Abstract
Background
Dexamethasone has anti-inflammatory properties that can affect postoperative analgesia when added to caudal bupivacaine.
Methods
Seventy-two geriatric patients scheduled for elective total hip replacement under ultrasound guided caudal anesthesia were randomized blindly into two groups: Group BD received caudal isobaric bupivacaine 0.25% (20 ml) and dexamethasone 8 mg (2 ml) and Group BS received caudal isobaric bupivacaine 0.25% (20 ml) and normal saline (2 ml). Postoperative analgesia was assessed by recording time to first rescue analgesia and the analgesic doses (paracetamol and meperidine hydrochloride) required during the first 24 h postoperatively as a primary outcome. Secondary outcomes were the time taken to the onset of sensory analgesia at T10, time to the onset of complete motor block, VAS pain score at rest and on movement at 1, 2, 4, 6, 8, 12 and 24 h, and postoperative adverse events.
Results
Group BD had a significantly longer time to first rescue analgesia [402 (63) vs 213 (53)] min and significantly lower doses of paracetamol [3389 (728) vs 2833 (697)] mg meperidine hydrochloride [78 (30) vs 142 (28)] mg than Group BS. VAS scores were significantly lower in Group BD than Group BS both at rest and on movement respectively at 4, 6, 8, 12 and 24 h.
Conclusion
Adding dexamethasone with isobaric bupivacaine caudal anesthesia prolongs the duration of postoperative analgesia and decreased postoperative analgesic requirement in geriatric patients undergoing total hip replacement surgery in comparison isobaric bupivacaine alone.
1 Introduction
Hip fracture is a common cause of perioperative morbidity and mortality in geriatric age group, 1 in 50 patients more than 60 years old suffered a fracture hip [Citation1]. Perioperative pain management is important in geriatric patients undergoing hip surgery due to their decreased tolerance to stress imposed by surgery [Citation2,Citation3] and can be done either by neuroaxial blockade or by intravenous analgesia [Citation4]. Unfortunately, there are little data showing the outcome of caudal analgesia in geriatric patients undergoing hip replacement surgery.
Various adjuvants have been used in combination with local anesthetics to prolong the duration of postoperative analgesia [Citation5–Citation8]. Dexamethasone could be used as an adjuvant to local anesthetics due to its anti-inflammatory and blocking effects of nociceptor C fiber transmission [Citation9,Citation10]. Ultrasound guided caudal epidural blockade might improve success rate in geriatric patients [Citation11]. This randomized, prospective, double blinded study investigated the effect of single bolus administration of dexamethasone (8 mg) in ultrasound guided caudal blockade as an adjuvant to caudal isobaric bupivacaine (20 ml) 0.25% on postoperative analgesia in geriatric patients undergoing total hip replacement surgery.
2 Methods
The protocol was approved by our institutional review board (IRB) and patient gave written informed consent. Seventy-two patients with ASA I or II, >60 years scheduled for total hip replacement surgery in Ain shams university hospitals were included in this randomized parallel prospective double blinded study by using computer generated randomization list and patients were randomized by opening sequentially numbered opaque envelopes immediately prior to entering the operating room into one of the two groups; control group (Group BS) n = 36 patients and dexamethasone group (Group BD) n = 36 patients. Exclusion criteria included patients with coagulation or hematological disorders, patients with contraindication to regional anesthesia, history of significant coexisting diseases such as ischemic heart disease, uncontrolled hypertension, impaired renal functions, impaired liver functions, rheumatoid arthritis, psychiatric diseases, pre-existing neurological disease, infection at site of injection, patients who had a past history of reaction to study drugs, patients on previous steroid medication or non steroidal anti-inflammatory and patient refusal.
Immediately after admission, patients were instructed to use a 10-point linear Visual analogue scale (VAS) and were asked to record his or her level of perceived pain intensity on the scale from 0 to 10, with the zero representing no pain and the 10 representing the worst pain possible preoperatively. On arrival to the operating room an intravenous access was established using 18 gauge intravenous cannula and patients preloaded with ringer acetate 500 cc intravenous. Patients were monitored using standard monitoring (pulse oximetry, electrocardiogram and noninvasive arterial blood pressure monitoring). Oxygen at 5 L/min was given via a facemask during surgery, and ketamine 0.25 mg/kg and propofol 1 mg/kg were given intravenously 5 min before patient positioning. The high frequency curved ultrasound probe (7–12 MHz) connected to a portable ultrasound unit (Sonoscape) was inserted at first in the transverse plane to detect the sacral cornua (frog sign) and sacral hiatus with the patients in the lateral decubitus position, with the fractured site up then the ultrasound probe was rotated 90° and a 20 gauge spinal needle attached with tubing system to a syringe filled with the local anesthetic solution was inserted in plane in real time visualization of the needle after local skin infiltration with 2 ml lidocaine 2% and passed through the sacrococcygeal ligament (4–6 cm distance) into the sacral canal with the feeling of characteristic click. The needle was advanced only a few millimeters after the penetration of the sacrococcygeal membrane to reduce the risk of dural puncture. After negative aspiration for CSF or blood 3 ml test dose of 1.5% lidocaine HCl was administered at least 5 min prior to local anesthetic required for caudal epidural block which was injected more than 2–3 min and detected by ultrasound turbulence in the sacral canal. Surgery was started 15 min after performing the caudal block with complete motor and sensory block. The bilateral pin prick method was used to detect the sensory level and bromage scale [Citation12] (0 = no motor block, 1 = inability to raise extended leg, 2 = inability to flex knee and 3 = inability to flex ankle and foot) was used to assess caudal blockade at 5, 10, 15 min after caudal epidural administration of drugs.
Hemodynamic parameters were continuously monitored every 5 min till 30 min, every 10 min up to next 30 min and every 15 min thereafter. Hypotension was defined as a decrease in the systolic blood pressure <20% from the baseline treated with 10 mg ephedrine single bolus and bolus administration of 250 ml of lactated Ringer’s solution more than 10 min. Ephedrine 10 mg and 250 ml bolus of lactated ringer solution were repeated if the blood pressure remained low. Bradycardia was defined as heart rate <50 beat per minute treated with 0.3 mg atropine. Patients were randomly included into two groups: Group BD included patients who were given caudal bupivacaine 0.25% (20 ml) and dexamethasone 8 mg (2 ml) and Group BS who were given caudal bupivacaine 0.25% (20 ml) and normal saline (2 ml). All patients in this study were anesthetized by the same team of anesthesiologist and surgeons who were unaware of the study medications.
Both groups were compared as regards patients’ characteristics, hemodynamics, time required to achieve T10 sensory level, onset of complete motor block and use of atropine and ephedrine. Intraoperative complications such as bradycardia, hypotension, nausea, vomiting and shivering were recorded and 4 mg ondansetron was given for patients complaining from nausea or vomiting, whereas 25 mg meperidine hydrochloride was given for attack of shivering. Patients with failed caudal block were excluded from the study and received general anesthesia.
Postoperative analgesia was assessed by a blinded observer using VAS [Citation13]. VAS was recorded after surgery at 1, 2, 4, 6, 8, 12, and 24 h. Patients were evaluated at rest and with passive movement of the operated leg. Postoperatively intravenous paracetamol (1 gm) was administrated every 6 h during the 24 h after surgery (when the VAS score was 4 or more), maximum daily dose: 4 g/day. If VAS >4 persisted for 20 min after paracetamol infusion, meperidine hydrochloride (50 mg) rescue analgesic was given intravenous infusion more than one hour. The duration of effective analgesia was recorded as the time from completion of surgery until the first analgesic dose was required. The analgesic doses (paracetamol and meperidine hydrochloride) required during the first 24 h postoperatively were recorded .Postoperative adverse events as nausea and vomiting, shivering, hyperglycemic episodes (defined as increase in the random blood glucose level >200 mg/dl), or uncontrolled hypertension (defined as increase in the systolic blood pressure >20% from the baseline) were also recorded.
Primary outcome of the study was time to first rescue analgesia and the analgesic doses (paracetamol and meperidine hydrochloride) required during the first 24 h postoperatively, whereas secondary outcomes were the time taken to the onset of sensory analgesia at T10, time to onset of complete motor block, VAS pain score at rest and on movement at 1, 2, 4, 6, 8, 12 and 24 h, and postoperative adverse events as nausea and vomiting, shivering, hyperglycemic episodes or uncontrolled hypertension.
3 Statistical analysis
Data were analyzed using computer statistical software system SPSS® version 15 (Statistical Packages for the Social Sciences, Chicago, IL). Data were presented as mean and standard deviation (SD), median and numbers. Analysis of data between the groups was performed using the Student’s t test for independent samples for parametric data (age, weight, time to T10 sensory level, time to onset of complete motor block, duration of surgery, intraoperative blood loss, intraoperative fluid intake, time to first analgesic requirement, and total dose of analgesic requirement (paracetamol and meperidine hydrochloride), chi square tests for categorical data (sex, ASA physical status, incidence of nausea, and vomiting, shivering, hypotension, bradycardia, use of ephedrine and atropine). Pain scores were analyzed by using the Kruskal–Wallis test. The sample size was calculated using the time to first analgesia requirement as the primary variable. Based on a previous study assuming a 30 min difference with α = 0.05 and power of study = 80%, we calculated a group size of 36 patients would be sufficient to detect the difference [Citation14].
4 Results
Eighty patients scheduled for hip replacement surgery were assessed for randomization 8 patients were excluded, 2 patients had signs of infection of sacral area, 3 patients refused regional anesthesia and 3 patients had abnormal coagulation profile. Seventy-two patients were included in the study (39 female), mean age 72 (7) years old, weight 74 (7), duration of surgery 102 (7) min, with ASA I/II physical status 26/46. There were no significant differences between the two groups with respect to their age, sex, weight, and ASA physical status ().
Table 1 Patients characteristics. Data are presented as mean (SD) for age and weight, while frequency for sex and ASA status.
On adding dexamethasone (8 mg) to bupivacaine there was a significant decrease in the time taken for the onset of sensory analgesia at T10 (p < 0.0001) to be reached with an earlier time to the onset of complete motor block (p < 0.0001). Duration of surgical operation (p = 0.1), intraoperative blood loss (p = 0.8), intraoperative fluid intake (p = 0.6), the incidence of intraoperative hypotension (p = 0.7), bradycardia (p = 0.7), nausea and vomiting (p = 0.7), shivering (p = 0.7) as well as the use of ephedrine (p = 0.7), and atropine (p = 0.7) were not significantly different between groups (). None of the patients needed rescue analgesic or sedative agent administration during the surgery. There was no case of incomplete or patchy caudal block in the study groups.
Table 2 Intraoperative data. Data are presented as mean (SD) for time to T10 sensory level, onset of complete motor block, duration of surgery, fluid intake, and blood loss, while frequency and percentage for use of ephedrine, atropine, incidence of nausea and vomiting, bradycardia, hypotension and shivering.
Postoperative time to first analgesic requirement (P < 0.0001) was significantly longer, with a significant decrease in paracetamol analgesic requirement (p = 0.001), and meperidine rescue analgesia (P < 0.0001) in Group BD than Group BS (). Pain scores were significantly lower in Group BD than BS both at rest and on movement respectively at 4 h (p < 0.0001, and p = 0.0001), 6 h (p = 0.02, and p < 0.0001), 8 h (p = 0.0001, and p = 0.02), 12 h (p = 0.007, and p = 0.03), and 24 h (p = 0.04, and p = 0.04) but did not significantly differ at rest and on movement respectively at 1 h (p = 0.2 and p = 0.5), and 2 h (p = 0.6 and p = 0.3) and .
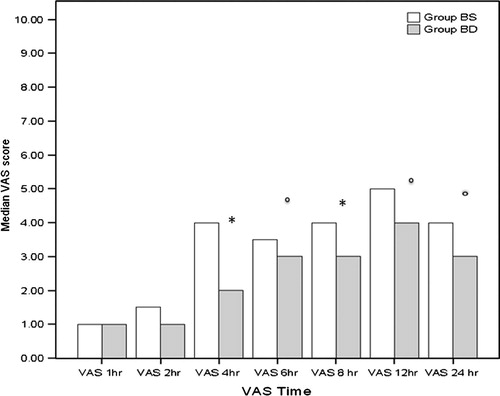
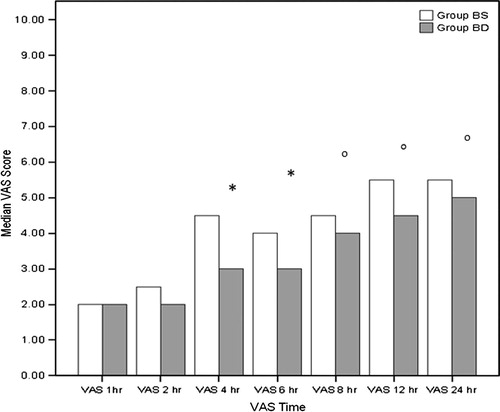
Table 3 Analgesic requirement. Data are presented as mean (SD), for time to first analgesic requirement, Total dose of paracetamol analgesia and total dose of meperidine rescue analgesia.
In the postoperative period there was no significant difference between the groups with respect to the incidence of postoperative nausea and vomiting (p = 0.4) as well as shivering (p = 0.5).Only 4 patients in Group BS and 2 patients in Group BD had nausea and vomiting, whereas 5 patients in Group BS and 3 patients in Group BD had shivering attacks. Mean random blood glucose level was not significantly different (0.1) between Group BS 153 (20) and Group BD 160 (18). No patient in the study groups had any episode of hyperglycemia or hypertension during the study period.
5 Discussion
This study revealed that during ultrasound guided caudal epidural anesthesia, addition of 8 mg dexamethasone to 20 mL 0.25% isobaric bupivacaine is associated with significantly prolonged postoperative analgesia and reduced the postoperative analgesic requirements in geriatric patients undergoing total hip replacement.
Neuraxial regional anesthesia provides anesthesia for hip fracture surgery with less systemic complications and less post-operative nausea and vomiting intraoperative blood loss and thromboembolic complications [Citation15,Citation16]. Caudal epidural block was found to cause effective postoperative analgesia as lumbar epidural anesthesia with increase time to first rescue analgesia than the general anesthesia group [13 (16) h vs 1 (1) h]in total hip replacement surgery [Citation17].
In the current study patients were safely given intravenous ketamine (0.25 mg/kg) and propofol (1 mg/kg) 5 min before positioning in the lateral decubitus with the fractured site up. Intravenous ketamine rapidly crosses the blood–brain barrier because of its high lipid solubility with quick onset of action and rapid recovery (duration of action 5–15 min) [Citation18]. Also co administration of propofol and subdissociative doses of 0.1–0.5 mg/kg ketamine attenuate propofol-induced hypoventilation and provide earlier recovery of cognition without significant difference with respect to VAS and postoperative opioid analgesic requirements [Citation19,Citation20].
Several previous studies reported the excellent long lasting analgesia effect of epidural and spinal steroid [Citation21–Citation23]. During lumbar discectomy the perioperative use of bupivacaine and corticosteroids was reported to cause an effective postoperative analgesia as well as decreased opioid usage without complications [Citation21]. Castill et al. [Citation24] demonstrated incorporation of dexamethasone into bupivacaine microspheres prolonged sciatic nerve blockade in rats compared to bupivacaine microspheres alone.
In our study, the addition of dexamethasone to bupivacaine decreased the time taken to the onset of sensory analgesia at T10, shortened time to onset of complete motor block with a longer time to first analgesic requirement, decreased doses of paracetamol analgesic required, needed meperidine rescue analgesia and VAS score at 4, 6, 8, 12, and 24 h postoperatively. In accordance with our study, Kopacz et al. [Citation25] reported that bupivacaine/dexamethasone microcapsules showed a dose-related effect in onset and duration of intercostal blockade. Also Thomas and Beevi [Citation26] showed the addition of dexamethasone to epidural local anesthetic decreased post-operative pain and analgesic requirements in laparoscopic cholecystectomy.
Corticosteroids induce analgesia through their anti-inflammatory or immune-suppressive effects [Citation27,Citation28]. Steroid actions were achieved through their binding to intracellular receptors and modulating nuclear transcription [Citation14].
In our study adding 8 mg dexamethasone to bupivacaine caudal epidural block was safe in geriatric patient as no patient reported hyperglycemia or uncontrolled hypertension during the study period. In accordance with our study previous studies reported the safety of a single dose and short term (<24 h) use of dexamethasone [Citation29,Citation30].
The current study has potential limitations, though placebo-controlled lacked an active control for systemic steroid effect. Thus, further studies are warranted comparing the effect of IV vs caudal dexamethasone in geriatric patients undergoing total hip replacement surgery. Also this study investigated only a single dose of caudal dexamethasone, and a study comparing different doses of dexamethasone is also warranted.
6 Conclusion
We conclude that adding dexamethasone with isobaric bupivacaine caudal anesthesia prolongs the duration of postoperative analgesia and decreased postoperative analgesic requirement in geriatric patients undergoing total hip replacement surgery in comparison baric bupivacaine alone.
Conflict of interest
There was no conflict of interest, and financial support was provided by institution resources only; no institutional or governmental fund was used.
Notes
Available online 14 February 2014
References
- D.T.SiskFractures of hip and pelvisA.H.CrenshawCampbell’s operative orthopaedics1987CV MosbySt. Louis17191781
- W.J.HallUpdate in geriatricsAnn Inter Med1271997557564
- Y.AuroyM.C.LaxenaireF.ClergueAnesthesiesselonlescaracteristiques des patients, des etablissements et de la procedure associeeAnn Francaisesd’Anesthesie-Reanimation17199813111316
- J.J.BonicaPostoperative painJ.J.BonicaThe management of pain2nd ed.1990Lea & FebigerPhiladelphia461480
- K.T.MuraliN.B.PandaY.K.BatraS.RajeevCombination of low doses of intrathecal Ketamine and midazolam with bupivacaine improves postoperative analgesia in orthopedic surgeryEur J Anesthesiol252008299306
- S.ChakrabortyJ.ChakrabartiD.BhattacharyaIntrathecal tramadol added to bupivacaine as spinal anesthetic increases analgesic effect of the spinal blockade after major gynecological surgeriesIndian J Pharmacol402008180182
- S.C.YuW.D.NganKeeA.S.KwanAddition of meperidine to bupivacaine for spinal anesthesia for cesarean sectionBr J Anesth882002379383
- J.A.AlhashemiA.M.KakiEffect of intrathecal tramadol administration post operative pain after transurethral resection of prostateBr J Anesth912003536540
- M.P.GolwalaV.N.SwadiaA.AditiDhimarN.V.SridbarPain relief by dexamethasone as an adjuvant to local anesthetics in supraclavicular brachial plexus blockJ Anesth Clin Pharmacol252009285288
- P.A.VieiraI.PulaiG.C.TsaoP.ManikantanB.KellerN.R.ConnellyDexamethasone with bupivacaine increases duration of analgesia in ultrasound-guided interscalene brachial plexus blockadeEur J Anaesthesiol272010285288
- C.P.C.ChenS.F.T.TangT.C.HsuUltrasound guidance in cau dal epidural needle placementAnesthesiology1012004181184
- P.R.BromageMechanism of action of extradural analgesiaBr J Anaesth471975199211
- A.GillianHawkerSamraMianTetyanaKendzerskaMelissaFrenchMeasures of adult painArthrit Care Res63S112011 S240-52
- B.NaghipourD.AghamohamadiR.AzarfarinM.MirinazhadE.BilehjaniD.AbbasaliDexamethasone added to bupivacaine prolongs duration of epidural analgesiaMiddle East J Anesthesiol2212013 Feb5357
- M.J.ParkerH.H.HandollR.GriffithsAnaesthesia for hip fracture surgery in adultsCochrane Database Syst Rev8442004 Oct CD000521 Review
- P.BreenK.W.ParkGeneralanaesthesia versus regional anaesthesiaInt Anesthesiol Clin40120026171 Winter
- T.KitaN.MakiY.S.SongF.AraiT.NakaiCaudal epidural anesthesia administered intraoperatively provides for effective postoperative analgesia after total hip arthroplastyJ Clin Anesth192007204208
- Abdullah M. Ketamine: a new look at an old drug. <http://www.painfreeed.com/images/yootheme/painfree/PDF/Pharmacology/K+3.pdf< [accessed 25.03.13].
- N.S.MortonKetamine for procedural sedation and analgesia in pediatric emergency medicine: a UK perspectivePaediatr Anaesth1820082529
- V.DahlP.E.ErnoeT.SteenJ.C.RaederP.F.WhiteDoes ketamine have preemptive effects in women undergoing abdominal hysterectomy procedures?Anesth Analg9062000 Jun14191422
- H.MirzaiI.TekinH.AlincakPerioperative use of corticosteroid and bupivacaine combination in lumbar disc surgery: a randomized controlled trialSpine (Phila Pa 1976)2742002343346 Feb 15
- N.KotaniT.KushikataH.HashimotoF.KimuraM.MuraokaM.YodonoIntrathecal methylprednisolone for intractable postherpeticneuralgiaN Engl J Med34321200015141519 Nov 23
- A.PasqualucciV.PasqualucciF.GallaV.De AngelisV.MarzocchiR.ColussiPrevention of post-herpetic neuralgia: acyclovir and prednisolone versus epidural local anesthetic and methylprednisoloneActa Anaesthesiol Scand4482000 Sep910918
- J.CastillJ.CurleyJ.HotzGlucocorticoids prolong rat sciatic nerve blockade invivo from bupivacaine microspheresAnesthesiology85200211571166
- D.J.KopaczP.G.LacoutureD.WuThe dose response and effects of dexamethasone on bupivacaine microcapsules for intercostal blockade (T9 to T11) in healthy volunteersAnesth Analg962003576582
- S.ThomasS.BeeviEpidural dexamethasone reduces postoperative pain and analgesic requirementsCan J Anaesth5392006 Sep899905
- K.McCormackThe spinal actions of nonsteroidalantiniflammatory drugs and the dissociation between their antiinflammtory and analgesic effectsDrugs4719942845
- S.C.AhlgrenJ.F.WangJ.D.LevineC-fiber mechanical stimulus response functions are different in inflammatory versus neuropathic hyperalgesia in the ratNeuroscience761997285290
- P.TanK.LiuC.H.PengThe effect of dexamethasone on postoperative pain and emesis after intrathecal neostigmineAnesth Analg922001228232
- W.M.SplinterE.J.RhineLow-dose ondansetrone with dexamethasone more effectively decreases vomiting after strabismus surgery in children than does high-does ondansetroneAnesthesiology8819987275
