Abstract
Objective
To assess safety and effectiveness of ultrasound-guided TAP block in children undergoing laparoscopic surgery for undescended testis.
Subjects and methods
This randomized controlled trial involved 108 children, 3–7 years old, randomly allocated into one of two equal groups; TAP Group and Control Group. All children received general anesthesia using propofol 1.5–2.5 mg/kg, atracurium 0.5 mg/kg and fentanyl 2 μg/kg. TAP Group received 0.5 ml/kg of ropivacaine 0.375% bilaterally under ultrasound guidance and control group received regular analgesics. Quality of analgesia was assessed using Children’s Hospital Eastern Ontario Pain Scale (CHEOPS) and Objective behavioral pain score (OPS). The primary outcome measures were hemodynamic parameters and degree of pain. Secondary outcome measures were intraoperative fentanyl requirement, postoperative rescue analgesia (time and dose), complications, hospital stay and degree of satisfaction of patients and their parents.
Results
TAP block group had significantly lower intraoperative fentanyl dose (p < 0.001), significantly longer time to first postoperative request of analgesic (p < 0.001), lower analgesic dose during the first postoperative 24 h (p < 0.001) and lower pain scores along the whole 24 postoperative hours. Mean arterial pressure and heart rate were within the clinically accepted range in the two groups. Parents’ satisfaction was significantly higher (p < 0.001) in the TAP block group.
Conclusion
TAP block under ultrasound guidance was easy, safe, reliable and effective analgesic in children undergoing laparoscopic surgery for undescended testis.
1 Introduction
In recent years an increasing number of pediatric surgical cases are being managed successfully by laparoscopic technique [Citation1]. Although abdominal laparoscopic surgery, a widely performed surgery, is known for less pain compared to that of laparotomy, many patients actually still complain of considerable postoperative pain [Citation2,Citation3].
The benefits of adequate analgesia include a reduction in the stress response of surgery, reduction in the perioperative morbidity and reduction in certain types of surgery improved surgical outcome. Effective pain control can also facilitate rehabilitation and accelerate recovery from surgery [Citation4,Citation5]. Regional anesthesia techniques are commonly advocated for pain control in pediatric surgical practice as they decrease parenteral opioid requirements and improve the quality of postoperative pain control as well as patient-parent satisfaction [Citation6].
A substantial component of the pain experienced by patients after abdominal surgery is derived from the abdominal wall incision. The abdominal wall is innervated by nerve afferents that course through the transversus abdominis neurofascial plane [Citation7]. Abdominal field blocks have been used in anesthesia for surgery involving the anterior abdominal wall for several decades. Many blocks in this area are either difficult or high risk when performed blind, but ultrasound renders them very accessible and safe to perform [Citation8].
The Transversus Abdominis plane (TAP) block was first described in 2004 by McDonnell et al. [Citation9] and ultrasound-guided technique was subsequently popularized by Hebbard et al. [Citation8] TAP block is a regional anesthetic technique that blocks neural afferents of the anterolateral abdominal wall. Using anatomical landmark guidance or with the aid of ultrasound (US), local anesthetic is injected into the transversus abdominis fascial plane, where the nerves from T6 to L1 are located [Citation9].
Randomized controlled trials have demonstrated the efficacy of TAP block in providing postoperative analgesia for up to 24 h after lower abdominal surgery [Citation10–Citation13].
The aim of this study was to compare ultrasound-guided TAP block versus conventional analgesia as regards the degree of pain relief and effect on hemodynamic stability in children undergoing laparoscopic surgery for undescended testis.
2 Subjects and methods
This randomized controlled trial involved children scheduled for laparoscopic surgery for undescended testis in Abu El-Reesh Pediatric Hospital, Cairo University during the period from February 2012 to June 2013. One-hundred and fifty children had laparoscopic procedures during this period; 42 were excluded; 18 refused to participate and 24 had one or more of exclusion criteria. The study included the remaining 108 children. After approval of the study by the local Ethical Committee, parents (or guardians) of all participating children provided an informed consent to share in the study. Participants were 3–7 years old, ASA I-II and were randomized using computer generated table ensuring allocation concealment into one of two groups; group I (TAP Group) and group II (Control Group).
Participants refusing regional block and those having bleeding disorders, skin lesions or wounds at the site of proposed needle insertion, evidence of peritonitis, septicemia and hepatic disease or enlargement in addition to those who required emergency procedures were excluded from the study.
2.1 Anesthesia procedure
EMLA cream was applied to the site of venous puncture 1 h before surgery. After insertion of venous access, all children received premedication in the form of atropine at a dose of 0.01–0.02 mg/kg. Perioperative monitoring included continuous ECG, pulse oximetry, non-invasive arterial blood pressure, capnography and temperature monitoring. Baseline reading (T0) of heart rate, systolic and diastolic blood pressure was recorded after monitor attachment.
General anesthesia was induced using propofol 1.5–2.5 mg/kg over 20–30 s as tolerated, atracurium 0.5 mg/kg to facilitate endotracheal intubation and fentanyl 2 μg/kg. Anesthesia was maintained using isoflurane (1 MAC) and atracurium supplements were given to maintain muscle relaxation.
Participants of TAP group (n = 54) received 0.5 ml/kg of ropivacaine 0.375% bilaterally and those of control group (n = 54) received regular analgesics. The patient was not aware of group allocation as the TAP block was done after induction of anesthesia. An independent anesthesiologist conducted postoperative assessments and was not aware of group allocation.
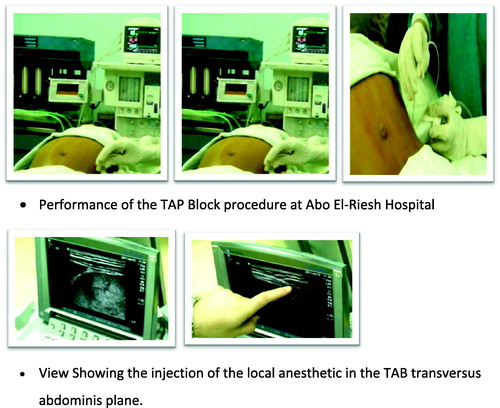
2.2 TAP block procedure: ()
The procedure was done under ultrasound guidance using SonoSite M Turbo (USA) with linear multi-frequency 13–6 MHz transducer (L25x13–6 MHz linear array) scanning probe. Stimuplex D needles (B Braun, Germany) were used.
With the patient in the supine position, the site of the ultrasound and needle entry was sterilized. The TAP block was performed laterally behind the midaxillary line between the iliac crest and the most inferior extent of the ribs. The plane between the internal oblique and transversus abdominis muscle was located around the midaxillary line with the probe transverse to the abdomen. Anteriorly, the Stimpex 35–50 mm needle was passed to come perpendicular to the ultrasound beam and placed between transversus and internal oblique posterior to the midaxillary line. Then, the local anesthetic was injected as a bolus of 0.5 ml/kg ropivacaine 0.375%.
An increase in heart rate and or arterial blood pressure by more than 20% of baseline values in response to surgical stimulus or thereafter throughout the whole operation warranted administration of intravenous fentanyl (0.5 μg/kg). After completion of surgical procedure anesthesia was discontinued, muscle relaxant reversed using atropine 0.02 mg/kg and 0.05 mg/kg of prostigmine and children received diclofenac sodium 1 mg/kg suppository, extubated and transferred to PACU.
The duration of surgery (time from skin incision till extubation) was recorded. Quality of analgesia was assessed immediately postoperatively and then at 2, 4, 8, 12 and 24 h postoperatively using Children’s Hospital Eastern Ontario Pain Scale (CHEOPS) [Citation14] and Objective behavioral pain score (OPS) [Citation15] scores. Proparacetamol (perfalgan) 15 mg/kg IV was given as rescue analgesia for patients if OPS was >5 or CHEOPS score >6.
The CHEOPS is a behavioral scale intended for children ages 1–7. It was originally developed for children in the PACU. It encompasses six indicators (). Children should be observed for 1 min in order to fully assess each indicator. The score ranges from 4 to 13. A score ⩾10 is usually used as an indication to treat pain. However, this should be decided on an individual basis for each patient. In the current study we administered rescue analgesia if the score is above 6 to guard against irritability and agitation.
Table 1 Children’s Hospital Eastern Ontario Pain Scale [Citation16].
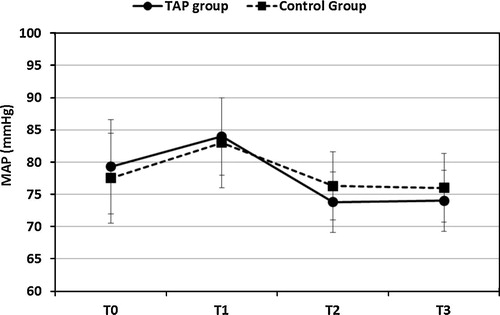
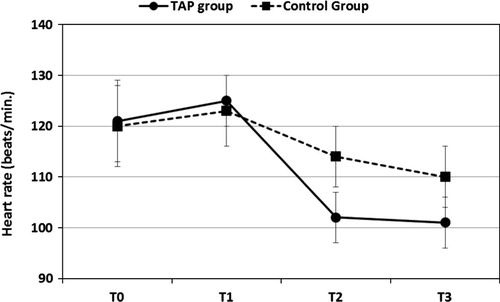
The primary outcome measures were hemodynamic parameters; blood pressure and heart rate measured at: baseline (T0), T1 (after induction of anesthesia and before the block), T2 (15 min after TAP block in group I and after induction in group II), T3 (mean of intraoperative values measured every 15 min) and degree of pain assessed by CHEOPS and OPS scales.
Secondary outcome parameters were intraoperative fentanyl requirement and postoperative need for rescue analgesia and its time and dose, complications (nausea and vomiting, infection or hematoma formation), length of hospital stay and degree of satisfaction of the patients and their parents assessed on a 5-point scale (completely dissatisfied, dissatisfied, not satisfied nor dissatisfied, satisfied or completely satisfied).
2.3 Statistical analysis
Data were analyzed using IBM SPSS Advanced Statistics version 20.0 (SPSS Inc., Chicago, IL). Numerical data were expressed as mean and standard deviation or median and range as appropriate. Qualitative data were expressed as frequency and percentage. Chi-square test (Fisher’s exact test) was used to examine the relation between qualitative variables. For quantitative data, comparison between two groups was done using independent sample t-test or Mann–Whitney test. A p-value <0.05 was considered significant.
3 Results
There was no significant difference between the two studied groups regarding age, weight, ASA physical status ().
Table 2 Baseline demographic and clinical characteristics of the study population.
The total intraoperative fentanyl dose was significantly lower in TAP block group (p < 0.001). Postoperatively, the time to first request of analgesic was significantly longer in TAP block group (p < 0.001) and the total paracetamol dose during the first 24 h was significantly lower in the TAP block group (p < 0.001). However, the duration of hospital stay was comparable between the two groups (). shows that pain scores were significantly lower in the TAP block along the whole 24 postoperative hours.
Table 3 Intraoperative and postoperative findings in the two studied groups.
Table 4 Postoperative pain scores in the two studied groups.
and show that the mean arterial pressure (MAP) and heart rate (HR) were comparable at baseline reading and immediately after induction. Then both become statistically significantly lower in the TAP block group 15 min after induction and intraoperatively. However, the differences between the two groups were always clinically insignificant. Also, in each group statistically significant changes in MAP and HR were noticed, however, all changes were within the clinically accepted range. Parents’ satisfaction was significantly higher (p < 0.001) in the TAP block group ().
Table 5 Degree of satisfaction of the parents in the two studied group.
4 Discussion
The results of the present randomized study demonstrated that bilateral TAP block provides an additional benefit to multimodal analgesia in children undergoing abdominal laparoscopic surgery. The children who received TAP block required less intraoperative as well as postoperative analgesia, with preserved hemodynamic stability and a good degree of parents’ satisfaction.
We found a statistically significant lower intraoperative fentanyl doses in children under TAP block (p < 0.001). This is consistent with the results of Fredrickson et al. in a prospective audit of the TAP block in 8 patients undergoing inguinal hernia repair; 5 of 8 children required no intraoperative opioid supplementation [Citation17]. In a double-blind trial of 40 children undergoing emergency open appendectomy, Carney et al. [Citation18] reported 50% reduction in postoperative morphine requirement. Jacobs et al. [Citation19] reported opioid sparing in a group of 10 children undergoing different abdominal procedures. This was also reported in many case reports and series in neonates and young children [Citation20–Citation25]. Similar results were reported in adults [Citation26,Citation7,Citation27,Citation28].
Conflicting results to ours were also reported. Sandeman et al. [Citation29] performed ultrasound-guided bilateral TAP blocks in a group of children older than the current study (7–16 years) undergoing laparoscopic appendectomy. Contrary to the current study, authors reported no difference in the proportion of patients requiring postoperative morphine compared to control group. However, in their study, cases of complicated appendicitis were more frequent and duration of surgery was significantly longer in the TAP block group. Nevertheless, pain control was superior in the TAP block group in the immediate postoperative period.
Fredrickson et al. [Citation30] compared TAP block with ilioinguinal blocks in children undergoing elective inguinal surgery. They found a higher proportion of children reporting pain in the recovery unit in the TAP block group. The lower operative site may explain the difference with the current study; spread of local anesthetic to the genital branch of the genitofemoral nerve seems more probable in cases of ilioinguinal block.
In our study, there were no complications during the procedure or after the block especially with the direct visualization of the neurofascial plane and real time injection of the local anesthetic under ultrasound guidance. Laghari and Harmon [Citation31] first described the use of ultrasound in TAP block of a pediatric patient undergoing an appendectomy. Moreover, Fredrickson et al. [Citation17] and Hebbard et al. [Citation8] confirmed the value of direct ultrasound imaging with good results in children undergoing inguinal herniorrhaphies.
The adverse effects pertaining to the TAP block have been reported in the literature. Farooq and Carey reported a case of liver trauma with a blunt regional anesthesia needle while performing a TAP block. But they carried out the block solely using the blind “double-pop” technique, so they could not evaluate the anatomical structures and the exact location of the needle tip [Citation32].
Two potential limitations should be considered. First, the study limited assessment of postoperative analgesia to the first 24 postoperative hours. However, the TAP block has been demonstrated to produce clinically useful levels of analgesia for at least 48 h postoperatively. Second, there are difficulties in adequately blinding studies such as these, given that the TAP block produces loss of sensation of the abdominal wall. However, neither the patient nor the anesthesiologist conducting postoperative assessments was aware of the group allocation. The patient’s abdomen was not examined during these assessments, and the TAP block sites were covered by dressings in all patients.
We can conclude that the use of ultrasound for the placement of peripheral nerve blocks has proved efficacy and is beginning to solidify a place in clinical practice. The TAP block under ultrasound guidance, was easy to perform and provided reliable and effective analgesia in children undergoing laparoscopic surgery for undescended testis. It was hemodynamically safe with no recorded intra- or postoperative complications.
Conflict of interest
We did not face any conflict of interest.
Notes
Available online 12 February 2014
References
- V.GuptaS.K.YadavE.DeanP.VincentF.WalidA.Al SaidPaediatric laparoscopic orchidopexy as a novel mentorship: training modelAfr J Paediatr Surg1022013117121
- M.BarczynskiR.M.HermanA prospective randomized trial on comparison of low-pressure (LP) and standard-pressure (SP) pneumoperitonium for laparoscopic cholecystectomySurg Endosc172003533538
- V.L.WillsD.R.HuntPain after laparoscopic cholecystectomyBrit J Surg872000273284
- H.KehletSurgical stress: the role of pain and analgesiaBrit J Anaesth631989189195
- X.CapdevillaY.bartheletP.BibouletEffects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgeryAnesthesiology911999815
- H.KehletK.HolteEffect of postoperative analgesia on surgical outcomeBrit J Anaesth8720016272
- J.G.McDonnellB.O’DonnellG.CurleyA.HeffernanC.PowerJ.G.LaffeyThe analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trialAnesth Analg1042007193197
- P.HebbardY.FujiwaraY.ShibataC.RoyseUltrasound guided transversus abdominis plane (TAP) blockAnaesth Intensive Care352007616617
- J.G.McDonnellB.D.O’DonnellD.TuiteT.FarrellC.PowerThe regional abdominal field infiltration (R.A.F.I.) technique: computerized tomographic and anatomical identification of a novel approach to the transversus abdominis neurovascular fascial planeAnesthesiology012004A899
- P.L.PetersenO.MathiesenH.TorupJ.B.DahlThe transverses abdominis plane block: a valuable option for postoperative analgesia? A topical reviewActa Anaesthesiol Scand542010529535
- N.BhartiP.KumarI.BalaV.GuptaThe efficacy of a novel approach to transversus abdominis plane block for postoperative analgesia after colorectal surgeryAnesth Analg112201115041508
- M.R.SiddiquiM.S.SajidD.R.UnclesL.CheekM.K.BaigA meta-analysis on the clinical effectiveness of transversus abdominis plane blockJ Clin Anesth232011714
- Y.S.RaC.H.KimG.Y.LeeJ.I.HanThe analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomyKorean J Anesthesiol582010362368
- K.L.CassidyG.T.ReidP.J.Mc GrathA randomized trial if emla patch for reduction of pain associated with intramuscular injections in 4–6 years old childrenActa Pediatr90200113291336
- American Academy of PediatricsCommittee on psychological aspects of child and family health; task force on pain in infants, children and adolescents. The assessment and management of pain in infants, children and adolescentsPediatrics10832001793797
- P.J.McGrathG.JohnsonCHEOPS: a behavioral scale for rating postoperative pain in childrenAdv Pain Res Ther91985395402
- M.FredricksonP.SealJ.HoughtonEarly experience with the transversus abdominis plane block in childrenPaediatr Anaesth182008891892
- J.CarneyO.FinnertyJ.RaufIpsilateral transversus abdominis plane block provides effective analgesia after appendectomy in children: a randomized controlled trialAnesth Analg11120109981003
- A.JacobsE.BergmansG.S.ArulThe transversus abdominis plane (TAP) block in neonates and infants – results of an auditPediatr Anesth21201110781080
- M.J.FredricksonP.SealUltrasound-guided transversus abdominis plane block for neonatal abdominal surgeryAnaesth Intensive Care372009469472
- L.J.TaylorP.BirminghamE.YerkesChildren with spinal dysraphism: transversus abdominis plane (TAP) catheters to the rescuePediatr Anesth202010951954
- C.A.HardyTransverse abdominis plane block in neonates: is it a good alternative to caudal anesthesia for postoperative analgesia following abdominal surgery?Pediatr Anesth19200956
- M.TekinY.GurkanM.SolakUltrasound-guided bilateral transversus abdominis plane block in a 2-month-old infantJ Anesth232009643644
- D.M.SimpsonJ.TyrrellJ.De RuiterUse of ultrasound-guided subcostal transversus abdominis plane blocks in a pediatric patient with chronic abdominal wall painPediatr Anesth2120118890
- M.VisoiuK.BoretskyG.GoyalPostoperative analgesia via transversus abdominis plane (TAP) catheter for small weight children-our initial experiencePediatr Anesth222012281284
- P.MarhoferA.El DawlatlyA.TurkistaniUltrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomyBJA1022009763767
- J.G.McDonnellJ.G.LaffeyG.CurleyThe analgesic efficacy of TAP block after Cesarean delivery: a randomized controlled trialAnesth Analg1062008186191
- J.CarneyJ.G.McDonnellJ.G.LaffeyThe TAP block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomyAnesth Analg107200820562060
- D.J.SandemanM.BennettA.V.DilleyUltrasound-guided transversus abdominis plane blocks for laparoscopic appendicectomy in children: a prospective randomized trialBrit J Anaesth1062011882886
- M.J.FredricksonC.PaineJ.HamillImproved analgesia with the ilioinguinal block compared to the transversus abdominis plane block after pediatric inguinal surgery: a prospective randomized trialPediatr Anesth20201010221027
- Z.A.LaghariD.HarmonUltrasound-guided transabdominus plane blockJ Clin Anesth202008156158
- M.FarooqM.CareyA case of liver trauma with blunt regional anesthesia needle while performing TAP blockReg Anesth Pain Med342008274277