Abstract
Objective
The aim of this study was to evaluate the efficacy of prophylactic pregabalin on postdural puncture headache incidence and severity after spinal anesthesia.
Method
86 ASA I-II male and female patients age 20–50 years old, undergoing elective general surgeries below the umbilicus under spinal anesthesia with 3 ml heavy bupivacaine 0.5% (15 mg), patients were randomly allocated into one of two groups (Group C, n = 43) (control group) received a placebo capsule 2 h preoperatively (Group P, n = 43) received 150 mg pregabalin capsule 2 h preoperatively, number of attempts for spinal block, sensory level, motor block grade, postoperative time to first analgesic requirement, the incidence, onset and intensity of PDPH and adverse events were recorded for 72 h.
Results
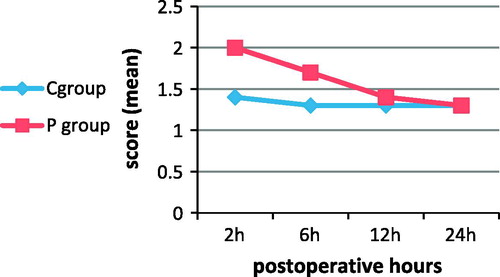
The peak sensory level in C group and P group showed no statistical significant difference, the time to peak sensory block was significantly earlier in P group than group C, the time to reach the modified Bromage motor block grade 3 was significantly earlier in P group than C group, time to two segment regression of sensory level to S1 and motor block regression to modified Bromage grade 0 were statistically insignificant between the studied groups. Group P had a significantly longer time to first analgesic requirements than group C, and there was no significant difference in VAS (visual analogue scale) of pain between the studied groups. There was significant increase in sedation score in P group compared to C group at 2 h and 6 h postoperatively, and there was statistically significant reduction in the incidence rate and severity of PDPH in P group compared to group C. There were no recorded cases of dizziness, visual disturbances, or PONV.
Conclusions
preoperative oral pregabalin 150 mg reduced the incidence and severity of PDPH, beside the earlier onset of peak sensory and motor block with increase duration of analgesia in patients undergoing elective surgeries under spinal anesthesia.
Keywords:
1 Introduction
Postdural puncture headache (PDPH) is unpleasant complication following dural puncture. The incidence of PDPH following dural puncture ranges from 0.3% to 20% in spinal anesthesia and up to 70% after accidental dural puncture in epidural anesthesia [Citation1]. The incidence rate of PDPH is related to age, gender, needle size, pregnancy, and a previous history of PDPH [Citation2]. PDPH is characterized by severe, dull nonthrobing pain, often fronto-occipital, aggravated by erect or sitting position coughing, sneezing or straining, and diminished in supine position. It may be associated with nausea, vomiting, or visual disturbances [Citation3]. Headache starts one or 2 days after spinal anesthesia and if left untreated, relieved spontaneously after a week [Citation3,Citation4].
The real etiology of PDPH is not fully understood, but mostly the decreased CSF volume as a result of CSF leakage leading to reduced pressure and cerebral venodilation [Citation1,Citation5,Citation6].
Pregabalin is an antiepileptic drug, it is a structural analogue of gamma-aminobutyric acid (GABA), and it is effective in reducing hyperalgesia in pain model and may play an important role in acute postoperative pain in humans [Citation7].
It was reported that pregabalin may be useful for the management of PDPH in patients who developed PDPH after spinal anesthesia or diagnostic and/or therapeutic lumbar puncture [Citation8].
To our knowledge, there is no study used pregabalin as a prophylaxis agent against PDPH. This study was designed to evaluate the efficacy of prophylactic pregabalin on postdural puncture headache incidence and severity after spinal anesthesia.
2 Patients and method
After approval of the ethical committee, a written informed consent was obtained, this double blind study was conducted on 86 patients of both sex, ASA I&II aged 20–50 years old, planned for elective general surgeries below the umbilicus (repair of inguinal hernia, varicocele, and varicose vein) under spinal anesthesia at El – Mansoura Main University Hospital from January 2012 to July 2012. Patients were excluded from the study if they had history convulsions, diabetes, those with known allergy to amide local anesthetic or to the study drugs, or any contraindication to regional anesthesia (e.g., local infection, coagulation abnormality, tight valvular heart lesion, or patient refusal), patients with psychological, spinal cord deformity, previous spinal surgery, and pregnant and patients with chronic headache were also excluded. The study protocol was explained to each patient during the preoperative visit. No premedication was given to the patients. In the operating room, 18 G intravenous cannula was inserted and IV normal saline at a rate of 10 ml kg−1 was started. Intraoperative monitoring every 10 min includes the following: Electrocardiogram, pulse oximetry, and noninvasive arterial blood pressure. The patients were randomly divided to one of two groups using closed envelope technique for randomization, to maintain the blind nature of the study, the studied drug were given by a well trained anesthesia resident (unaware of the study drugs) according to the instructions written in a sealed envelope and were given to the patients in the ward as follows: Group C (control group) (n = 43): received a placebo capsule 2 h preoperatively. Group P (n = 43): received 150 mg pregabalin capsule (vronogabic) 150 mg pregabalin capsule 2 h preoperatively. Spinal anesthesia was performed under strict aseptic technique in the sitting position, 2 ml lidocaine 2% for local infiltration of the skin at L3–L4 or L4–L5 space, then insertion of 25-G Quincke type spinal needle by midline approach, when free flow of CSF was obtained, a 3 ml heavy bupivacaine 0.5% (15 mg) was injected, spinal needle was withdrawn, and the patients were put in the supine position immediately, supplemented with oxygen 3 l/min by face mask.
At the end of surgery, patient was transferred to PACU where they were monitored and received supplemental oxygen (4 l min−1) by facemask for 1 h; then, they were shifted to the wards.
The following parameters were evaluated and recorded by an anesthesiologist unaware of the study drugs: Patient characteristics, number of attempts to perform spinal anesthesia, and sensory level were assessed by pin prick 5 min after completion of spinal anesthesia. Motor block was evaluated by the modified Bromage motor scale (Grade 0: No motor block, Grade 1 Inability to raise extended leg; able to move knees and feet, Grade 2: Inability to raise extended leg and move knee; able to move feet, Grade 3: Complete motor block of limb) 5 min after the completion of spinal anesthesia, time to peak sensory block and to two segment regression (minutes), onset time to modified Bromage 3 and time of regression to modified Bromage 0 (minutes).
The postoperative pain at rest was assessed using VAS (visual analogue scale), where zero score corresponds to no pain and 10 to the maximum or worst pain, if VASS ⩾ 4, 75 mg diclofenac sodium intramuscular/12 h was planned to be given. The onset, incidence, and severity of PDPH in 72 h were recorded, time to rescue analgesia in minutes. The intensity of the headache was assessed according to a previous study [Citation9]: Class I: Patient suffers from a mild headache while sitting or walking, Class II: Patient suffers from a moderate to severe headache while sitting or walking, Class III: Patient suffers from a moderate to severe headache even in supine position which impedes his/her daily activities. Sedation was assessed by Ramsy et al. sedation score [Citation10] and other complications such as dizziness, nausea, and vomiting visual disturbances were recorded. If any patient complained from PDPH, bed rest, hydration was tried, and if the PDPH was not relieved, oral paracetamol 500 mg with caffeine 65 mg (panadol extra, Galaxo Smith)/8 h was planned to be given.
3 Statistical analysis
Sample size was calculated by using one tail z test in G *power 3.1.5 program. According to a pilot study (10 patients in each group), we calculated that 43 patients per each group were sufficient to give p < 0.05 significant with confidence interval 95% with a actual power of 95% when incidence rate of PDPH in placebo group was (4) and in pregabalin group was (1). Statistical analyses were performed using SPSS 16 (SPSS Inc., Chicago, IL, USA). Parametric data were analyzed using the independent t-test. Nonparametric data were compared using Mann–Whitney test. Chi-square test was used for comparison between percentages and frequencies. All values were expressed as mean (SD), number or percentage (%) of patient. Significance level was established at a p value ⩽ 0.05.
4 Results
Eighty-six patients were enrolled and completed; this study had statistically insignificant differences among patients demographic (age, sex, and weight) and duration of surgery (). The peak sensory level reached was T6 (T6–T8) in (C) group, T7 (T5–T8) in (P) group without any statistical difference between the groups, but the time to peak sensory block was significantly earlier in (P) group than group (C) (p = 0.05) (). All patients achieved modified Bromage motor block grade 3 which was significantly earlier in (P) group than (C) group (p = 0.02), Time to two segment regression, sensory level regression to S1 and motor block regression to modified Bromage motor block grade 0 were statistically insignificant among the studied groups (). Group (P) had a significantly longer time to first analgesic requirement than group (C) (p = 0.04) (), and there was no significant difference in VAS of pain between studied groups (). There was significant increase in sedation score in (P) group compared with (C) group at 2 h and 6 h postoperatively (p ⩽ 0.001). There was statistically significant reduction in the incidence rate of PDPH in (P) group 7(16%) compared with group (C) 13(30%) (p = 0.02) with significant reduction in the intensity of PDPH; in group (P), one patient (14%) had class III PDPH compared to group (C) in which six patients (46%) had class III PDPH (p = 0.008), and there was no significant differences between the studied groups as regard the number of needle attempts (). Four patients had Class I PDPH in Group P and 3 in Group C relived with bed rest, good hydration, and patients who had Class II and III PDPH received oral paracetamol 500 mg with caffeine 65 mg (panadol extra, Galaxo Smith)/8 h.
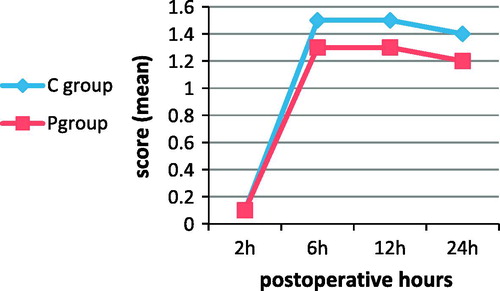
Table 1 Demographic characteristics of patients in the study groups. Data were expressed as mean ± SD and numbers.
Table 2 Spinal block characteristics (onset and regression time of sensory and motor blocks in minutes). Data were expressed as mean ± SD.
Table 3 PDPH characters (incidence rate, intensity classes, time of onset (day), and number of needle attempts). Data were expressed in number with or without (%).
There were no recorded cases of dizziness or postoperative nausea and vomiting or visual disturbances (see ).
5 Discussion
The results of the present study showed that prophylactic oral pregabalin 150 mg 2 h before surgery was effective in reduction in the incidence and severity of postdural puncture headache, with earlier onset of peak sensory and motor block with increase duration of analgesia compared to a placebo in patients undergoing elective surgeries under spinal anesthesia, this may be due to the actions of pregabalin as analgesic, anti-hyperalgesic, and anxiolytic [Citation11,Citation12], the main mechanism of action pregablin is through blocking the development of hyperalgesia and central sensitization, and it binds to the α2-δ_ subunit of voltage-gated calcium channels with binding affinity six times more than that of gabapentin, reducing the release of excitatory neurotransmitters including glutamate, noradrenaline, serotonin, dopamine, and substance P. Additionally, it also produces an inhibitory modulation of neuronal excitability in areas of the central nervous system dense in synaptic connections as the neocortex, amygdala, and hippocampus [Citation12–Citation14]. Zencirci [Citation7] reported that oral pregabalin 150 mg/day reduced the severity of postdural puncture headache in two females who did not respond to conventional treatments with oral paracetamol and caffeine (300 mg/day), bed rest and hydration and 200 mg intravenous theophylline infusion for 36 h with no recorded side effects except sedation. Huseyinoglu and coworkers [Citation8] found that oral pregabalin was effective in treatment of PDPH after spinal anesthesia or diagnostic and/or therapeutic lumbar puncture, patients were given 150 mg/day oral pregabalin for the first 3 days, and then, 300 mg/day for further 2 days had significantly lower visual analog scale scores after the second day of treatment. In the same line of our results, Ghai et al. [Citation15] documented that single dose of 300 mg pregabalin 1–2 h prior to abdominal hysterectomy associated with increased the time to first request for analgesia. Moreover, another study showed that oral premedication with pregabalin 150 and 300 mg reduced analgesic consumption in laparoscopic hysterectomy [Citation16].
6 Conclusion
Preoperative oral pregabalin 150 mg reduced the incidence and severity of PDPH, beside the earlier onset of peak sensory and motor block with increase duration of analgesia in patients undergoing elective surgeries under spinal anesthesia.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- AlamaRaheenbK.M.IqbalcChowdhurydHeadache following spinal anaesthesia: a review on recent updateJ Bangladesh Coll Phys Surg2920113240
- S.T.VilmingR.KlosterL.SandvikThe importance of sex, age, needle size, height and body mass index in postlumbar puncture headacheCephalalgia2172001738743
- A.HennessyN.EustaceJ.GardinerA.LaneLong-term headache following epidural analgesiaIr Med J.951200226
- P.T.ChoiS.E.GalinskiL.TakeuciS.LucasC.TamayoA.R.JadadPDPH is a common complication of neuroaxial blockade in parturient: a meta-analysis of obstetrical studiesCan J Anesth5052003460469
- FaramarzMosaffaKhodamoradKarimiFiroozMadadiSeyyed HasanKhoshnevisLalehDaftariBesheliAlirezaEajaziPost-dural puncture headache: a comparison between median and paramedian approaches in orthopedic patientsAnesth Pain Med1220114448
- Mohammad RezaDoroudianMehrdadNorouziMohammadEsmailieRoozbehTanhaeivashDexamethasone in preventing post-dural puncture headache: a randomized, double-blind, placebo-controlled trialActa Anaesth Belg622011143146
- BeyazitZencirciPostdural puncture headache and pregabalinJ Pain Res320101114
- U.HuseyinogluN.HuseyinogluE.HamurtekinH.AygunB.SuluEffect of pregabalin on post-dural-puncture headache following spinal anesthesia and lumbar punctureJ Clin Neurosci1810201113651368
- A.EsmaogluH.AkpinarF.UgurOral multidose caffeine paracetamolcombination is not effective for the prophy – laxis of postduralJ Clin Anesth1720055861
- M.A.RamsayT.M.SavegeB.R.SimpsonR.GoodwinControlled sedation with alphaxolone–alphadaloneBMJ21974656659
- B.F.ShnekerJ.W.McAuleyPregabalin: a new neuromodulator with broad therapeutic indicationsAnn Pharmacother39200520292037
- B.A.ChizhM.GohringA.TrosterG.K.QuarteyM.SchmelzW.KoppertEffects of oral pregabalin and aprepitant on pain and central sensitization in the electrical hyperalgesia model in human volunteersBr J Anaesth982007246254
- J.ZhangK.-Y.HoY.WangEfficacy of pregabalin in acute postoperative pain: a meta-analysisBr J Anaesth10642011454462
- D.McClellandR.EvansL.BarkworthD.MartinR.ScottA study comparing the actions of gabapentin and pregabalin on the electrophysiological properties of cultured DRG neurones from neonatal ratsBMC Pharmacology4200414
- AnjuGhaiMonikaGuptaSarlaHoodaDineshSinglaRamanWadheraA randomized controlled trial to compare pregabalin with gabapentin for postoperative pain in abdominal hysterectomySaudi J Anaesth532011252257
- R.JokelaJ.AhonenM.TaligrenM.HaanpaaK.KortillaA randomized controlled trial of perioperative administration of pregabalin for pain after laparoscopic hysterectomyPain1342008106112