Abstract
Objectives
The purpose of our study was to evaluate the prophylactic use of low dose ketamine and comparing it to dexamethasone for reducing intraoperative nausea and vomiting (IONV) during cesarean section under spinal anesthesia.
Methods
The study was performed in 135 full term parturient women of ASA I & II (American Society of Anesthesiology Grade I & II), aged between 20 and 40 years with uncomplicated pregnancies. The group I (n = 45) received 0.4 mg/kg ketamine, group II (n = 45) received 8 mg dexamethasone while control group III (n = 45) received 5 ml normal saline, slowly IV immediately after spinal anesthesia and before surgical incision. The number of episodes of nausea and vomiting was recorded, as well as any other adverse effects.
Results
The results of this study showed that the rate of nausea and vomiting was lower in patients who received 0.4 mg/kg ketamine and 8 mg dexamethasone than in the placebo group with significant reduction in hypotensive episodes in ketamine group (P = 0.02).
Conclusion
Low dose ketamine is effective as dexamethasone in prevention of IONV during cesarean section under spinal anesthesia.
1 Introduction
Nausea and vomiting is seen in almost 80% of the patients undergoing cesarean section (CS) under regional anesthesia [Citation1–Citation3]. Many factors may contribute to this high rate of IONV during CS; sympathetic block and the resultant hypotension secondary to spinal anesthesia, visceral pain and vagal stimulation during CS probably the most important factors [Citation4]. Dexamethasone is an effective antiemetic agent with minimal side effects after single dose administration. [Citation5]. Ketamine has unique central sympatho-mimetic, vagolytic and analgesic properties [Citation8]. These effects of ketamine are assumed to reduce the incidence of spinal induced hypotension and consequently nausea and vomiting. In this study, we aimed to compare the antiemetic efficacy of low dose ketamine and dexamethasone to decrease the incidence of IONV during CS under spinal anesthesia.
2 Patients and methods
After obtaining approval from the clinical research ethics committee of Al-Minia University, all participants provided a written informed consent. This randomized, prospective, double blind, study was performed on 135 ASA physical status I–II female patients, between 20 and 40 years of age undergoing a planned CS under spinal anesthesia. We exclude patients with, preeclampsia, eclampsia, psychiatric disorder, a gastrointestinal disease, drug allergies, infection, diabetes, glaucoma, epileptic patients, and those on antiemetic agent in the last 24 h. All parturients received 1000 ml lactated Ringer solution IV over 30 min before spinal injection. Patients connected to standard monitoring includes electrocardiogram, noninvasive arterial blood pressure measurement and pulse oximetry (MARQUERR, SOLAR 8000, Patient monitor, UK). Spinal anesthesia performed using a 25-gauge spinal needle (GHATWARY MEDICAL SUPPLY, EGYPT), while the patient is in the sitting position, through the L3-4, L4-5 or L2-3 interspace 2.2–2.8 ml (depending on patients height) of 0.5% heavy marcaine (Marcaine Spinal Heavy Ampul 0.5%, Astrazeneca) was administered to the subarachnoid space. Parturients were moved to supine position with operation table turned 15–20 deg left lateral tilt to decrease the aortocaval compression caused by the uterus and reducing hypotension after spinal anesthesia. The parturients were allocated randomly to three groups, ketamine group (n = 45) received 0.4 mg/kg ketamine diluted in 5 ml normal saline, dexamethasone group (n = 45) received 8 mg dexamethasone diluted in 5 ml normal saline and control group (n = 45) received 5 ml normal saline, the three syringes were given by the second anesthetist to the anesthetist who was unaware of the content of the syringe and would administer it in a double-blind fashion slowly IV over 1 min before surgical incision. Face mask oxygenation used to all patients at a rate of 2–3 L/min, the level of sensory blockage was evaluated by pinprick test before the surgical incision, and the level of blockade was determined. We exclude from the study Patients in whom the level of analgesia was insufficient, and were given general anesthesia. Estimated fluid deficits and maintenance requirements were replaced with lactated Ringer’s solution IV, intraoperative hypotension (MABP less than 20% of the basal reading) was managed by increasing the infusion rate of Ringer lactate solution with injecting increments of 3 mg ephedrine hydrochloride IV and if hypotension persists another ephedrine bolus was given. Bradycardia (HR < 50 beat/min) managed by atropine sulfate (0.5 mg). After delivery of the baby, routine use of 10 units oxytocin IV and 0.2 mg ergometrine IM were given to all parturient to enhance uterine contraction. We recorded the incidence of hypotension (percentage per each group) and increments of ephedrine hydrochloride in mg. During the intraoperative period, nausea, retching and vomiting episodes were recorded by an anesthetist who was blinded to the drug administered to the patient, questioning the patient in every 3 min about these emetic symptoms, the patient was also requested to report the symptoms that occur at the intervals. Vomiting was managed by metoclopramide 10 mg slowly IV, and analgesic requirements (fentanyl) 20–50 μg that injected IV when needed after delivery of the baby and the amount recorded. A standardized surgical technique was used in all cesarean section’s except for the tubal ligation procedure performed in some but not all of the cases. Ramsay Sedation Scale (RSS; 1 = anxious and agitated, 2 = co-operative and tranquil, 3 = drowsy but responsive to command, 4 = asleep but responsive to glabellar tap, 5 = asleep with a sluggish response to tactile stimulation, 6 = asleep and no response). It was used to measure sedation level at 5, 10, 20, and 30 min after surgical incision.
2.1 Statistical analysis
The statistical analysis was done using SPSS program statistical package for social science version 16 (SPSS Inc., Chicago, USA). At two-tailed significance level of 0.05% and power of 80%, it was calculated that a minimum sample size of 43 patients in each group was required to achieve 30% reduction in the total incidence of intraoperative nausea and vomiting (from 60% to 30%), thus 45 patients were enrolled in the present study to receive each drug for prevention of intraoperative nausea and vomiting. Data values were expressed as frequency (%) or means ± standard deviation (SD), as appropriate. Student t-test was used to compare between three groups of normally distributed data. Chi square test was used for qualitative data. Mann–Whitney test was used to compare three groups of non parametric data. P-value was significant if it is <0.05.
3 Results
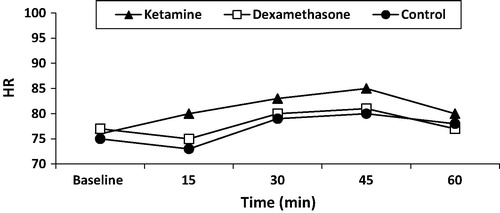
There were no statistically significant differences in age, height, weight, gestational age, history of PONV, history of vertigo or baseline hemodynamics between the studied three groups (). We exclude three cases from the study due to incomplete block (below T10) one in each group. Intraoperatively, there were no differences in anesthesia time, operating time, total ephedrine administered (the average amount in those who suffered hypotension and received ephedrine), total fentanyl administered (average for each patient), hypotensive episodes (number of patients who suffered from hypotension) between ketamine and dexamethazone groups, while the control group showed a significant high dose of total ephedrine administrated when compared to ketamine and dexamethazone groups (8 ± 3.2 versus 4.5 ± 2.1 in ketamine group, and 5.3 ± 2 in dexamethazone group), and a significant high rate of hypotensive episodes when compared to ketamine group (84.4% versus 64%) (). There was statistically insignificant increase in the rate of successful prevention of IONV in ketamine group when compared to dexamethazone group (77.8% versus 71.2%). The incidence of only nausea (13.3% with ketamine versus 17.7% with dexamethazone), and the incidence of only vomiting (8.9% with ketamine versus 11.1% with dexamethazone) were statistically insignificant when compared between both groups. The total incidence of intraoperative nausea and vomiting was 22.2% in the ketamine group compared with 28.8% in the dexamethazone group, which was statistically insignificant. The number of patients who required rescue antiemetics in the ketamine group compared with dexamethazone group (6.7% versus 8.8%; P = 0.69) was not statistically significant. The control group showed a significant high incidence of IONV (51.1%) and a significant low incidence of successful prevention of IONV (48.9%) when compared to ketamine or dexamethazone group (). There was a significant increase in Ramsey sedation score in ketamine group when compared to dexamethazone group and control group at 10, 20 and 30 min after surgical incision (). The studied groups were comparable as regard to mean arterial blood pressure and heart rate, there was no statistically significant difference between groups during the study period ( and ), also the studied groups were comparable as regard to the highest sensory level reached after spinal injection (T4) and the remaining not below (T10).
Table 1 Baseline maternal characteristics.
Table 2 Operative details.
Table 3 Comparison of the emetic symptoms during intraoperative period in the studied groups.
Table 4 Ramsey sedation score (RSS) in the studied groups.
4 Discussion
IONV is distressing for patients, obstetricians, anesthetists, and may increase the risk of visceral injury during surgery by involuntary uncontrolled abdominal movements. The precise etiology of IONV remains unknown and various factors have been implicated [Citation10]. Hypotension is probably the most important cause of IONV that occurs during CS under spinal anesthesia. Hypotension can induce the emetic symptoms by leading to cerebral hypoperfusion [Citation11]. Prevention of hypotension is therefore important for the prevention of IONV. We tried to take the necessary measures to prevent hypotension in all of our patients by preload, left uterine tilt, increasing rate of fluid infusion and increments of ephedrine when necessary. Our double blind study demonstrated that CSs performed under spinal anesthesia using 0.4 mg ketamine as a single agent for the control of IONV is as effective as 8 mg intravenous dexamethasone with no increase in the side effect profile. The mechanism for the antiemetic effect of dexamethasone has been incompletely understood but it is thought to be caused by the inhibition of prostaglandin synthesis, by showing anti-inflammatory efficacy and by causing a decrease in the release of endogenous opiates [Citation6,Citation7]. Several studies investigates different medications to reduce IONV in parturients undergoing CS under spinal anesthesia, Fujii and his colleagues [Citation12] investigated the preventive effect of IV granisetron 3 mg, some studies compared the antiemetic efficacy of dexamethasone for the prevention of PONV with other agents, or the efficacy of combining metoclopropamide 10 mg, droperidol 1.25 mg against placebo; they found that the three drugs were similarly effective in reduction of intraoperative nausea compared to placebo effect (P value = 0.001). dexamethasone with other antiemetic agents for the same purpose. D’Souza et al. compared dexamethasone with ondansetron for the prevention of PONV after laparoscopic gynecologic surgery and found that dexamethasone decreased the incidence of PONV and use of single dose of dexamethasone was safe and could be alternative to single dose ondansetron [Citation13]. In agreement of previous studies our study demonstrates significant reduction in IONV in dexamethasone group than placebo (P value = 0.03). Ketamine is an intravenous dissociative anesthetic agent related to phencyclidine group which works by antagonizing N-methyl d-aspartate (NMDA) receptors [Citation8]. Few studies examined the effect of a ketamine on the incidence of nausea and vomiting during cesarean section by spinal anesthesia The sympatho-mimetic and vagolytic properties of ketamine encouraged us to examine its effects on IONV and compare it to dexamethasone which examined by many author. Ure D, et al. studied the effect of glycopyrolate in prevention of intraoperative nausea during CS relying on its vagolytic effect, the incidence of IONV reduced from 68% in the placebo group to 42% in the glycopyrolate group [Citation14]. Shabana et al. studied the effect of 0.5 mg/kg ketamine on IONV, they showed significant reduction (P value 0.004) in nausea in the ketamine group compared with placebo group, also showed statistically insignificant reduction in vomiting in ketamine versus placebo group (2.3% versus 4.6%) [Citation15], and the majority of hypotensive episodes occurs during the infusion time of ketamine. In our study we started by three pilot cases of 0.5 mg/kg ketamine injection but we found RSS of the three cases is 4 in first 10 min, we reduced the dose of ketamine to 0.4 mg/kg to avoid high RSS, shorten the duration of drug infusion and avoid any side effects. In agreement to our view some blood-borne toxins and drugs stimulate an area in the medulla which is called chemoreceptor trigger zone (CTZ). This zone communicates with the vomiting center, to initiate vomiting [Citation9]. It should be noted that if the CTZ was stimulated, its deactivation would be difficult [Citation10], so we decided to start injection of studied drugs early, in contrast to many lecturers that started antiemetics after umbilical cord clamping. In our study the rate of successful prevention of IONV in ketamine group when compared to dexamethazone group (77.8% versus 71.2%) which was statistically insignificant, but significant reduction in both groups when compared with control group (48.9%). Total amount of ephedrine and hypotensive episodes was greater in control group than in studied drugs, and the hypotensive episodes in ketamine group insignificantly less than in dexamethasone group because of sympathomimetic and vagolytic effect of ketamine. There was a significant increase in Ramsey sedation score in ketamine group when compared to dexamethazone group and control group at 10, 20 and 30 min after surgical incision, only one parturient in ketamine group gain RSS 4 at 10 min. In conclusion; the current study demonstrated that direct IV ketamine 0.4 mg/kg is effective as 8 mg dexamethasone in prevention of IONV in parturients subjected to elective CS under spinal anesthesia and associated with reduction in the incidence of hypotensive episodes compared to placebo group.
Conflict of Interest
None.
Notes
Available online 19 October 2014
References
- S.A.LussosA.M.BaderM.L.ThornhillS.DattaThe antiemetic efficacy and safety of prophylactic metoclopramide for elective cesarean delivery during spinal anesthesiaReg Anesth171992126130
- A.SantosS.DattaProphylactic use of droperidol for control of nausea and vomiting during spinal anesthesia for cesarean sectionAnesth Analg6319848587
- D.HarmonM.RyanA.KellyM.BowenAcupressure and prevention of nausea and vomiting during and after spinal anaesthesia for caesarean sectionBr J Anaesth842000463467
- M.F.WatchaP.F.WhitePostoperative nausea and vomiting: its etiology, treatment, and preventionAnesthesiology771992162
- J.I.TzengJ.J.WangS.T.HoDexamethasone for the prophylaxis of nausea and vomiting after epidural morphine for post-caesarean section analgesia: a comparison of droperidol with salineBr J Anaesth85200014
- M.WattwilS.E.ThornA.LovqvistDexamethasone is as effective as ondansetron for the prevention of postoperative nausea and vomiting following breast surgeryActa Anaesthesiol Scand472003823827
- K.HolteH.KehletPerioperative single-dose glucocorticoid administration: pathophysiologic effects and clinical implicationsJ Am Coll Surg1952002694712
- E.J.MorganM.S.MikhailJ.MurrayNonvolatile anesthetic agents, clinical anesthesiology4th ed., vol. 12006Lange Medical Books/McGraw-Hill179204 [chapter 8]
- C.C.ApfelPostoperative nausea and vomitingR.D.MillerL.I.ErikssonL.A.FleisherJ.P.Wiener-KronishW.L.YoungMiller’s anesthesia7th ed., vol. 22009Churchill Livingstone/Elsevier [chapter 86]
- C.F.FanE.TanhuiS.JoshiAcupressure treatment for prevention of postoperative nausea and vomitingAnesth Analg8441997821825
- M.BalkiJ.C.CarvalhoIntraoperative nausea and vomiting during cesarean section under regional anesthesiaInt J Obst Anesth142005230241
- Y.FujiiH.TanakaH.ToyookaPrevention of nausea and vomiting with granisetron, droperidol and metoclopramide during and after spinal anaesthesia for caesarean section: a randomized, double-blind, placebo-controlled trialActa Anaesthesiol Scand421998921925
- N.D’SouzaM.SwamiS.BhagwatComparative study of dexamethasone and ondansetron for prophylaxis of postoperative nausea and vomiting in laparoscopic gynecologic surgeryInt J Gynaecol Obstet1132011124127
- D.UreK.S.JamesM.McNeillGlycopyrrolate reduces nausea during spinal anaesthesia for caesarean section without affecting neonatal outcomeBr J Anaesth821999277279
- A.M.ShabanaE.S.NasrH.E.MoawadEffect of ketamine on intraoperative nausea and vomiting during elective caesarean section under spinal anaesthesiaEgypt J Anaesth282012169174