinenInsulin resistance implications for type II diabetes mellitus and coronary heart diseaseAm J Med1032003152162
- N.R.RoblesS.BarrosoG.MarcosLipid control in diabetic patients in SpainEndocrinol Nutr562009112117
- N.Cortez-DiasS.MartinsA.BeloPrevalence, management and control of diabetes mellitus and associated risk factors in primary health care in PortugalRev Port Cardiol292010509537
- M.H.CriquiG.HeissR.CohnPlasma triglyceride level and mortality from coronary heart diseaseN Engl J Med328199312201225
- J.JeppesenH.O.HeinP.SuadicaniTriglyceride concentration and ischemic heart disease: an eight-year follow-up in the Copenhagen Male StudyCirculation97199810291036
- E.Di AngelantonioN.SarwarP.PerryMajor lipids, apolipoproteins, and risk of vascular diseaseJAMA302200919932000
- M.MillerJ.N.StoneC.H.BallantyneTriglycerides and cardiovascular disease a scientific statement from the American Heart AssociationCirculation1232011 00-00
- J.PuelP.ValensiG.VanzettoV.Lassmann-VagueJ.L.MoninP.MoulinALFEDIAM; SFC. Identification of myocardial ischemia in the diabetic patient. ALFEDIAM and SFC recommendationsDiabetes Metab3020043S318
- O.BarthelemyC.Le FeuvreJ.TimsitSilent myocardial ischemia screening in patients with diabetes mellitusArq Bras Endocrinol Metab512007285293
- A.C.SharmaA.GulatiRole of endothelin in regional vascular systemA.GulatiEndothelin: role in health and disease1995Harwood Academic PublishersAmsterdam215232
- J.G.SchneiderN.TillyT.HierlElevated plasma endothelin-1 levels in diabetes mellitusAm J Hypertens152002967972
- G.ShirakamiK.TagaT.TanakaRelationship between tissue ischemia and venous endothelin-1 during abdominal aortic aneurysm surgeryJ Cardiothorac Vasc Anesth191998510514
- A.BoiliotB.ValletJ.MartyEffects of halothane, enflurane and isofluranee on contraction of rat aorta induced by endothelin-1Br J Anaesth751995761767
- P.C.HaggartP.F.LudmanA.W.BradburyCardiac troponin: a new biochemical marker for peri-operative myocardial injuryEur J Vasc Endovasc Surg222001301305
- Y.IshikawaJ.E.SaffitzT.L.MealmanReversible myocardial ischemic injury is not associated with increased creatine kinase activity in plasmaClin Chem46719974375
- R.J.CarlsonA.NavoneJ.P.McConnellEffect of myocardial ischemia on cardiac troponin I and TAm J Cardiol892002224226
- L.BabuinS.A.JaffeTroponin: the biomarker of choice for the detection of cardiac injuryCMAJ173200511911203
- J.E.AdamsIIIG.A.SicardB.T.AllenDiagnosis of perioperative myocardial infarction with measurement of cardiac troponin IN Engl J Med3301994670674
- J.E.AdamsIIIV.G.Davila-RomanP.Q.BesseyImproved detection of cardiac contusion with cardiac troponin IAm Heart J1311996308312
- C.KlingstedtK.GieseckeB.HambergerP.-O.JanbergHigh- and low-dose fentanyl anaesthesia, circulatory and catecholamine responses during cholecystectomyBr J Anaesth591987184188
- K.OlaussonH.MagnusdottirL.LurjeAnti-ischemic and anti-anginal effects of thoracic epidural anesthesia versus those of conventional medical therapy in the treatment of severe refractory unstable angina pectorisCirculation96199721782182
- S.BlombergH.EmanuelssonH.KvistEffects of thoracic epidural anesthesia on coronary arteries and arterioles in patients with coronary artery diseaseAnesthesiology1122000840847
- A.RodgersN.WalkerS.SchugA.McKeeH.KehletA.van ZundertReduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trialsBMJ321200014931497
- K.TanakaL.M.LudwigJ.R.KerstenP.S.PagelD.C.WarltierMechanisms of cardioprotection by volatile anestheticsAnesthesiology1002004707721