Abstract
Background
Beach chair position (BCP) is used in arthroscopic shoulder operations for its advantages. The BCP together with deliberate hypotension used to decrease intraoperative blood loss during arthroscopic shoulder procedures, this may have risk to cause postoperative neurological insults. Dexmedetomidine and esmolol are used to induce deliberate hypotension. Near-infrared spectroscopy (NIRS) provides a non-invasive technique of continuous monitoring of regional cerebral tissue oxygen saturation (rScO2). In this study we evaluate the prevalence of rScO2 during hypotensive anesthesia induced by intra-operative infusion of either dexmedetomidine or esmolol in patients undergoing elective arthroscopic shoulder surgery in the BCP.
Patients and methods
Fifty patients scheduled for elective arthroscopic shoulder surgery under general anesthesia with hypotensive technique in BCP, randomly assigned into two equal groups, dexmedetomidine group (D Group) and esmolol group (E Group) according to the drug used for deliberate hypotension. MAP, HR, BIS and rScO2 were recorded before induction of anesthesia T0, post-induction of anesthesia T1 as baseline, 5 min after BCP T2, 5 min after starting the studied drug T3, 30 min T4, 60 min T5, 90 min T6, 5 min after stopping the studied drug T7, 5 min after return to supine T8 and after extubation T9.
Results
In D group there was significant decrease in Lt.rsco2 and Rt.rsco2, at T2 to T7 compared to T1. In E group there was significant decrease in Lt.rsco2 and Rt.rsco2 at T2, to T7 compared to T1. In D group two patients had CDEs compared to five patients in E group.
Conclusion
In patients undergoing shoulder arthroscopic surgery under general anesthesia, the BCP significantly decreases rScO2, with further slight decrease of rScO2 with dexmedetomidine and esmolol induced hypotension with no affection of postoperative cognitive function with both drugs. Dexmedetomidine and esmolol are safe drugs with better safety of dexmedetomidine over esmolol.
1 Introduction
In the last decades open anterior stabilization and capsular shift were traditionally considered to be “mainstay and gold standard” for anterior shoulder instability, however, most surgeons lately found that arthroscopic anterior stabilization has become the procedure of choice [Citation1].
The beach chair (BCP) and lateral decubitus (LDP) positions are both reliable techniques to perform effective arthroscopic shoulder operations [Citation2]. The use of BCP for shoulder arthroscopic procedures started from early 1980s [Citation3]. The BCP advantages include lack of brachial plexus strain, proper intra-articular visualization, and ease of conversion to an open approach if necessary [Citation4], depending on joint positioning and surgeon training [Citation5].
The BCP in association with deliberate hypotension has been used to decrease intraoperative blood loss and provide a relatively blood-free surgical environment to improve surgical field [Citation6]. However, this combination has the potential to affect cerebral perfusion pressure and oxygenation during surgery and induce cerebral ischemia [Citation7].
Deliberate hypotension can be achieved by using anesthetics, direct acting vasodilators, β adrenergic blockers and calcium channel blockers. However, it may have the risk to cause postoperative neurological insults due to cerebral hypoperfusion [Citation8], so ideal hypotensive agent should be easy administrated in titration without toxic side effect, have short term effect, no change in cardiac performance and maintaining cerbrovascular autoregulation [Citation9].
Dexmedetomidine (DEX) is an imidazole-derivative adrenoceptor agonist representing high selectivity for α2 adrenergic agonist [Citation10]. It has a sedative, analgesic and induces inhibition of central sympathetic outflow [Citation11]. It specifically stimulates presynaptic α2 receptors [Citation12] with dose dependent decrease in arterial pressure, heart rate, cardiac output and norepinephrine release [Citation13].
Esmolol is a cardio-selective β1 blocker characterized by ultra-short half life of about 2 min. Its peak effect starts 6–10 min after IV injection. It is titrated easily with its short clearance time of average 9 min after stoppage of infusion. These special pharmacokinetic properties have led to the successful use of esmolol in deliberate hypotension [Citation14].
The central nervous system (CNS) is considered to be the main end-point of most general anesthetics, however, it remains the least monitored organ during anesthesia [Citation14]. Near-infrared spectroscopy (NIRS) provides a non-invasive technique of continuous monitoring of regional cerebral tissue oxygen saturation (rScO2) [Citation15]. This method has been demonstrated repeatedly to monitor changes in parenchymal and microcirculatory oxygenation of the frontal cerebral cortex reflecting tissue oxygen use [Citation16] as a marker of the balance between oxygen supply and demand [Citation17], which allow for the immediate recognition and management of cerebral desaturation events (CDEs) that would otherwise be undetected with other conventional intraoperative monitoring during procedures with a high risk of adverse neurological outcomes [Citation18].
The aim of this prospective, randomized, double blind study was to compare the prevalence of regional cerebral oxygen desaturation during hypotensive anesthesia induced by intra-operative infusion of either dexmedetomidine or esmolol in patients undergoing elective arthroscopic shoulder surgery in the beach chair position with further detection of the occurrence of postoperative cognitive dysfunction (POCD).
2 Materials and methods
This prospective, randomized, double blind study was conducted in Prince Salman Hospital in Kingdom of Saudi Arabia after obtaining the approval of the ethical committee board of the hospital from February 2013 till December 2013.
A written informed consent was taken from fifty patients American Society of Anesthesiologists physical status (ASA) I or II, 20–55 years old scheduled to undergo elective arthroscopic shoulder surgery under general anesthesia with hypotensive technique in beach chair position (BCP). Based on a computer-generated randomization list, patients were classified into two groups, dexmedetomidine group (D Group) and esmolol group (E Group) according to the drug used for deliberate hypotension during general anesthesia.
Exclusion criteria included, patients with preexisting cerebral pathology (such as previous episodes of cerebral ischemia or stroke), patients clinically apparent to have neurological or cognitive dysfunction, cervical stenosis, cervical disk herniation, documented carotid stenosis, history of serious psychiatric illness, Mini Mental State Examination (MMSE) score of 23 or less and history of orthostatic hypotension, myocardial infarction or uncontrolled hypertension.
Anesthetic management was carefully standardized in all patients in both groups. Patients were premedicated with midazolam IV 0.02 mg/kg after insertion of a 22 G peripheral intravenous cannula 1 h before induction of anesthesia. Upon arrival to the operating room, standard monitoring (Aisys; Datex-Ohmeda, Inc., a General Electric Company, doing business as GE Healthcare, Madison, Wisconsin, USA) was applied; heart rate (HR), non invasive blood pressure, and oxygen saturation (SPO2) were continuously monitored. Standard Bispectral Index (BIS)® electrode montage (Aspect Medical Systems, Natick, MA) was applied to the forehead before induction of anesthesia, and BIS was measured continuously using an Aspect BIS® A-2000 monitor version 3.31 (Aspect Medical Systems).
Patients were actively warmed throughout the procedure using a forced-air warming system (Bair-Hugger, Augustine-Medical, Eden Prairie, MN) to maintain intraoperative normothermia as the esophageal temperature was monitored continuously using (Mon-a-Therm; Mallinckrodt, St. Louis, MO) and maintained at 36–37°.
Regional cerebral oxygen saturation (rScO2) was continuously monitored using near-infrared spectroscopy (NIRS) with an INVOS® 5100C cerebral oximeter (Somanetics, Troy, MI). Before induction of general anesthesia, after cleansing the skin area with alcohol, sensors for cerebral oximeter were placed bilaterally on the right and left sides of the forehead according to the manufacturer’s instructions with the caudal border about 1 cm above the eyebrow with the medial edge at the midline as this position makes the light source and sensors away from the frontal sinus and temporalis muscle, rScO2 values from the right and left frontal lobes were averaged to determine cerebral oxygenation. Another 20 G peripheral cannula was inserted; one for administration of the study drug and the other one used for induction of anesthesia.
After full preoxygenation, Granisetron 10 μg/kg IV was given then anesthesia was induced with propofol (1.5–2.0 mg/kg), and fentanyl (2 μg/kg). The trachea was intubated 2–3 min after administration of cis-atracurium 0.15 mg/kg IV, and the lungs were mechanically ventilated with 40% oxygen in nitrous oxide. Anesthesia was maintained by 1–2% end-tidal sevoflurane in 40% oxygen in nitrous oxide flow. Intraoperative fluid administration was 6–8 ml/kg of lactated ringer solution. Invasive blood pressure monitoring was done by using a 20 gauge catheter inserted into a radial artery in the contralateral side of operation and connected to a pressure transducer (Aisys; Datex-Ohmeda, Inc., a General Electric Company, doing business as GE Healthcare, Madison, Wisconsin, USA) for continuous monitoring of invasive blood pressure. The pressure transducer was referenced to the mid-axillary level when patient was supine and referenced to the external ear canal level when in BCP to reflect directly cerebral perfusion pressure.
Approximately 10 min after anesthesia induction, when hemodynamics became stable, the head was secured in neutral position to ensure that cerebral venous drainage was not impaired. The back of the operating room table was then raised to 65–75° above the horizontal plane to put the patient into the beach-chair position (BCP) using a beach-chair table (T-MAX beach chair; TENET Medical Engineering, Calgary, Alberta, Canada), after which the surgery was started.
After induction of anesthesia and the patient positioned in BCP, D group received loading dose of 1 μg/kg of dexmedetomidine {Precedex® 200 μg/2 ml (Hospira, USA)} diluted in 10 ml of 0.9% normal saline infused over 10 min then iv bolus of 10 ml of 0.9% normal saline, followed by infusion rate 0.2–0.6 μg/kg/h (200 μg dexmedetomidine diluted in 48 ml of 0.9% normal saline injection for a final concentration of 4 μg/ml). Patients who were allocated to E group, started to receive IV 10 ml of 0.9% normal saline over 10 min followed by iv bolus esmolol 0.5 mg/kg {Brevibloc® 100 mg/10 ml (Baxter Deutschland GmbH)} diluted in 10 ml of 0.9% normal saline followed by infusion rate of 0.05–0.3 mg/kg/min throughout the operation (400 mg esmolol added to 10 ml of 0.9% normal saline for a final volume 50 ml with concentration of 8 mg/ml).
Patients were mechanically ventilated to maintain the end-tidal carbon dioxide (ETCO2) tension at 30–35 mmHg. Neuromuscular blockade was carefully controlled by train-of-four monitoring, and additional boluses of cis-atracurium were administered to maintain one twitch response in response to electrical stimulation of the ulnar nerve during the surgical procedure.
At the end of main surgical procedures, deliberate hypotensive drug infusion and incremental doses of cisatracurium were stopped. Paracetamol 1 g IVI over 15 min was given. The residual of neuromuscular blocker was antagonized with neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg. After extubation and full recovery, the patient received 1 mg/kg pethidine IM as postoperative analgesia then transferred to the post anesthesia care unit (PACU).
During the maintenance of anesthesia by the hypotensive technique, tachycardia was defined as a persistent increase in HR exceeding 90 beats/min for more than 5 min, which was treated by IV administration of 1 μg/kg of fentanyl. If bradycardia occurred (HR < 50 beats/min), it was treated with 0.01 mg/kg of atropine intravenously. MAP was maintained between 55 and 65 mmHg, hypo tension less than 50 mmHg of the MAP was treated by a gradual decrease of the studied drug to achieve the desired MAP, whereas an increase of MAP of more than 65 mmHg was treated by increasing the dose of hypotensive drug used.
Routine monitoring included invasive measurement of mean arterial blood pressure (MAP), heart rate (HR), and rhythm by 5-lead electrocardiography, pulse oximetry (O2Sat), BIS, esophageal temperature and regional cerebral oxygen saturation (rScO2) throughout the surgery. The end-tidal concentrations of carbon dioxide, sevoflurane, and nitrous oxide were measured using a gas analyzer.
These variables (MAP, heart rate, BIS and rScO2) were recorded before induction of anesthesia T0 (supine position), post-induction of anesthesia T1 (supine position) as baseline values, 5 min after BCP T2, 5 min after starting the studied drug T3, 30 min after starting the studied drug T4, 60 min after starting the studied drug T5, 90 min after starting the studied drug T6, 5 min after stopping the studied drug T7, 5 min after change from BCP to supine position T8 and after extubation of the patient T9.
Baseline rScO2 was defined as the average saturation value over a 1-min period after induction of general anesthesia. Cerebral desaturation was defined as a reduction of rScO2 less than 75% of baseline for more than 15 s [Citation19,Citation14], which should be treated by the attending anesthesiologist by checking the ventilator, head position, and tubing system, increasing Fio2, increasing end-tidal CO2 partial pressure if the end-tidal CO2 was less than 30 mmHg, and increasing arterial blood pressure with intravascular fluid administration and/or vasopressor drugs as ephedrine (5 mg IV) if MAP pressure was less than 50 mmHg [Citation20].
The number and duration of cerebral desaturation events (CDEs) together with the number and type of interventions used to treat CDEs were recorded. In addition, interventions used to treat MAP reductions which did not decrease rScO2 were also noted. All these data were recorded from BCP until tracheal extubation.
At postoperative visit on the evening of surgery, the patient was assessed neurologically by an anesthetist who was not related to the study, for gross motor and sensory neurologic evaluation and gross cognitive evaluation (orientation in time and space, recall of name, date of birth, and address). Any side effects were recorded.
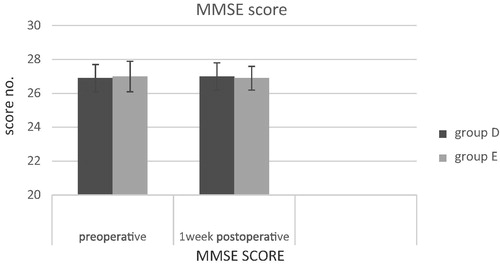
Cognitive function of the patients was assessed using the MMSE test the day before surgery and then reassessed 1 wk after the operation. The mini-mental state examination (MMSE) or Folstein test is a brief 30-point questionnaire test that is used to screen for cognitive impairment. The MMSE test includes simple questions and problems in a number of areas: the time and place of the test, repeating lists of words, arithmetic, language use and comprehension, and basic motor skills [Citation21] ().
Table 1 Mini-mental state examination (MMSE).
Postoperative cognitive dysfunction (POCD) was considered when there was decrease in MMSE score 2 points or more from preoperative value [Citation20,Citation22].
3 Statistical analysis
Group sample sizes of 25 per group achieved 80% power to detect a clinically relevant decrease in cerebral oxygen saturation with mean difference of 10 and estimated SD of 5 and with a significance level (alpha) of 0.05 using a two-sided two-sample t-test.
Statistical analysis was done on a personal computer using the Statistical Package for Social Sciences version 16.0 (SPSS© v. 16.0, SPSS Inc., Chicago, IL, USA). Qualitative data were analyzed with Pearson’s Chi-square test and were presented as number [%]. Quantitative data were analyzed using unpaired t-student test for between group comparison, and paired t-test for within group comparison, data were presented as mean ± standard deviation. A P value of <0.05 was considered statistically significant.
4 Results
A total of fifty-two adult patients were enrolled in this study, two cases were excluded throughout the course of the study, one case excluded due to incomplete data collection and other one due to unplanned conversion to open surgical procedure.
There was no statistical significant difference in the patients’ demographic data as regards age, sex, weight and ASA classification ().
Table 2 Demographic data in both groups.
There was no statistical significant difference between both groups as regards patient characteristics (see ).
Table 3 Patients’ characteristics in both groups.
As regards the change in MAP, within group D, there was significant decrease in MAP T2 (71.52 ± 8), T3 (64.5 ± 4), T4 (61.5 ± 2.9), T5 (59.5 ± 2.6), T6 (58.2 ± 2.7) when compared to T1 (83.5 ± 8.5), and insignificant decrease in MAP in T7 (77.8 ± 8.4) and T8 (79.6 ± 5.36) compared to T1 (83.5 ± 8.5). There was no significant change in MAP T9 (80.6 ± 7.3) when compared to T1 (83.5 ± 8.5) ().
Table 4 Changes of mean arterial blood pressure in both D group (Dexmedetomidine) and E group (Emolol).
As regards the change in MAP, within group E, there was significant decrease in MAP T2 (69.4 ± 6.7), T3 (64 ± 3.3), T4 (62.2 ± 5.7), T5 (59.4 ± 3.2), T6 (58.5 ± 3.7) when compared to T1 (83.8 ± 10), and insignificant decrease in MAP in T7 (78.2 ± 5.1) and T8 (81.3 ± 9.3) compared to T1 (83.8 ± 10). There was no significant change in MAP T9 (82.4 ± 5.9) when compared to T1 (83.8 ± 10) ().
As regards the change in MAP, in between groups, there was no significant difference between both groups in different time intervals ().
As regards the change in HR, within group comparison in D group, there was significant decrease in HR T2 (76.2 ± 8), T3 (76.9 ± 10), T4 (73.9 ± 6.7), T5 (69.6 ± 6.9), T6 (66.3 ± 7) when compared to T1 (88.4 ± 10.1), and insignificant decrease in HR in T7 (77.3 ± 8.7), T8 (76.8 ± 9.7) and T9 (77.6 ± 4) compared to T1 (88.4 ± 10.1) ().
Table 5 Changes of heart rate in both D group (Dexmedetomidine) and E group (Emolol).
While, the change in HR, within group comparison in E group, there was significant decrease in HR T2 (74.5 ± 9), T3 (77.8 ± 10), T4 (71.8 ± 6.2), T5 (67.4 ± 5.6), T6 (67.8 ± 6.4) when compared to T1 (87.3 ± 3.9), and insignificant decrease in HR in T7 (78.7 ± 7.6) and T8 (81.6 ± 6.4) compared to T1 (87.3 ± 3.9). There was no significant change in HR T9 (82 ± 7) when compared to T1 (87.3 ± 3.9) ().
As regards the change in HR, in between groups, there was no significant difference between both groups in different time intervals ().
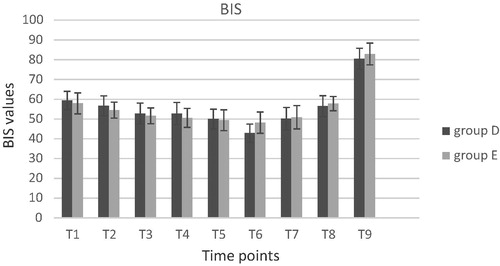
As regards the BIS readings representing the depth of anesthesia, there was no significant difference within group comparison in both group or in between groups in different time intervals except if we compared T9 with T1 within group comparison in both group as the patient is awake in T9 reading .
As regards the change in Lt.rsco2 within D group, there was significant decrease in Lt.rsco2 at T2 (76.8 ± 7.8), T3 (71 ± 5.8), T4 (70.4 ± 4.1), T5 (69.6 ± 3.5), T6 (72 ± 5.3) and T7 (71 ± 5.2) when compared to T1 (88.6 ± 4.3) and insignificant decrease in Lt.rsco2 in T8 (86.7 ± 7.7) compared to T1 (88.6 ± 4.3). There was no significant change in Lt.rsco2 at T9 (87.7 ± 4.1) when compared to T1 (88.6 ± 4.3) ().
Table 6 Changes of Lt.rsco2 in both D group (Dexmedetomidine) and E group (Emolol).
As regards the change in Lt.rsco2 within in E group, there was significant decrease in Lt.rsco2 at T2 (73.5 ± 7.5), T3 (69.9 ± 6.3), T4 (71 ± 6.2), T5 (65.6 ± 5.7), T6 (70 ± 5.5) and T7 (68.4 ± 4.8) when compared to T1 (86.9 ± 3.7), and insignificant decrease in Lt.rsco2 in T8 (85.5 ± 5.2) compared to T1 (86.9 ± 3.7). There was no significant change in Lt.rsco2 at T9 (85.7 ± 4.4) when compared to T1 (86.9 ± 3.7) ().
As regards the change in Lt.rsco2 in between groups, there was no significant difference between both groups in different time intervals except at T5 there was significant decrease in E group (65.6 ± 5.7) in comparison with D group (69.6 ± 3.5) at this time .
As regards the change in Rt.rsco2, within D group, there was significant decrease in Lt.rsco2 at T2 (76 ± 4.6), T3 (70.1 ± 5.6), T4 (71.2 ± 5.4), T5 (70 ± 3), T6 (68.4 ± 3.8) and T7 (70.9 ± 4) when compared to T1 (87.6 ± 5), and insignificant decrease in Lt.rsco2 in T8 (85 ± 4.3) compared to T1 (87.6 ± 5). There was no significant change in Lt.rsco2 at T9 (87.8 ± 4.4) when compared to T1 (87.6 ± 5) ().
Table 7 Changes of Rt.rsco2 in both D group (Dexmedetomidine) and E group (Emolol).
As regards the change in Rt.rsco2, within E group, there was significant decrease in Lt.rsco2 at T2 (74.3 ± 10), T3 (71.9 ± 4.2), T4 (70.6 ± 4.2), T5 (66.3 ± 4.4), T6 (68.7 ± 4.8) and T7 (71.6 ± 3.8) when compared to T1 (87.6 ± 6.8), and insignificant decrease in Lt.rsco2 in T8 (84.5 ± 4.5) compared to T1 (87.6 ± 6.8). There was no significant change in Lt.rsco2 at T9 (88 ± 4.5) when compared to T1 (87.6 ± 6.8) ().
As regards the change in Rt.rsco2, in between groups, there was no significant difference between both groups in different time intervals except at T5 there is significant decrease in E (66.3 ± 4.4) group in comparison with D (70 ± 3) group at this time ().
As regards the occurrence of cerebral desaturation events (CDEs), only two patients had CDEs in D group compared to five patients had CDEs in E group. Each patient in D group had only one CDEs attack while in E group, three patients had one CDEs attack and the other two patients each one had two CDEs attack. Patients in D group who had CDEs attack require no interventional management and disappeared spontaneously, while in E group two patients of the five who had CDEs required management by the attending anesthetist to treat the CDEs attacks as they last more than 30 s ().
Table 8 Cerebral desaturation events (CDES).
As regards the MMSE score there was no significant difference in both groups within group comparison or in-between group comparison .
P value >0.05 was considered statistically not significant.
5 Discussion
This prospective, randomized, double blind study was conducted to compare the prevalence of rScO2 during hypotensive anesthesia induced by intra-operative intra-venous infusion of either dexmedetomidine or esmolol in patients undergoing elective arthroscopic shoulder surgery in the BCP with further detection of the occurrence of POCD, as the association of deliberate hypotension with BCP under general anesthesia has the potential to induce changes in cerebral perfusion pressure which may be the major etiology of poor neurological outcomes [Citation23].
Alterations in systemic hemodynamics occur when postural conditions are changed from supine to BCP, including diminished cardiac index, stroke volume, and arterial pressure [Citation24] caused by marked decrease of venous return which persists for up to 30 min after the positioning in an anesthetized patient [Citation25]. In conscious subjects, sitting position activates the sympathetic nervous system, resulting in an increase of systemic blood pressure associated with increased systemic vascular resistance and sustained reduction in cardiac output. Compensatory increases in sympathetic nervous system activation and systemic vascular resistance are attenuated under general anesthesia causing more pronounced hypotension [Citation26].
In the current study, MAP decreased abruptly from the baseline values (T1) when patients were switched to BCP in both groups, with a statistically significant value. MAP was not statistically significant between the 2 groups during the study. Our findings corroborate previous studies of Fuchs and his colleagues [Citation27] and Tange and his colleagues [Citation28] who have confirmed considerable hemodynamic shift when positioning from the supine to the BCP.
In D group, this hemodynamic profile after starting the hypotensive agents can be attributed to the known sympatholytic effect of α2 agonists which are involved in regulating the autonomic and cardiovascular systems [Citation29]. Dexmedetomidine sympatholytic action is manifested by dose-dependent decrease in arterial blood pressure, heart rate, cardiac output and norepinephrine release [Citation30]. This was coinciding with Basar and his colleagues [Citation31] who investigated the effect of single dose of dexmedetomidine and reported significant reduction in MAP and HR.
Esmolol is an ultra-short acting selective B1 adrenergic antagonist and possesses no significant membrane stabilizing activity, given as continuous infusion to induce stable and controllable beta-adrenergic block [Citation32], providing a stable course of controlled hypotension and produces beneficial effects in the surgical field and in blood conservation [Citation33]. Negative chronotropic and ionotropic effects of esmolol decrease the cardiac output which lowers arterial blood pressure. When heart rate and strength of contractions are decreased this will reduce arterial pressure and carotid sinus baroreceptors response [Citation34].
Esmolol had extremely short half-life (about 9 min). This explained that there was no significant change in HR in T9 when compared to T1, in contrast to dexmedetomidine which had insignificant decrease in HR in T9 when compared to T1, as it had more prolonged action compared to esmolol.
In the present study, MAP was maintained between 55 and 65 mmHg as outcome studies have demonstrated that a reduction of the mean arterial pressure (MAP) to 55–65 mmHg or a decrease of 30% from baseline is safe with regards to endorgan perfusion and oxygen delivery [Citation35].
During this research work, invasive blood pressure was continuously measured at the level of the external auditory meatus, which is representing the level of the circle of Willis, to assess accurately cerebral perfusion pressure. This was explained by the “open model” or “waterfall” theory, as blood flows vertically from the heart, there is a reduction in arterial pressure directly related to the weight of the column of blood [Citation36,Citation37]. This was coinciding with ko and his colleagues [Citation38] who stated that “Monitoring cerebral rScO2 and MAP at the level of brain can be helpful to detect the possibility of cerebral desaturation earlier”. However, Pranevicius and his colleagues [Citation39] stated that no need for modifying the level of measurement as long as the CVP can be maintained above 18 mmHg.
Factors which may modulate cerebral oximetry values include depth of anesthesia, anesthetic technique, arterial carbon dioxide concentrations, inspired oxygen content and MAP [Citation40]. Therefore, anesthetic management was carefully standardized in all patients in both groups, MAP was maintained between 55 and 65 mmHg, end-tidal carbon dioxide (ETCO2) tension at 30–35 mmHg and BIS readings representing the depth of anesthesia, there was no significant difference within group comparison in both group or in between groups comparison in different time intervals reflecting stable depth of anesthesia in both groups all through the anesthesia course.
Brain oxygenation can be measured invasively by jugular bulb oximetry to measure jugular venous oxygen saturation (Sjvo2) as an index of cerebral blood flow/metabolism coupling [Citation15], Sjvo2 is generally accepted as a method for the monitoring of global cerebral oxygen saturation and rScO2 as a method for monitoring regional oxygen saturation [Citation19].
NIRS measures the ratio of oxyhemoglobin to total hemoglobin in a field beneath the sensor, and this ratio is expressed as a percentage of rScO2 on the right and left side [Citation41]. rScO2 has been reported to be more sensitive than jugular venous oxygen saturation Sjvo2 to brain ischemia. Also, McLeod and his colleagues found that NIRS correlated more closely with changes in Sjvo2 [Citation42]. So, rScO2 may be an alternative method for detecting brain ischemia during induced hypotension [Citation43].
In the present study, there was significant decrease in both Rt.rsco2 and Lt.rsco2 with BCP after induction of general anesthesia in both groups, however Fuchs and his colleagues [Citation27] found that rScO2 values in the BCP were not different from those in the supine position in non-anesthetized volunteers. However, rScO2 values in the sitting position were significantly lower than those in the supine position in anesthetized patients, although their MAP was maintained. These results were explained by the role of general anesthesia in impairment of regulatory pathways of peripheral circulation and cerebral autoregulation and thus indicate that changes in rScO2 related to BCP cannot be only explained by changes in hemodynamic parameters as MAP.
In our study Rt.rsco2 and Lt.rsco2 values were influenced also by deliberate hypotension in both groups. Our results were agreed with Lee and his colleagues [Citation44] who found that the BCP combined with induced hypotension significantly decreases rSO2 in patients undergoing shoulder arthroscopic surgery under general anesthesia; however they used remifentanil and nitroglycerine in deliberate hypotension. Also, Endoh and his colleagues [Citation45] who found decreased rsco2 in controlled hypotension induced by nicardipine. But in our work it was found that there was significant decrease in Rt.rsco2 and Lt.rsco2 in E group compared with D group at T5, but this was in contrast to the results of Heinke and his colleagues [Citation46] who stated that moderate esmolol doses do not change cognitive performance and had no direct effects on CBF, so this excludes regional or global effects of esmolol on CBF. However, this study did not use higher esmolol doses which may cause a greater reduction of cardiovascular variables. Moreover, this study was done in awake volunteers, so whether these data can be applied under general anesthesia with BCP, needs to be clarified in future investigations.
The incidence of CDEs in patients monitored with NIRS undergoing elective shoulder surgery in the beach chair position in many previous studies is quite variable and ranges from 8% to 80% [Citation47,Citation48,Citation44,Citation49,Citation28]. Despite the frequent occurrence of CDEs in these patients, no clear neurologic insults were documented [Citation48]. This can be explained by limited duration of the surgical procedure, as severity and duration of cerebral hypoperfusion are critical determinants of tissue damage, so, viability-time thresholds usually not exceeded to cause neurologic deficits [Citation50].
The normal range for rScO2 values was variable in different studies, Madsen and his colleagues [Citation51] stated that the normal range for rScO2 values in 39 healthy resting subjects is 55–78, Similarly, Casati and his colleagues [Citation14] reported baseline rScO2 values 63 ± 8 in healthy elderly patients undergoing general surgery, also Kim and his colleagues [Citation52] reported that mean baseline rScO2 value was 71 ± 6 in healthy volunteers aged 20–36 years.
In the present study we defined cerebral desaturation events (CDEs), as a reduction of rScO2 less than 75% of baseline for more than 15 s in agreement with Casati and his colleagues [Citation22] and Iglesias and his colleagues [Citation53], however other literature defined a CDE as a drop in rScO2 of 20% or greater from baseline or an rScO2 of less than 55% for any time period [Citation18] and this definition depend on the fact that in conscious patients, a 20% decrease in frontal lobe oxygenation is associated with clinical symptoms and signs of cerebral ischemia [Citation54]. Also during carotid endarterectomy, 20% or greater drop in rScO2 during clamping of carotid artery is associated with a 20-fold increase in obvious signs and symptoms of cerebral ischemia [Citation55].
In the present study, the MMSE was used for evaluating cognitive function as it has many advantages include high validity and reliability, ease of use, brevity and suitability for bedside use. Also, MMSE is very appropriate for repeated cognitive assessments over time [Citation22]. There are other sensitive and specific scores as regards the assessment of cognitive functions evaluating different components of cognitive function; however, they have major drawback of lengthy, complex administration guidelines and long time in its application [Citation56].
In our study, as regards the MMSE score there was no significant difference in both groups within group comparison or in-between group comparison. This was coinciding with Williams-Russo and his colleagues [Citation57] who found no POCD after hypotensive epidural anesthesia in elderly patients. Also, Townes and his colleagues [Citation58] reported there were no neuropsychological changes or decrease in MMSE score after induced hypotension in healthy young adults.
The absence of a significant difference between preoperative and postoperative MMSE values could be explained by proper management of any intra-operative CDEs. Also, proper monitoring of rScO2 values after BCP and induced hypotension preserve intra-operative cerebral perfusion and oxygenation which may protect the CNS from any insult.
6 Conclusion
In patients undergoing shoulder arthroscopic surgery under general anesthesia, the beach-chair position significantly decreases rScO2, with further slight decrease of rScO2 with dexmedetomidine and esmolol induced hypotension with no affection of postoperative cognitive function with both drugs. Dexmedetomidine and esmolol are safe drugs for induced hypotension as rScO2 values are well maintained during hypotension with better safety of dexmedetomidine over esmolol which had more incidences of intraoperative CDEs.
Conflict of interest
None.
Notes
Available online 18 October 2014
References
- LauchlanChambersThomasKremenChristopher J.SnellSeth C.GamradtArthroscopic anterior shoulder stabilization in the beach chair position using trans-subscapularis drilling of the 5:30 anchorTech Should Surg1220115661
- M.T.ProvencherE.S.McIntireT.M.GastonAvoiding complications in shoulder arthroscopy: pearls for lateral decubitus and beach chair positioningTech Shoulder Elbow Surg11201013
- P.E.GelberF.ReinaE.CaceresJ.C.MonllauA comparison of risk between the lateral decubitus and the beach-chair position when establishing an anteroinferior shoulder portal: a cadaveric studyArthroscopy232007522528
- D.D.RainsG.A.RookeC.J.WahlPathomechanisms and complications related to patient positioning and anesthesia during shoulder arthroscopyArthroscopy272011532541
- C.PerutoM.CiccottiS.CohenShoulder arthroscopy positioning: lateral decubitus versus beach chairArthroscopy252009891896
- D.S.MorrisonR.K.SchaeferR.L.FriedmanThe relationship between subacromial space pressure, blood pressure, and visual clarity during arthroscopic subacromial decompressionArthroscopy111995557560
- A.PohlD.J.CullenCerebral ischemia during shoulder surgery in the upright position: a case seriesJ Clin Anesth172005463469
- M.T.BhattiF.K.EnnekingVisual loss and ophthalmoplegia after shoulder surgeryAnesth Analg962003899902
- C.S.DegauteControlled hypotension: a guide to drug choiceDrugs67200710531076
- R.VirtanenJ.M.SavolaV.SaanoL.NymanCharacterization of the selectivity, specificity and potency of medetomidine as an alpha2 adrenoceptor agonistEur J Pharmacol1501–21988914
- P.P.LakhlaniL.B.MacMillanT.Z.GuoB.A.McCoolD.M.LovingerM.MazeL.E.LimbirdSubstitution of a mutant alpha2a-adrenergic receptor via “hit and run” gene targeting reveals the role of this subtype in sedative, analgesic, and anesthetic-sparing responses in vivoProc Natl Acad Sci USA9418199799509955
- C.ChrysostomouSchmitt CG – dexmedetomidine: sedation, analgesia and beyondExpert Opin Drug Metab Toxicol42008619627
- J.PenttiläA.HelminenM.AnttilaCardiovascular and parasympathetic effects of dexmedetomidine in healthy subjectsCan J Physiol Pharmacol822004359362
- A.CasatiG.FanelliP.PietropaoliR.ProiettiR.TufanoS.MontaniniMonitoring cerebral oxygen saturation in elderly patients undergoing general abdominal surgery: a prospective cohort studyEuropean Journal of Anaesthesiology2420075965
- G.W.FischerT.M.TorrilloM.M.WeinerM.A.RosenblattThe use of cerebral oximetry as a monitor of the adequacy of cerebral perfusion in a patient undergoing shoulder surgery in the beach chair positionPain Pract92009304307
- P.W.McCormickM.StewartM.G.GoettingNoninvasive cerebral optical spectroscopy for monitoring cerebral oxygen delivery and hemodynamicsCrit Care Med221991596602
- H.L.EdmondsMulti-modality neurophysiologic monitoring for cardiac surgeryHeart Surg Forum52002225228
- A.CasatiE.SpreaficoM.PutzuG.FanelliNew technology for noninvasive brain monitoring: continuous cerebral oximetryMinerva Anestesiol722006605625
- J.M.MurkinS.J.AdamsR.J.NovickMonitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective studyAnesth Analg10420075158
- A.CasatiG.FanelliP.PietropaoliContinuous monitoring of cerebral oxygen saturation in elderly patients undergoing major abdominal surgery minimizes brain exposure to potential hypoxiaAnesth Analg1012005740747
- M.FolsteinS.FolsteinP.McHughMini Mental State. A practical method for grading the cognitive state of patients for clinicianJ Psychiatr Res121975 189–9
- A.CasatiG.AldegheriE.VinciguerraRandomized comparison between sevoflurane anaesthesia and unilateral spinal anaesthesia in elderly patients undergoing orthopaedic surgeryEur J Anaesthesiol202003640646
- A.PapadonikolakisE.R.WieslerM.A.OlympioG.G.PoehlingAvoiding catastrophic complications of stroke and death related to shoulder surgery in the sitting positionArthroscopy242008481482
- J.J.SmithC.M.PorthM.EricksonHemodynamic response to the upright postureJ Clin Pharmacol341994375386
- JM.PorterC.PidgeonAJ.CunninghamThe sitting position in neurosurgery: a critical appraisalBr J Anaesth821999117128
- W.BuhreA.WeylandK.BuhreS.KazmaierK.MurschM.SchmidtM.SydowH.SonntagEffects of the sitting position on the distribution of blood volume in patients undergoing neurosurgical proceduresBr J Anaesth842000354357
- G.FuchsG.SchwarzA.KulierG.LitscherThe influence of positioning on spectroscopic measurements of brain oxygenationJ Neurosurg Anesthesiol1220007580
- K.TangeH.KinoshitaT.MinonishiN.HatakeyamaN.MatsudaM.YamazakiY.HatanoCerebral oxygenation in the beach chair position before and during general anesthesiaMinerva Anestesiol762010485490
- S.Z.LangerPresynaptic regulation of the release of catecholaminesPharmacol Rev321980337362
- F.RichaA.YazigiG.SleilatyP.YazbeckComparison between dexmedetomidine and remifentanil for controlled hypotension during tympanoplastyEur J Anaesthesiol252008369374
- H.BasarS.AkpinarN.DoganciU.BuyukkocakC.KaymakO.SertThe effect of preanaesthetic single dose dexmedetomidine on induction, hemodynamic and cardiovascular parametersJ Clin Anesth202008431436
- D.L.BloweyAnihypertensive agents: mechanism of action, safety profiles, and current uses in childrenCurr Ther Res Clin Exp622001298313
- C.S.DegouteM.J.RayM.ManchonC.DubreuilV.BanssillonRemifentanil and controlled hypotension; comparison with nitroprusside or esmolol during tympanoplastyCan J Anaesth4820012027
- D.TimperleyR.SacksR.J.ParkinsonR.J.HarveyPerioperative and intraoperative maneuvers to optimize surgical outcomes in skull base surgeryOtolaryngol Clin North Am432010699730
- PH.PetrozzaInduced hypotensionInt Anesth Clin281990223229
- J.C.DrummondA.R.HargensP.M.PatelHydrostatic gradient is important: blood pressure should be correctedAPSF Newslett2420096
- Glenn S.MurphyJoseph W.SzokolJesse H.MarymontSteven B.GreenbergMichael J.AvramJeffery S.VenderJessica.VaughnBAMargaritaNismanCerebral oxygen desaturation events assessed by near-infrared spectroscopy during shoulder arthroscopy in the beach chair and lateral decubitus positionsAnesth Analg1112010496505
- S.H.KoY.W.ChoS.H.ParkJ.G.JeongS.M.ShinG.KangCerebral oxygenation monitoring of patients during arthroscopic shoulder surgery in the sitting positionKorean J Anesthesiol632012297301
- M.PraneviciusO.PraneviciusModified calculation of the cerebral perfusion pressure in a sitting position: jugular Starling resistor and related clinical implicationsAPSF Newsletter2320083233
- A.FassoulakiH.KaliontziG.PetropoulosA.TsarouchaThe effect of desflurane and sevoflurane on cerebral oximetry under steady-state conditionsAnesth Analg102200618301835
- J.D.TobiasCerebral oxygenation monitoring: near-infrared spectroscopyExpert Rev Med Dev32006235243
- A.D.McLeodF.IgielmanC.ElwellMeasuring cerebral oxygenation during normobaric hyperoxia: a comparison of tissue microprobes, near-infrared spectroscopy and jugular venous oximetry in head injuryAnesth Analg972003851856
- P.J.KirkpatrickP.SmielewskiM.CzosnykaNear-infrared spectroscopy use in patients with head injuryJ Neurosurg831995963
- J.H.LeeK.T.MinY.M.ChunE.J.KimS.H.ChoiEffects of beachchair position and induced hypotension on cerebral oxygen saturation in patients undergoing arthroscopic shoulder surgeryArthroscopy272011889894
- H.EndohT.HondaS.OhashiThe influence of nicardipine, nitroglycerin and prostaglandin E1 induced hypotension on cerebral pressure autoregulation in adult patients during propofol–fentanyl anesthesiaAnesth Analg942002169173
- WolfgangHeinkeStefanZyssetMargretHund-GeorgiadisDerkOlthoffD.Yves von CramonThe effect of esmolol on cerebral blood flow, cerebral vasoreactivity, and cognitive performance: a functional magnetic resonance imaging studyAnesthesiology10220054150
- C.DippmannS.WingeH.B.NielsenSevere cerebral desaturation during shoulder arthroscopy in the beach-chair positionArthroscopy262010S148150
- D.J.FriedmanN.Z.ParnesZ.ZimmerL.D.HigginsJ.J.WarnerPrevalence of cerebrovascular events during shoulder surgery and association with patient positionOrthopedics322009256
- D.SalazarB.SearsB.AghdasiA.OnlyA.FrancoisP.ToninoG.MarraCerebral desaturation events during shoulder arthroscopy in the beach chair position: patient risk factors and neurocognitive effectsJ Shoulder Elbow Surg201310.1016/j.jse.2012.12.036 Epub ahead of print
- C.D.KurthJ.C.McCannJ.WuL.MilesA.W.LoepkeCerebral oxygen saturation-time threshold for hypoxic–ischemic injury in pigletsAnesth Analg108200912681277
- P.L.MadsenH.B.NielsenP.ChristiansenWell-being and cerebral oxygen saturation during acute heart failure in humansClin Physiol2022000158164
- M.B.KimD.S.WardC.R.CartwrightEstimation of jugular venous O2 saturation from cerebral oximetry or arterial O2 saturation during isocapnic hypoxiaJ Clin Monit Comput1632000191199
- I.IglesiasJ.M.MurkinD.BainbridgeS.AdamsMonitoring oxygen saturation significantly decreases postoperative length of stay: a prospective randomised blinded studyHeart Surg Forum62003204
- S.K.SamraE.A.DyK.WelchP.DorjeG.B.ZelenockJ.C.StanleyEvaluation of a cerebral oximeter as a monitor of cerebral ischemia during carotid endarterectomyAnesthesiology932000964970
- A.RigamontiM.ScandroglioF.MinicucciS.MagrinA.CarozzoA.CasatiA clinical evaluation of near-infrared cerebral oximetry in the awake patient to monitor cerebral perfusion during carotid endarterectomyJ Clin Anesth172005426430
- A.C.te Winkel-WitloxM.W.PostJ.M.Visser-MellyE.LindemanEfficient screening of cognitive dysfunction in stroke patients: Comparison between the CAMCOG and the R-CAMCOG, mini mental state examination and functional independence measure-cognition scoreDisabil Rehabil30200813861391
- P.Williams-RussoN.E.SharrockS.MattisRandomized trial of hypotensive epidural anesthesia in older adultsAnesthesiology911991926
- B.D.TownesS.S.DikmenS.W.BledsoeNeuropsychological changes in a young, healthy population after controlled hypotensive anesthesiaAnesth Analg651986955