Abstract
Background
Statins anti-inflammatory and antioxidant properties improve vascular function in septic patients. The aim of this prospective study was to assess vasopressor effect and safety of rosuvastatin therapy in septic patient.
Methods
One hundred and eight patients admitted to intensive care unit (ICU) with suspected or confirmed infection plus at least 2 systemic inflammatory response syndrome criteria were included in this prospective double-blinded randomized two groups’ parallel study. Group R received standard therapy and rosuvastatin 20 mg/day and Group C received standard therapy with placebo/day for 14 days.
The primary endpoint was number of acceptable blood pressure and systemic perfusion days (ABPSPD). Secondary outcome included time to initial ABPSPD, vasopressor dose and duration, arterial lactate, organ dysfunction or failure free days, ICU and hospital stay, 28 ICU and hospital mortality, CPK and transaminases level.
Results
The number of ABPSPD was significantly increased 11(3) vs. 8 (3) (p = 0.0001), with a shorter time to initial ABPSPD 18(21) vs. 41(37) h (p = 0.0001) in Group R than Group C. Norepinephrine dose 0.8 (0.5) vs. 1.6 (0.6) and duration 3(2) vs. 6(3) were significantly reduced in Group R with no significant elevation in transaminases or CPK.
Conclusions
Rosuvastatin 20 mg/day in septic patients increased number ABPSPD, decreased time to initial ABPSPD, norepinephrine dose and duration, with no significant elevation in transaminases or CPK.
1 Introduction
Microvascular circulation and endothelial cell dysfunction is the core pathogenesis of sepsis [Citation1]. Induction of inflammatory cytokines decreases the vascular tone, and causes severe hypotension, inadequate organ perfusion, multiple organ dysfunction and failure [Citation2,Citation3]. Vasopressors are used to increase blood pressure and improve tissue perfusion. However, in sepsis the decreased reactivity to exogenously administered catecholamine [Citation4] limits improvement in hypoperfusion. Studies have demonstrated that the vascular effect of statins was independent of lipid lowering effect and the anti-inflammatory and antioxidant properties [Citation5,Citation6] caused the improvement in vascular function.
The aim of this prospective study was to assess vasopressor effect and safety of rosuvastatin therapy in septic patient.
2 Methods
The protocol was approved by our institution medical board and patients’ guardian or next of kin gave informed written consent. One hundred and eight patients who met the inclusion criteria: age >18 years old, of both sexes, with the presence of clinically suspected or confirmed infection plus at least two of the systemic inflammatory response syndrome criteria (temperature < 38 °C or <36 °C, heart rate >90 beats/min, respiratory rate >20 breaths/min or arterial Pco2 < 32 mmHg, WBC count < 12,000/mm3 or <4000/mm3 or >10% immature forms) with organ dysfunction, hypoperfusion or hypotension, and initiated appropriate antimicrobial therapy admitted to Intensive Care Unit Ain Shams University Hospital during the period of May 2011 to May 2012 were assigned randomly using computerized program in this randomized prospective double blinded study to one of the two parallel groups (Control group n = 54 patients and 54 patients in Rosuvastatin group). Patients were randomly assigned after admission to the ICU by opening sequentially numbered opaque envelopes. Exclusion criteria were as follows: pregnancy, A severe moribund state, an anticipated ICU stay of less than 24 h, serum creatine kinase (CPK) < 5 times the upper limit of normal range, liver transaminases (AST and ALT) < 3 times the upper limit of normal range, contraindication to enteral nutrition, chronic renal failure, treatment of statins within the previous 30 days, high risk of rhabdomyolysis (multiple trauma, extensive burn and crush injuries), serum creatine < 2 mg/dl allergy to statins and concurrent treatment with anticoagulants as warfarin, cimetidine, ketoconazole, cyclosporine, clofibrate, fenofibrate, gemfibrozil, niacin, or specific HIV protease inhibitors.
All patients received standard protocol of Intensive Care Unit management in Ain Shams University Hospital using early goal directed therapy of sepsis. Patients were given intravenous fluids resuscitation, antimicrobials, stress ulcer prophylaxis (proton pump inhibitor), enteral nutrition, analgesic, antipyretics, and prophylactic low molecular weight heparin. Severe sepsis and septic shock were defined according to the American College of Chest Physicians/Society for Critical Care Medicine Consensus Conference on sepsis and organ failure [Citation7]. Severe sepsis was defined as sepsis associated with organ dysfunction, hypoperfusion or hypotension (hypoperfusion abnormalities as lactic acidosis, oliguria or an acute alteration in mental status), whereas septic shock was defined as sepsis-induced hypotension MABP < 65 mmHg despite adequate fluid resuscitation associated with hypoperfusion abnormalities or organ dysfunction (oliguria < 0.5 ml/kg/h for >2 h, lactic acidosis, and alteration in mental status).
Norepinephrine was started at 0.5–1 mcg/kg/min and titrated to maximum dose: 5 mcg/kg/min till mean arterial blood pressure ⩾65 mmHg. The norepinephrine infusion rate was adjusted by the nursing staff blinded to the study groups (at least every hour) to the minimal dose necessary to maintain mean arterial blood pressure ⩾65 mmHg [Citation8].
The study group (Group R) received the standard protocol therapy and rosuvastatin 20 mg/day starting from the onset of the diagnosis of sepsis for 14 days whereas, the control group (Group C) received only the standard protocol therapy with identically appearing placebo preparation tablet that resembles the statin/day starting from the onset of the diagnosis of sepsis for 14 days as well.
For all patients general characteristics were recorded; Age, gender, body mass index, severity of illness on APACHE II score, and SOFA scores (recorded once daily), cause of admission (medical or surgical), origin of sepsis and causative organism, need for mechanical ventilation on admission. Arterial lactate concentrations and blood gases were recorded twice daily. Results of routine laboratory tests, blood cultures, and cultures of specimen sampled from site of infection were also recorded.
During the study period careful neurological and cardiac examinations were conducted daily for all patients. Routine ECG, continuous invasive blood pressure, SPO2, as well as hourly CVP, and UOP were also monitored. Central venous blood gas sampling was done to monitor oxygenation as indicated to achieve the early goal directed therapy. Patients were mechanically ventilated if they met the criteria of mechanical ventilation and weaned upon improvement according to protocols.
Norepinephrine dose and duration were recorded. Any suspected side effects of statins were assessed and recorded by measuring daily serum aminotransferase (ALT and AST) and CPK levels. Statin therapy was stopped if the patient suffered intolerance as vomiting, aminotransferase elevation more than three times the upper normal level, or increase in serum CPK above five times the upper normal level and restarted after resolution.
The primary endpoint was the number of days with acceptable blood pressure and systemic perfusion (ABPSPD) up to 14 day. The ABPSPD defined as a mean arterial pressure (MAP) ⩾ 65 mmHg, urine output < 2 ml/kg/h, and central venous oxygen saturation (ScvO2) ⩾ 70%, with no increase in the infusion of vasopressors or inotropic therapy maintained for four hours.
Secondary outcome included time taken to achieve initial ABPSPD, the dose and duration of vasopressor infused for 14 days, arterial lactate ,the number of organ dysfunction-free, and organ failure free days as assessed by SOFA score up to day 14, ICU length of stay, length of hospital stay, and twenty-eight ICU mortality or hospital mortality.
Evaluation of safety of rosuvastatin was assessed as elevation of serum CPK above five times the upper normal level and transaminases level above three times the upper normal level for the study period.
Organ dysfunction and organ failure were defined by a Sequential Organ Failure Assessment (SOFA) score above one and above two, respectively [Citation8]. Organ failure or dysfunction -free days were defined as the number of days between ICU admission (day 1) and day 14 with the patient alive without any organ failure. In case of ICU death before day 14, organ failure-free days were considered equal to zero. Patients discharged from ICU before day 14 were considered free from organ failure after ICU discharge.
3 Statistical analysis
Statistical analysis was performed using SPSS version 15.0 package (SPSS Inc, Chicago, IL, USA). Data were expressed as Mean (SD) for quantitative parametric measures and comparison done using independent t-test. Categorical data were expressed as both number and percentage and compared using the Chi-square test or exact Fisher test. Quantitative variables are reported as median and compared using the nonparametric Mann–Whitney test. Logistic regression analysis was done to adjust for other covariates that may affect the outcome such as age, APACHE II score, sex, body mass index, type of patients, SOFA score, sepsis characteristics ,need for mechanical ventilation on admission. A P value less than 0.05 was considered significant, whereas P value less than 0.0001 was considered significant highly significant. A sample size of 98 patients (49 patients per group) was estimated at a power of study = 80% and α = 0.05, using Power and Sample size calculation 2.1.31 program (PS). A pilot study of 10 patients was carried out. A mean difference of 2 with SD 3.5 for the number of days with acceptable blood pressure and systemic perfusion (ABPSPD) was considered for calculation of sample size. 10% was added to the sample to cover for dropouts.
4 Results
One hundred and thirty-five patients admitted to Intensive Care Unit Ain Shams University Hospital during the study period was assessed for randomization, 4 patients were less than 18 years, 5 patients were multiple trauma patients and 2 patients suffered crushed injuries, 5 patients suffered elevations in liver enzymes more than 3 times due to a hepatic disease, 3 patients had a chronic kidney disease on hemodialysis, and 3 patients were admitted with acute abdomen which contraindicated enteral feeding, 3 patients were already on current treatment with statins, the serum creatine was more than 2 mg/dl in 2 patients. In the study group consisting of 108 patients there was a male predominance 59%, mean age 36 (9), body mass index 27 (4), median APACHEII score 25, SOFA score 9. Fifty-two percent of patients were defined as severe sepsis and 47% defined as septic shock. The study group included 54 patients in the rosuvastatin group (Group R) and 54 in the control group (Group C). There was no significant difference within the groups regarding the patient characteristics, sepsis characteristics and demographic data (). Logistic regression analysis was done to adjust for other covariates that may affect the outcome between groups, age (p = 0.5), APACHE II score (p = 0.3), sex (p = 0.6), body mass index (p = 0.1), type of patients (p = 0.1), SOFA score (p = 0.3), sepsis characteristics (p = 0.5), origin of sepsis (p = 0.3), causative organism (p = 0.2), and need for mechanical ventilation on admission (p = 0.2).
Table 1 Patients characteristics, sepsis characteristics and demographic data. Mean (SD) for age and body mass index, median and mean rank APACHE II score, and SOFA score, number and percentage for sex, Origin of sepsis , type of infection, causative organism, and need for mechanical ventilation on admission.
The number of days with acceptable blood pressure and systemic perfusion (ABPSPD) was significantly higher (p = 0.0001) in Group R 11(3) than Group C 8 (3) (), with a significantly shorter time to reach acceptable blood pressure and systemic perfusion in Group R than Group C (p = 0.0001) (), and significantly increase in the number of organ dysfunction-free days 8(3) vs. 4 (3) (p = 0.0001), and organ failure free days 10(3) vs. 6(3) (p = 0.0001) in Group R than Group C ( and ). Norepinephrine dose (ug/kg/min) (p = 0.0001) and duration (p = 0.0001), arterial lactate level (p = 0.0001), number of patients requiring mechanical ventilation (p = 0.02) and the duration of mechanical ventilation (p = 0.0001) were significantly less in Group R than Group C. There was a decrease in length of ICU stay, ICU mortality, in hospital stay, and hospital mortality within both groups, but did not reach statistical significance (, ).
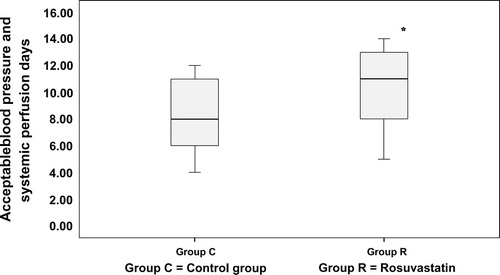
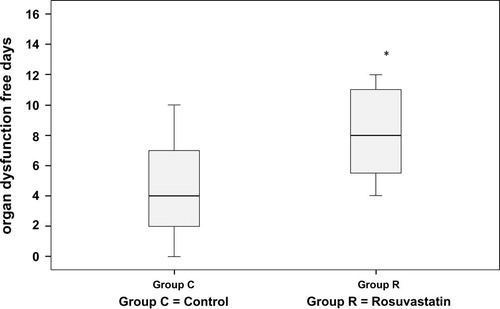
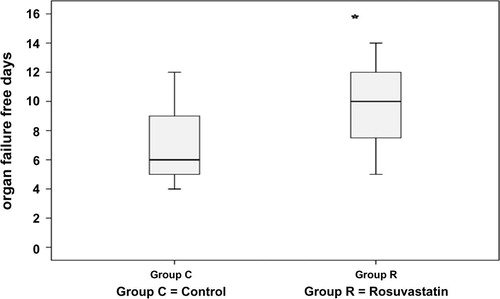
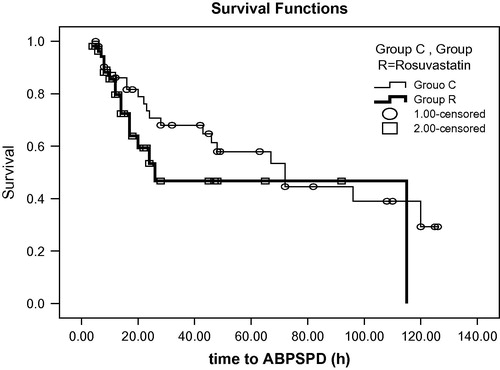
Table 2 Outcome parameters; mean (SD) for time to initial stabilization norepinephrine doses, norepinephrine duration, arterial lactate, duration of invasive mechanical ventilation, ICU length of stay and hospital length of stay. While frequency and percentages for invasive mechanical ventilation, ICU mortality and Hospital mortality.
Treatment with rosuvastatin 20 mg for 14 days was safe as the number of patients with significant elevation in either serum CPK and/or transaminases level (ALT and AST) was not significantly different in Group R than Group C during the study period ().
Table 3 Safety parameters; number and percentage for serum creatine phosphokinase and serum transaminases.
5 Discussion
In this study we investigated the effect of Rosuvastatin 20 mg/day starting from the onset of the diagnosis of sepsis for 14 days. There was an increased number of days with acceptable blood pressure and systemic perfusion (ABPSPD) accompanied by a shorter time to reach ABPSPD , smaller doses and shorter duration of norepinephrine used in Group R than Group C.
In sepsis the cardiovascular disturbance and multisystem organ failure is caused by endotoxins and cytokines [Citation2,Citation3]. This hypotensive response occurs in the later stage of sepsis due to failure of endothelial mechanism controlling vascular smooth muscle contractility [Citation9–Citation11].
Vascular endothelial dysfunction in sepsis is associated with loss of endothelial nitric oxide synthase (e NOS) which is important for maintaining normal endothelial cell surface [Citation12,Citation13]. The balance between e NOS and inducible nitric oxide synthase (i NOS) has been studied and demonstrated that cytokines had a stimulatory effect on i NOS expression causing excessive vasodilatation with a suppression effect on e NOS activity [Citation13].
In vitro studies proved simvastatin and lovastatin increased the half-life of e NOS under normal or low cholesterol level [Citation14,Citation15]. Also, in vivo experimental studies showed hydrophilic rosuvastatin upregulated e NOS expression independent of cholesterol level with a protective effect that is equal or superior to simvastatin and atorvastatin [Citation16].
Several studies investigated the vasopressor effect of statins. Johannes et al. [Citation17] demonstrated the vaso-protective properties of simvastatin 8 mg in endotoxemia associated with decreased vascular reactivity. Giusti-Paiva et al. determined pretreatment with simvastatin increased endothelial response to phenylephrine [Citation18]. McGown et al. [Citation19] reported improved nitric oxide synthase mediated vessel relaxation by pravastatin with microvascular anti-inflammatory effect which was protective against sepsis induced hypotension in rats. The protective effects of statins were evaluated by several studies showing conflicting results, Almog et al. reported the protective effect of prior statin therapy against severe sepsis [Citation20]. In contrast Doson Chua et al. [Citation21] found no difference between statin and non-statin users in septic shock patients (mean duration of vasopressor support 233 ± 94 h vs. 120 ± 20 h), and this may be due to the retrospective nature of their study as statin users had higher incidence of comorbidities. Also Kruger et al. the use of atorvastatin was not effective on either suppression of inflammatory mediator, improvement in organ dysfunction, SOFA score or mortality, this may be due to the difference in study design as well as some patients included in the study were on statins prior to the study and continued on were this group was found to show improved survival [Citation22].
In the current study rosuvastatin group showed significantly lower lactate and lower dose and duration of norepinephrine than Group C which might be due to better tissue perfusion as lactate is strongly associated with hypoperfusion state and MABP □ 65 mmHg [Citation23]. Moreover, there was a significant decrease in the incidence and duration of invasive mechanical ventilation in Group R. In accordance with our study Fuller et al. [Citation24] reported fewer mechanical ventilation days in patients with prior statin use than non-statin users (7.92 vs. 8.49 days, P = 0.0026).
Interventions that shorten ventilation days might eliminate the risk associated with prolonged intubation and ventilation; but, our study fails to show significant differences in ICU length of stay, ICU mortality, hospital mortality and hospital length of stay between the groups. This may be due to complex pathophysiology of sepsis and the prolonged ICU course making the interpretation of the results difficult. These results were supported by Doson Chua et al. [Citation21] who also failed to demonstrate difference in ICU and hospital mortality. Whereas Fernandez et al. [Citation25] showed higher hospital mortality in mechanically ventilated patients receiving statin therapy. The lack of statin benefit in their study might be related to the differences in patient’s comorbidities, severity of illness, or type and dose of statin. In contrast other studies associated statin use with decreased mortality in hospitalized infected or septic patients. [Citation26,Citation27].
Evaluation of safety of rosuvastatin was assessed using elevation of serum CPK and transaminases during the study period, and the number of patients with elevation in transaminases and CPK level was not significantly different between groups. In accordance with our results Terblanch et al. [Citation28] found that the statin groups were not associated with liver cell failure and ALT was not markedly increased. Also Harris et al. [Citation29] reported muscle pain without elevation of serum CPK in about 10% of cases on long standing statin therapy.
The current study has potential limitations though placebo-controlled study in septic patients, lacked comparison with other statins, and measurement of rosuvastatin level and further study is warranted comparing other statins with different doses to evaluate the safe vasopressor effect of statins in septic patients as well as measurement of statin level.
We conclude that rosuvastatin 20 mg/day in septic patients increased number of days with acceptable blood pressure and systemic perfusion (ABPSPD), decreased time to initial ABPSPD, norepinephrine dose and duration, with no significant elevation in transaminases or CPK.
Conflict of interest
None.
Notes
Available online 19 March 2014
References
- C.C.McGownZ.L.S.BrookesBeneficial effects of statins on the microcirculation during sepsis: the role of nitric oxideBr J Anaesth982007163175
- B.B.TanR.L.PrewittL.D.BrittInterleukin-10 prevents loss of rat skeletal muscle arterioles exposed to endotoxinJ Surg Res1002001110115
- J.L.VincentCardiovascular alterations in septic shockJ Antimicrob Chemother411998915
- R.J.BealeS.M.HollenbergJ.L.VincentJ.E.ParrilloVasopressor and inotropic support in septic shock: an evidence based reviewCrit Care Med3211 suppl.2004S455S465
- D.PrueferJ.MakowskiM.SchnellU.BuerkeM.DahmH.OelertSimvastatin inhibits inflammatory properties of Staphylococcus aureus alpha-toxinCirculation106200221042110
- Y.RikitakeS.KawashimaS.TakeshitaT.YamashitaH.AzumiM.YasuharaAnti-oxidative properties of fluvastatin, an HMG-CoA reductase inhibitor, contribute to prevention of atherosclerosis in cholesterol-fed rabbitsAtherosclerosis15420018796
- R.C.BoneR.A.BalkF.B.CerraACCP/SCCM consensus conference. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsisCrit Care Med201992964974
- X.ViviandM.LeoneX.ThirionEffect of norepinephrine on the outcome of septic shockCrit Care Med2882000
- T.M.GlembotL.D.BrittM.A.HillLack of direct endotoxin induced vasoactive effects on isolated skeletal muscle arteriolesShock31995216223
- T.M.GlembotL.D.BrittM.A.HillEndotoxin interacts with tumour necrosis factor-alpha to induce vasodilation of isolated rat skeletal muscle arteriolesShock51996251257
- R.ScaliaT.J.StalkerMicrocirculation as a target for the anti-inflammatory properties of statinsMicrocirculation92002431442
- P.A.VoB.LadJ.A.TomlinsonS.FrancisA.AhluwaliaAutoregulatory role of endothelium-derived nitric oxide (NO) on lipopolysaccharide-induced vascular inducible NO synthase expression and functionJ Biol Chem280200572367243
- T.YamashitaS.KawashimaY.OhashiResistance to endotoxin shock in transgenic mice over expressing endothelial nitric oxide synthaseCirculation1012000931937
- U.LaufsV.L.FataJ.K.LiaoInhibition of 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase blocks hypoxia mediated down-regulation of endothelial nitric oxide synthaseJ Biol Chem27219973172531729
- U.LaufsV.La FataJ.PlutzkyJ.K.LiaoUpregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitorsCirculation97199811291135
- U.LaufsK.GertzU.DirnaglM.BohmG.NickenigM.EndresRosuvastatin, a new HMG-CoA reductase inhibitor, upregulates endothelial nitric oxide synthase and protects from ischemic stroke in miceBrain Res94220022330
- MarsikPolterauerStefanKapiotisStylianosPleiner Michael WolztJohannesSchallerGeorgMittermayerFriedrichSimvastatin prevents vascular hyporeactivity during inflammationCirculation110200433493354
- A.Giusti-PaivaM.R.MartinezJ.V.FelixSimvastatin decreases nitric oxide overproduction and reverts the impaired vascular responsiveness induced by endotoxic shock in ratsShock212004271275
- C.C.McGownN.J.BrownP.G.HellewellBeneficial microvascular and anti-inflammatory effects of pravastatin during sepsis involve nitric oxide synthase IIIBr J Anaesth10422010183190
- Almog Y, shefer A, Novack V, et al. Prior statin therapy protects against severe sepsis. Presented at: annual meeting of the Society of Critical Care Medicine; Orlando, Fla Circulation 2004; 110(7): 880–5.
- DosonChuaKarinaChoiceRochelleGellatlyGlenBrownStatin use and morbidity outcomes in septic shock patients: a retrospective cohort studyCrit Care Shock1420111518
- P.KrugerM.BaileyR.BellomoD.J.CooperM.HarwardA.HigginsA multicenter randomized trial of atorvastatin therapy in intensive care patients with severe sepsisAm J Respir Crit Care Med1877201374375010.1164/rccm.201209-1718OC
- E.RiversB.NguyenS.HavstadEarly goal- directed therapy collaborative group. Early goal-directed therapy in the treatment of severe sepsis and septic shockN Engl J Med34519200113681377
- B.M.FullerM.GajeraC.SchorrThe association of prior statin use in septic shock treated with early goal directed therapyEur J Emerg Med1942012226230
- R.FernandezV.J.De PedroA.ArtigasStatin therapy prior to ICU admission: protection against infection or a severity marker?Intens Care Med322006160164
- E.M.MortensenM.I.RestrepoL.A.CopelandImpact on previous statin and angiotensin II receptor blocker use on mortality in patients hospitalized with sepsisPharmacotherapy2712200716191626
- M.W.DonninoM.N.CocchiM.HowellStatin therapy is associated with decreased mortality in patients with infectionAcad Emerg Med162009230234
- M.J.TerblancheR.PintoC.WhiteleyStatins do not prevent acute organ failure in ventilated ICU patients: single-centre retrospective cohort studyCrit Care151201174
- L.J.HarrisR.ThapaM.BrownClinical and laboratory phenotype of patients experiencing statin intolerance attributable to myalgiaJ Clin Lipidol542011299307
