Abstract
Objective
This study was conducted to compare the efficacy and safety of addition of two drugs; clonidine versus fentanyl to epidural levobupivacaine to control postoperative pain after radical cystectomy surgery.
Patients and Methods
All urinary bladder cancer patients of both sex, ASA I and II, 40–70 years undergoing radical cystectomy surgery in National Cancer Institute (NCI) from November 2011 till May 2012 are the target group of which 50 patients accepted to share in the study, they are randomly classified by permuted block technique into two groups; group C (clonidine) who received 6 ml of levobupivacaine 0.25% + clonidine 75 μg epidural bolus dose followed by continuous epidural infusion of levobupivacaine 0.125% + clonidine 2 μg/ml at a total rate of 6–10 ml/h, and group F (fentanyl) who received 6 ml of levobupivacaine 0.25% + fentanyl 50 μg bolus dose followed by continuous epidural infusion of levobupivacaine 0.125% + fentanyl 2 μg/ml at a total rate of 6–10 ml/h. Paracetamol 1 g IV infusion was used as a rescue pain treatment. In both groups epidural activation is done after complete recovery from balanced general anesthesia. In both groups we measured vital signs (HR, MBP, RR), 0–10 visual analogue scale (VAS) and Sedation using the four-point Ramsay Sedation Scale are assessed for first 24 h postoperatively. In addition we recorded the total 24 h rescue paracetamol dose needed and side effects of both drugs were also observed.
Results
We found that there is no statistical significant difference between both groups in the vital signs (HR, MBP, and RR), analgesic efficacy (VAS), and Sedation effects (Sedation Scale), and all data were within clinically accepted range. There was no statistically significant difference in total 24 h paracetamol rescue dose needed in both groups with the same range (1–3 g/24 h) and same median value (2 g/24 h). Recorded side effects were minimal and insignificant in both groups.
Conclusion
We concluded that both clonidine and fentanyl can be used as effective additive to epidural levobubivacaine for postoperative analgesia after radical cystectomy with no significant difference between them in vital signs, analgesic, sedative effects and safety profile on adding each of them in doses not exceeding 20 μg/h to epidural continuous levobupivacaine infusion.
1 Introduction
Control of postoperative pain is an important concern of anesthesiologists [Citation1]. One of the good methods is multimodal pain therapy “balanced analgesia” based on the hypothesis that a combination of analgesics with different sites of action may improve overall pain relief [Citation2]. Epidural administration of combined local anesthetics and opioids may provide improved pain relief but still carries the risk of side effects when doses approach levels necessary for total pain relief [Citation3–Citation7].
Levobupivacaine, the pure S-enantiomer of bupivacaine, is theoretically safer alternative than its racemic parent [Citation8,Citation9]. It has been claimed to be more potent than bupivacaine [Citation10,Citation11] or ropivacaine [Citation12], in addition to cause less motor impairment [Citation13–Citation15], however little difference was found by evidence based medicine to support this [Citation10].
Clonidine, an α2-adrenergic agonist, reduces but does not eliminate pain after surgery [Citation16–Citation18]. However, with high doses of clonidine, significant hemodynamic depression with hypotension was observed [Citation16–Citation18].
Several studies have been published describing the anesthetic-sparing effects and analgesic properties of epidural clonidine [Citation19–Citation21]. Several reports of epidural clonidine have focused on the optimal doses of clonidine to be used [Citation22–Citation24], rather than analyzing the potential advantages of using epidural clonidine versus opioids with respect to efficacy and incidence of side effects [Citation21,Citation25].
Epidural fentanyl has been used effectively as an alternative to morphine and has been shown to induce fewer complications when compared with epidural morphine [Citation26,Citation27].
The addition of clonidine to epidural local anesthetic as an adjuvant to prolong analgesia has been studied extensively since 1984, by the study of Tamsen and Gordh published in Lancet [Citation28]. However few studies investigated the effect of adding clonidine to levobupivacaine.
The aim of this study was to compare both analgesic efficacy and side effect profile of epidural clonidine versus fentanyl when each of them is added to epidural levobubivacaine.
2 Patients and methods
Ethical approval for this study (Ethical Committee No. 2010011052A.2) was provided by the Institutional Review Board (IRB) of National Cancer Institute-Cairo University, Cairo, Egypt (Chairperson Prof. Dr. Ahmed Morsi Mostafa) at 30/10/2011. This prospective randomized study was conducted on fifty urinary bladder cancer patients who were willing to participate and meet the following inclusion criteria: age 40–70 years old of both sex, ASA I and II undergoing radical cystectomy and urinary diversion in National Cancer Institute (NCI) from November 2011 till May 2012. Fully informed written consent was taken from each patient prior to contribution in the study. Exclusion criteria include hemodynamically unstable patients on vasopressors or inotropes, patients with contraindications to epidural catheter insertion, or patients, refusal. Lumbar epidural catheter is inserted at L3/4 or L4/5 intervertebral space pre-operatively after detection of epidural space by loss of resistance technique and test dose of lidocaine 1% in epinephrine 1:200,000 is injected. Then patients were divided randomly by permuted block technique into two equal groups (twenty-five patients each): Group C (clonidine) and Group F (fentanyl).
Both groups received balanced general anesthesia (Midazolam 0.05 mg/kg, Fentanyl 2 μg/kg, Poropofol 2 mg/kg, Atracurium 0.5 mg/kg then 0.1 mg/kg every 30 min, Sevoflurane 1–2 MAC and Morphine 0.1 mg/kg IM + metoclopramide 10 mg IV) and activation of epidural analgesia is done immediately after complete recovery.
Group C (clonidine) includes twenty-five patients in whom activation of epidural analgesia is done using 6 ml of levobupivacaine (Chirocaine, 2.5 mg/ml, Abbott) 0.25% + clonidine (Catapress ampoule, 150 μg/ml, Boehringer Ingelheim) 75 μg bolus dose followed by continuous epidural infusion of levobupivacaine 0.125% + clonidine 2 μg/ml at a total rate of 6–10 ml/h according to VAS.
Group F (fentanyl) includes twenty-five patients in whom activation of the epidural is done using 6 ml of levobupivacaine (Chirocaine, 2.5 mg/ml, Abbott) 0.25% + fentanyl (Fentanyl ampoule, 50 μg/ml, Janssen Cilag) 50 μg bolus dose followed by continuous epidural infusion of levobupivacaine 0.125% + fentanyl 2 μg/ml at a rate of 6–10 ml/h according to VAS. A vial of paracetamol (Perfalgan, Bristol Myers Squibb) 1 g IV infusion over 20 min was given as rescue treatment analgesia with maximum dose of 3000 g/24 days although the maximum safe daily dose approved for paracetamol is 4000 g [Citation29]. In both groups we measured vital signs (mainly heart rate, respiratory rate, and mean blood pressure) for 24 h, 0–10 visual analogue scale (VAS), Sedation using the four-points Ramsay Sedation Scale [Citation30]: [0: awake and alert, 1: mildly sedated, easily aroused, 2: moderately sedated, aroused by shaking, 3: deeply sedated, difficult to be aroused by physical stimulation] were also assessed for the first 24 h postoperatively. Total dose of paracetamol IV infusion needed in both groups was calculated. In addition major side effects of the used drugs (e.g., respiratory depression, pruritis, nausea and vomiting) were observed and recorded.
3 Statistical methods
Statistical analysis was performed using Statistical Package for Social Sciences, Version 17.0 (SPSS, Inc., Chicago, III, USA) for Windows. Continuous variables were analyzed as mean values ± standard deviation (SD) or median (range) as appropriate. Rates and proportions were calculated for categorical data. For categorical variables, differences were analyzed with χ2 (chi square) tests.
Differences among continuous variables with normal distribution were analyzed by Student’s T-test; for continuous variables without normal distribution, we used non-parametric tests and differences were analyzed by the Mann–Whitney U-test. All tests were 2 tailed, p-values ⩽ 0.05 was considered significant.
4 Results
Regarding the demographic and clinical characteristics of the two groups there was no statistical significant difference between the two groups in age, sex, body mass index and duration of surgery as shown in .
Table 1 Patients characteristics (mean ± SD).
Mean measurements of vital signs in the 1st 24 h after surgery are shown in . No statistical significant difference was found between both groups and all readings were in the normal range; (HR: 70–100 beats/min, MBP: 75–105 mmHg, RR: 16–24 breaths/min). However heart rate showed interesting finding as higher value were observed in group F than group C (p = 0.080). Mean Blood pressure showed higher value in group F than group C with p value = 0.060.
Table 2 Vital signs (mean ± SD).
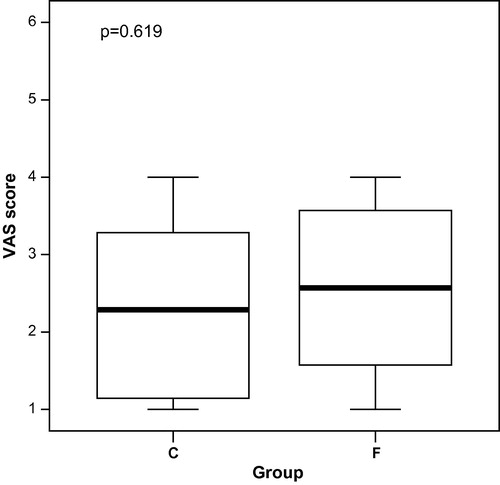
With regard to the means of Sedation Scale and visual analogue scale (VAS) there was no statistically significant difference between both groups as shown in and . The range of Sedation Scale was 0–2, and that of VAS was 1–4.
Table 3 Mean Sedation Scale in both groups, median (range).
The total 24 h dose of rescue treatment with paracetamol IV infusion showed the same range in both groups (1–3 g/24 h) with the same median value 2 g/24 h with no statistical significant difference between both groups (p value = 1.000) (see ).
Table 4 Side effects in the two groups.
Regarding major complications and side effects:
| – | Nausea and vomiting were reported in only 3/25 patients of (F) group and in none of the (C) group patients. | ||||
| – | Hypotension (mean blood pressure reduced by >20%) was not reported although generally patients of the (C) group had a lower blood pressure than those of group (F) with p value > 0.05 | ||||
| – | Respiratory depression was not reported. | ||||
| – | Pruritis in only 2/25 patient of F group. | ||||
5 Discussion
Postoperative pain control is a major concern of anesthesiologists [Citation31]. Epidural route of postoperative analgesia has been used widely as a good method of analgesia [Citation32]. The addition of opioids to local anesthetics epidurally markedly improves quality of analgesia and reduces the dose of local anesthetics [Citation32]. Additives other than opioids including clonidine are used with local anesthetics [Citation33]. In this study we compared the efficacy and safety of addition of clonidine versus fentanyl to epidural levobupivacaine to control post-operative pain after radical cystectomy surgery.
The results of this study showed that there were no statistical significant different data in both groups in vital signs, they were within clinically acceptable range (HR 70–100, MBP 80–105, RR 16–24) and they did not require medical interference. There was no statistically significant difference regarding VAS, and all values of VAS were within clinically accepted ranges and did not require interference as they were less than 4/10. Also for Sedation Scale the results lacked statistical significance and they were within clinically accepted ranges (0–2). Marked side effects (e.g., hypotension, and respiratory depression) were not reported apart from three cases of nausea and vomiting in group F patients and two cases of allergic pruritis in F group.
The results of this present study demonstrated that the analgesic and sedative effects of the combination levobupivacaine–clonidine are clinically equivalent to those of the combination levobupivacaine–fentanyl with nearly similar side effects profile.
Cucchiaro et al. [Citation21] have shown that epidural clonidine is superior to morphine with respect to its side effect profile. However, the authors included in the study patients who had undergone a variety of surgical procedures, making it difficult to compare the analgesic efficacy of the two medications. In our study, we chose patients undergoing radical cystectomy surgery for urinary bladder cancer (a more homogeneous group of patients). We found that the incidence of vomiting, hypotension and Sedation was clinically insignificant in both groups.
Concerns have been raised in the past about the safety and efficacy of epidural clonidine. Studies conducted in women in labor have shown that boluses of epidural clonidine at doses larger than 100 μg may cause significant Sedation [Citation34,Citation35]. However, the incidence of Sedation in our study was minimal and similar among both groups, this most probably because we used smaller doses of clonidine less than 20 μg/h. These results coincides with the results of Sjostrom and Blass who have found that continuous infusion of clonidine at doses ranging between 0 and 20 μg/h in combination with local anesthetics has been shown to have similar sedative effects to epidural fentanyl [Citation36].
Epidural clonidine has been shown to produce hypotension, which has been reported with infusion doses ranging between 20 and 40 μg/h [Citation37]. We used smaller doses of clonidine in our study, and this may explain why no significant hypotension noticed in our study.
The quality of analgesia obtained in the two study groups was similar, as shown by absence of significant difference in VAS scores and similar total 24 h dose of rescue treatment with paracetamol IV (2 g in each group).
In conclusion, this study shows that both clonidine and fentanyl can be used as effective additive to epidural levobubivacaine for postoperative analgesia after radical cystectomy with no significant difference between them in analgesic, sedative effects and safety profile on adding each of them in doses not exceeding 20 μg/h to epidural continuous levobupivacaine infusion. Future studies are needed to get more results about larger doses’ impact on patients’ overall satisfaction with their postoperative care.
Conflict of Interest
None.
Notes
Available online 11 January 2014
References
- S.KuhnK.CookeM.CollinsPerceptions of pain relief after surgeryBr Med J300199016871690
- H.KehletSurgical stress: the role of pain and analgesiaBr J Anaesth631989189195
- R.D.BredtmannN.H.HerdenW.TeichmannEpidural analgesia in colonic surgery: results of a randomized prospective studyBr J Surg77199063842
- H.L.CullenE.D.StarenA.El-GanzouriContinuous epidural infusion for analgesia after major abdominal operations: a randomized, prospective, double-blind studySurgery981985717728
- A.LeeD.SimsomA.WhitfieldPostoperative analgesia by continuous extradural infusion of bupivacaine and diamorphineBr J Anaesth601988845850
- N.B.ScottT.MogensenD.BiglerContinuous thoracic extradural 0.5% bupivacaine with or without morphine: effect on quality of blockade, lung function and the surgical stress responseBr J Anaesth621989253257
- N.C.HjortsØC.LundT.MogensenEpidural morphine improves pain relief and maintains sensory analgesia during continuous epidural bupivacaine after abdominal surgeryAnesth Analg65198610331036
- C.L.BurlacuD.J.BuggyUpdate on local anesthetics: focus on levobupivacaineTher Clin Risk Manage42008381392
- L.E.MatherD.H.ChangCardiotoxicity with modern local anaesthetics: is there a safer choice?Drugs612001333342
- M.CamorciaG.CapognaEpidural levobupivacaine, ropivacaine and bupivacaine in combination with sufentanil in early labor: a randomized trialEur J Anaesthesiol202003636639
- N.SahM.VallejoA.PhelpsEfficacy of ropivacaine, bupivacaine, and levobupivacaine for labor epidural analgesiaJ Clin Anesth192007214217
- D.BenhamouC.GhoshF.J.MercierA randomized sequential allocation study to determine the minimum effective analgesic concentration of levobupivacaine and ropivacaine in patients receiving epidural analgesia for laborAnesthesiology99200313831386
- H.J.LacassieM.O.ColumbThe relative motor blocking potencies of bupivacaine and levobupivacaine in laborAnesth Analg97200315091513
- H.J.LacassieA.S.HabibH.P.LacassieMotor blocking minimum local anesthetic concentrations of bupivacaine, levobupivacaine, and ropivacaine in laborReg Anesth Pain Med322007323329
- Y.BeilinN.R.GuinnH.H.BernsteinLocal anesthetics and mode of delivery: bupivacaine versus ropivacaine versus levobupivacaineAnesth Analg1052007756763
- F.BonnetO.BoicoS.RostaingPostoperative analgesia with extradural clonidineBr J Anaesth631989465469
- J.C.EisenachS.Z.LysakC.V.ViscomiEpidural clonidine analgesia following surgery: phase IAnesthesiology711989640646
- F.BonnetO.BocioS.RostaingClonidine-induced analgesia in postoperative patients. Epidural versus intramuscular administrationAnesthesiology72199042S7
- P.L.BaileyR.J.SperryG.K.JohnsonRespiratory effects of clonidine alone and combined with morphine, in humansAnesthesiology7419914348
- B.ClaesM.SoetensA.Van ZundertClonidine added to bupivacaine–epinephrine–sufentanil improves epidural analgesia during childbirthReg Anesth Pain Med231998540547
- G.CucchiaroC.DagherC.BaujardSide effects of postoperative epidural analgesia in children: a randomized study comparing morphine and clonidinePaediatr Anaesth132003318323
- M.DeKockP.WiederkherA.LaghmicheEpidural clonidine used as the sole analgesic agent during and after abdominal surgery: a dose-response studyAnesthesiology861997285292
- M.CuratoloT.W.SchniderS.Petersen-FelixA direct search procedure to optimize combinations of epidural bupivacaine, fentanyl, and clonidine for postoperative analgesiaAnesthesiology922000325337
- M.CuratoloT.W.SchniderS.Petersen-FelixA direct search p-rocedure to optimize combinations of epidural bupivacaine, fentanyl, and clonidine for postoperative analgesiaAnesthesiology922000325337
- P.DeNegriG.IvaniC.ViscontiThe dose–response relationship for clonidine added to a postoperative continuous epidural infusion of ropivacaine in childrenAnesth Analg9320017176
- S.KizilarslanB.KuvakiU.OnatEpidural fentanyl–bupivacaine compared with clonidine–bupivacaine for analgesia in labourEur J Anaesthesiol172000692697
- J.A.GedneyE.H.C.LiuSide effects of epidural infusions of opioid bupivacaine mixturesAnaesthesia53199811481155
- G.OzalpF.GunerN.KuruPostoperative patient-controlled epidural analgesia with opioid bupivacaine mixtures*Can J Anaesth*451998938942
- A.TamsenT.GordhEpidural clonidine produces analgesiaLancet21984231232
- E.P.KrenzelokM.A.RoyalConfusion: acetaminophen dosing changes based on NO evidence in adultsDrugs RD12220124548
- M.NemethyL.ParoliP.G.Williams-RussoAssessing sedation with regional anesthesia: inter-rater agreement on a modified Wilson sedation scaleAnesth Analg942002723728
- NaliniVadiveluSukanyaMitraDeepakNarayanRecent advances in postoperative pain managementYale J Biol Med83120101125
- R.G.WheatleyS.A.SchugD.WatsonSafety and efficacy of postoperative epidural analgesiaBr J Anaesth8720014761
- J.G.FörsterP.H.RosenbergSmall dose of clonidine mixed with low-dose ropivacaine and fentanyl for epidural analgesia after total knee arthroplastyBr J Anaesth9352004670677
- J.G.FörsterP.H.RosenbergOplasty: a double blind, randomized and placebo-controlled studyActa Anaesthesiol Scan492005538545
- F.RoelantsP.M.Lavand’hommeV.Mercier-FuzierEpidural administration of neostigmine and clonidine to induce labor analgesia: evaluation of efficacy and local anesthetic-sparing effectAnesthesiology102200512051210
- S.SjostromJ.BlassPostoperative analgesia with epidural bupivacaine and low-dose fentanyl: a comparison of two concentrationsActa Anaesthesiol Scand421998776782
- I.DobrydnjovK.AxelssonA.GuptaImproved analgesia with clonidine when added to local anesthetic during combined spinal-epidural anesthesia for hip arthroplasty: a double blind, randomized and placebo-controlled studyActa Anaesthesiol Scan492005538545