Abstract
Objective
The aim was to test the effect of amantadine, an NMDA antagonist, on tourniquet induced cardiovascular responses under general anesthesia.
Method
In a randomized, double blind, placebo-controlled study; thirty adult male patients with ASA physical status I or II, aged 18–50 years underwent anterior cruciate ligament reconstruction with a tourniquet under general anesthesia, were divided to receive either oral amantadine 200 mg capsule in the evening before surgery and 200 mg capsule 60 min before surgery (group A) or placebo capsules (group P). Heart rate, systolic and diastolic blood pressures were recorded (before induction of anesthesia, every 15 min after tourniquet inflation, before tourniquet deflation, and 10 min after tourniquet deflation). Incidence of tourniquet-induced hypertension, and postoperative tramadol consumption were also recorded.
Results
Systolic and diastolic pressures significantly increased in both groups compared to baseline values (P < 0.05) at 15, 30, 45, 60, 75 min after tourniquet inflation, and before tourniquet deflation with significantly lesser increase with amantadine compared to placebo at 45, 60, and 75 min after tourniquet inflation (P < 0.05). Heart rate significantly increased at 45, 60, and 75 min after tourniquet inflation in both groups compared to baseline values (P < 0.05) with significantly lesser increase with amantadine compared to placebo (P < 0.05). Development of tourniquet induced hypertension was less with amantadine (5 out of 15) than with placebo (8 out of 15).The total tramadol consumed during the first 24 h postoperative was significantly less with amantadine compared to placebo (P < 0.05).
Conclusion
Preoperative oral amantadine reduced tourniquet induced hypertension and postoperative analgesic requirements in anterior cruciate ligament reconstruction surgery under general anesthesia.
1 Introduction
Pneumatic tourniquets are widely used during the upper or lower limbs orthopedic surgery to provide bloodless surgical field. However, the associated pain and increase in the arterial blood pressure are frequently observed 30–60 min after tourniquet inflation in spite of adequate level of anesthesia and they are often resistant to profound depth of anesthesia and analgesic drugs [Citation1]. Tourniquet induced hypertension occurs more frequent under general anesthesia than spinal anesthesia and more with lower limb tourniquet than with upper limb tourniquet and can be serious in patients with cardiovascular diseases, neurological diseases, or glaucoma. The exact mechanism of its development is still unclear [Citation2].
Several methods were used to attenuate tourniquet pain and hypertension intra-operatively such as the use of regional anesthesia, intravenous (IV) opioids (remifentanil) [Citation3], α2 agonists (clonidine and dexmedetomidine) [Citation4,Citation5].
There are several attempts to use N-methyl-D-aspartate (NMDA) receptor antagonists (Ketamine, magnesium, and dextromethorphan) to attenuate tourniquet-induced pain and hypertension and have reported to be effective [Citation1,Citation2,Citation4,Citation6,Citation7].
Amantadine (1-aminoadamantane), a non-competitive NMDA antagonist, was used for long period as an antiviral against influenza and for the treatment of Parkinsonism. It has been used in some studies to reduce postoperative analgesic requirements [Citation8,Citation9] but to our knowledge there were no studies used this drug to reduce tourniquet induced hypertension. Therefore, the purpose of this study was to test the effect of preoperative oral amantadine, as an NMDA antagonist, on tourniquet-induced hypertension under general anesthesia as a primary outcome and postoperative analgesic requirements and side effects as a secondary outcome.
2 Method
After approval of the local ethical committee, informed written consents were obtained from 30 adult male patients, American Society of Anesthesiologists (ASA) physical status I or II, age ranging between 18 to 50 years old, scheduled for elective anterior cruciate ligament reconstruction with a tourniquet under general anesthesia.
This randomized, double blind, placebo controlled study was carried out in Dar Alshifa hospital (State of Kuwait) during the period from April 2013 to September 2013.
Patients were excluded from the study if they had sickle cell disease, peripheral vascular disease, history of DVT, poorly controlled hypertension, history of allergy to the studied drug or recent ingestion of cough suppressant (dextromethorphan), morbid obesity (BMI > 35).
Patients were randomly assigned into two equally divided groups (15 patients each) by using the closed envelop technique. The studied drugs were given by an anesthesia nurse unaware of the study medication as per the sealed envelope instruction (to maintain the blind nature of the study) as follows:
Amantadine group (group A): the patients received oral amantadine 200 mg capsule in the evening before surgery and 200 mg capsule 60 min before surgery (Symmetrel®, Novartis pharma AG., Basel, Switzerland) using the dose used in the study of Snijdelaar et al. [Citation8]
Placebo group (group P) (control group): the patients received placebo capsules.
During the preoperative anesthesia visit, the patients were informed about the study and how to use the patient controlled analgesia (PCA) machine postoperatively. The patients were premedicated with i.v. metoclopramide 10 mg and oral midazolam 5 mg 60 min before surgery.
When the patients reached the operation room, the monitors were attached including ECG, pulse oximetry, non-invasive arterial blood pressure cuff, skin temperature probe and bispectral index (BIS) (the BIS electrodes were placed on the forehead and were connected to the BIS monitoring system) (Aspect Medical Systems, Leiden, The Netherlands) with infusion of Ringer’s lactate solution according to fasting volumes, and maintenance volumes.
General anesthesia was induced with fentanyl 2 μg/kg, propofol 2 mg/kg, lidocaine 1 mg/kg and cisatracurium 0.15 mg/kg intravenously. The patients were intubated with oral cuffed tube lubricated with lidocaine gel 2% 2 min after cisatracurium administration and mechanically ventilated to maintain end tidal CO2 between 35 to 40 mmHg.
Anesthesia was maintained with sevoflurane 1.5% in 50% air/O2 mixture with adjustment of the sevoflurane concentration to maintain BIS value between 40 to 60. Analgesia was maintained by additional dose of fentanyl 50–100 μg if there were signs of inadequate analgesia (>20% increase in the heart rate and mean arterial blood pressure from the baseline). Esmolol 25 mg increments were given when systolic blood pressure (SBP), diastolic blood pressure (DBP) or heart rate (HR) increased >30% from the baseline reading. Muscle relaxation was maintained with cisatracurium boluses 0.03 mg/kg guided by peripheral nerve stimulator.
The pneumatic tourniquet (PTS ii portable tourniquet system, Delfi Medical Innovations Inc, Vancouver, Canada) 20 cm width was applied over cotton layer on the thigh of the operated limb which was elevated at 45° for 5 min with exsanguination using crepe bandage and inflation of the tourniquet pressure at 300 mmHg.
At the end of the surgery, the tourniquet was deflated with discontinuation of all anesthetics and the patients were extubated after reversal of neuromuscular blockade with intravenous 0.05 mg/kg neostigmine and 0.02 mg/kg atropine, and the patients were shifted to postanesthesia care unit (PACU) for monitoring and observation. The postoperative pain was treated according to our hospital protocol with tramadol 25 mg intravenous followed by intravenous PCA tramadol (bolus dose 10 mg, lockout time 15 min, and maximum limit 60 mg/4 h with no back ground infusion) for 24 h with additional intravenous tramadol 25 mg if the patients complained of pain during PCA (IVAC®PCAM, Cardinal Health, Switzerland).
The following parameters were recorded by an anesthesia nurse unaware of study medication; HR, SBP, and DBP were recorded at the following time: before induction of anesthesia (baseline), every 15 min after tourniquet inflation, before tourniquet deflation, and 10 min after tourniquet deflation, incidence of tourniquet-induced hypertension (defined as an increase of systolic or diastolic blood pressure >30% from baseline), time to first postoperative analgesic requirement, postoperative tramadol consumption during the first 24 h after surgery, postoperative side effects such as nausea and vomiting (treated with ondansetron 4 mg i.v.) or sedation [graded on a five-point scale: (1) fully awake and oriented; (2) drowsy; (3) eyes closed, arousable to command; (4) eyes closed, arousable to physical stimulation; and (5) eyes closed, unrousable to physical stimulation] [Citation10].
3 Statistical analysis
After a pilot study with ten patients, the mean maximum SAP (SD) was 123 (8.7) and 147 (8.9) in the amantadine group and the placebo group, respectively. Therefore, using the program of biostatistics version 3.01, the sample size was calculated as minimum five per group was needed to show a difference of maximum SAP 24 mmHg (SD 9 mmHg) between groups with the power set at 90% and the α-error level fixed at 0.05. However, we recruited 15 patients for each group.
Data values were presented as means (SD), or number (%). Numerical data were analyzed by using Student’s unpaired t-test. Nonparametric data were analyzed by using the Mann Whitney U-test. A value of P < 0.05 was considered significant. All statistical calculations were done using computer programs Microsoft Excel version 7 (Microsoft Corporation, NY, USA).
4 Result
Both groups of patients were similar regarding patients’ characteristics, tourniquet time and operation time ().
Table 1 Patients characteristics, tourniquet time and operation time.
There was no significant difference between the two groups in systolic pressure, diastolic pressure, and heart rate values before induction of anesthesia (BI) (baseline) ().
Table 2 Hemodynamic changes.
Systolic and diastolic blood pressures significantly increased in both groups compared to baseline values (P < 0.05) at Ti15, Ti30, Ti45, Ti60, Ti 75, and BTD with significantly lesser increase in amantadine group compared to placebo group at Ti45, Ti60, and Ti 75 (P < 0.05) with return back to normal values after tourniquet deflation ().
Heart rate significantly increased at Ti45, Ti60, and Ti 75 in both groups compared to baseline values (P < 0.05) with significantly lesser increase in amantadine group compared to placebo group (P < 0.05) with return back to normal values after tourniquet deflation ().
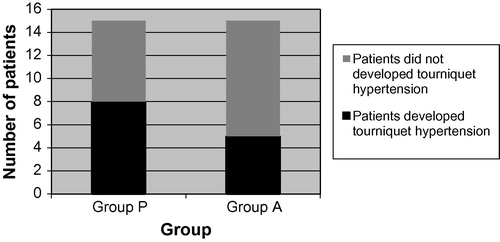
The number of patients showed tourniquet hypertension and given esmolol to control the hypertension was more in placebo group 8 out of 15 (53.3%) than amantadine group 5 out of 15 (33.3%) ().
Time to first request of analgesia was significantly longer in amantadine group compared to placebo group (P < 0.05). Also, total postoperative tramadol consumption during the first 24 h was significantly less in amantadine group compared to placebo group (P < 0.05) ().
Table 3 Time to first postoperative analgesic requirement and tramadol consumption during the first 24 h after surgery.
The incidence of postoperative nausea and vomiting was comparable in both groups without development of postoperative sedation in both groups ().
Table 4 Incidence of side effects.
5 Discussion
This study demonstrated that preoperative oral amantadine attenuated the increase in blood pressure and heart rate associated with tourniquet inflation compared with placebo with reduction of the incidence of the tourniquet-induced hypertension from 53.3% in placebo group to 33.3% in amantadine group with decrease in the number of patients given esmolol to control the hypertension or tachycardia from 8 out of 15 in placebo group to 5 out of 15 in amantadine group.
The exact mechanism of the cardiovascular changes associated with tourniquet inflation is unknown [Citation2]. However, few theories tried to explain the tourniquet-induced hypertension. One theory suggested that the development of the tourniquet pain causes activation of the sympathetic nervous system. This theory is supported by the finding that the onset of the tourniquet-induced hypertension is analogous to the onset of tourniquet pain and both usually occurred 30–60 min after cuff inflation [Citation11], Tetzlaff et al., concluded that there is a correlation between tourniquet induced hypertension and sympathetic nervous system activation [Citation12], Heropoulos et al., found increase in plasma catecholamines in association with tourniquet hypertension [Citation13], and preoperative clonidine suppresses the cardiovascular and hyperadrenergic response to tourniquet inflation [Citation4,Citation14].
Another theory suggested that tourniquet inflation causes tissue ischemia with discharge of impulses in both large myelinated A fibers and unmyelinated C fibers, the A fibers rapidly undergo conduction block with disinhibition of pain perception conducted by C fibers. Continuous firing of C fiber nociceptors causes activation of NMDA receptors in the dorsal horn of the spinal cord leading to central sensitization [Citation2].
We suggested that oral amantadine, as an NMDA antagonist, attenuated the tourniquet induced cardiovascular changes through attenuation of the central sensitization and modulation of the transmission of peripheral noxious stimuli from periphery toward the higher centers in the brain.
This theory was supported by the previous studies of Yamashita and colleagues who showed that preoperative oral dextromethorphan reduced the increase in arterial blood pressure and heart rate during tourniquet inflation [Citation1], Park and colleagues concluded that pre-operative intravenous ketamine (0.1 mg/kg) significantly prevents systemic arterial hypertension during tourniquet inflation under general anesthesia [Citation2], and Satsumae et al., reported that magnesium sulfate reduced the tourniquet pain in healthy volunteers [Citation6].
In this study preoperative amantadine administration significantly reduced the postoperative tramadol consumption with increase in the time to request of the first dose of postoperative analgesia, this could be explained by potentiation of the analgesic action of tramadol by amantadine through NMDA receptor blockade, this finding is in agreement with the reports of Snijdelaar et al. [Citation8] and Bujak-Giżycka et al. [Citation9] who observed reduction of postoperative morphine consumption with amantadine.
Adequate depth of anesthesia was maintained during the study by maintaining BIS value between 40 to 60 by adjustment of sevoflurane concentration, also adequate analgesia and muscle relaxation were maintained by additional doses of fentanyl and cisatracurium respectively to exclude their inadequacy as causes of intraoperative hypertension and tachycardia.
Amantadine did not increase the incidence of postoperative nausea and vomiting because we used only two doses of amantadine as the same used in the study of Snijdelaar and colleagues [Citation8] who found the same results, in addition administration of the tramadol in relative low doses in PCA did not increase the incidence of nausea and vomiting [Citation15], also prophylactic administration of antiemetic (metoclopramide) with tramadol lower the incidence of associated nausea and vomiting [Citation16].
We concluded that preoperative use of oral amantadine reduced the tourniquet induced hypertension with reduction of postoperative analgesic requirements in anterior cruciate ligament reconstruction surgery under general anesthesia. Further studies are required on more number of patients to confirm the effectiveness of oral amantadine on the tourniquet induced hypertension.
Conflict of interest
There is no conflict of interest
Notes
Available online 4 September 2014
References
- S.YamashitaH.YamaguchiY.HisajimaK.IjimaK.SaitoA.ChibaT.YasunagaPreoperative oral dextromethorphan attenuated tourniquet-induced arterial blood pressure and heart rate increases in knee cruciate ligament reconstruction patients under general anesthesiaAnesth Analg982004994998
- J.W.ParkY.H.JungC.W.BaekH.KangS.M.ChaEffects of low dose ketamine on tourniquet-induced haemodynamic responses during general anaesthesiaJ Int Med Res3552007600608
- J.Y.JungJ.H.HanJ.W.YiJ.M.KangRemifentanil prevents tourniquet-induced arterial pressure increase in elderly orthopedic patients under sevoflurane/N2O general anesthesiaInt J Med Sci942012311315
- A.HonarmandM.R.SafaviPreoperative oral dextromethorphan vs. clonidine to prevent tourniquet-induced cardiovascular responses in orthopaedic patients under general anaesthesiaEur J Anaesthesiol2462007511515
- H.C.LaoP.S.TsaiJ.Y.SuT.G.KwokC.J.HuangDexmedetomidine attenuates tourniquet-induced hyperdynamic response in patients undergoing lower limb surgeries: a randomized controlled studyJ Surg Res17912013e99e106
- T.SatsumaeH.YamaguchiS.InomataM.TanakaMagnesium sulfate attenuates tourniquet pain in healthy volunteersJ Anesth2722013231235
- D.H.LeeD.L.JeeS.Y.KimJ.M.KimH.M.LeeMagnesium sulphate attenuates tourniquet-induced hypertension and spinal c -fos mRNA expression: a comparison with ketamineJ Int Med Res342006573
- D.G.SnijdelaarG.KorenJ.KatzEffects of perioperative oral amantadine on postoperative pain and morphine consumption in patients after radical prostatectomy: results of a preliminary studyAnesthesiology10012004134141
- B.Bujak-GiżyckaK.KąckaM.SuskiR.OlszaneckiJ.MadejJ.DobrogowskiR.KorbutBeneficial effect of amantadine on postoperative pain reduction and consumption of morphine in patients subjected to elective spine surgeryPain Med1332012459465
- E.WilsonA.DavidN.MacKenzieI.S.GrantSedation during spinal anaesthesia: comparison of propofol and midazolamBr J Anaesth6419904852
- Micheal K.UrbanAnaesthesia for orthopaedic surgeryR.D.MillerMiller’s anesthesia7th ed.2010Churcill Livingstone PublishersPhiladelphia2252
- J.E.TetzlaffJ.O’HaraH.J.YoonA.SchubertTourniquet induced hypertension correlates with autonomic nervous system changes detected by power spectral heart rate analysisJ Clin Anesth91997138142
- M.HeropoulosH.SchierenJ.L.SeltzerR.R.BartkowskiJ.LessinM.TorjmanIntraoperative hemodynamic, renin, and catecholamine responses after prophylactic and intraoperative administration of intravenous enalaprilatAnesth Analg801995583590
- M.P.ZalunardoD.SerafinoP.SzelloeF.WeisserA.ZollingerB.SeifertPreoperative clonidine blunts hyperadrenergic and hyperdynamic responses to prolonged tourniquet pressure during general anesthesiaAnesth Analg942002615618
- W.W.PangM.S.MokS.HuangC.P.HungM.H.HuangIntraoperative loading attenuates nausea and vomiting of tramadol patient-controlled analgesiaCan J Anaesth47102000968973
- K.A.LehmannTramadol in acute pain (French)Drugs53suppl. 219972533
