Abstract
Purpose
Tracheobronchopathia osteochondroplastica (TO) also known as tracheopathia chondro-osteoplastica, is a rare benign chronic disease of undetermined etiology usually involving the trachea and bronchi. We describe the case of a 40-year-old male with carcinoma colon with difficult intubation who was later diagnosed to have TO. Previously also TO has been reported with carcinoma colon. Whether this is an incidental finding or the two have any correlation remains to be deciphered.
Clinical features
The patient had no previous symptoms despite the presence of extensive endotracheal lesions. The patient had to be intubated with a tube that was several sizes smaller for his height and weight. Subsequent intraoperative and postoperative period was uneventful. The diagnosis of TO was confirmed by subsequent radiological and histopathological examination.
Conclusion
Awareness of this entity and its anticipation in patients with colorectal carcinoma may help anesthetists to manage similar cases appropriately in the future. Also it shall help in future research being directed to this condition.
1 Introduction
Tracheobronchopathia osteochondroplastica (TO) is a rare disorder with overgrowth of tracheal cartilage and sometimes associated with ossification into the lumen of the trachea and bronchi. The etiology of the disease is unknown. Although this disorder is usually discovered as an incidental finding during intubation or radiological imaging, multiple cases have been described with various malignancies especially colorectal carcinoma [Citation1,Citation2]. No significant anesthetic complications have been described with this condition except for difficult intubation. TO has been repeatedly described in the literature as a benign entity. Its etiopathogenesis however remains unclear. Whether there is any association with malignancies or due to confounding factor like smoking is not known but it is important for the anesthetist to be aware of this condition presenting as difficult intubation especially in patients with colorectal carcinoma.
2 Case report
A 40-year-old, 50 kg, male patient, chronic smoker presented with complaint of hematochezia for last 6 years with severe anemia. Patient was investigated and diagnosed to have carcinoma colon. He was planned to be taken up for right hemicolectomy and ileotransverse anastomosis for carcinoma colon after multiple blood transfusions. He had no other known comorbid illness and there was no history of any previous surgery. There were no respiratory signs or symptoms and no abnormality was detected in posterior–anterior view of chest X-ray ((a)). All other routine investigations were also within normal limits with hemoglobin of 8.5 g/dl on the day of surgery.
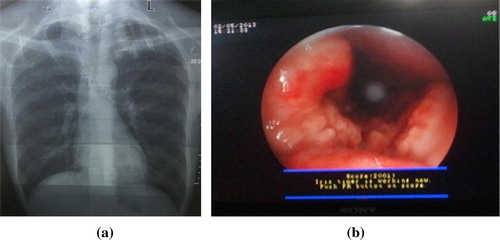
The patient was taken up for surgery under standard anesthesia monitoring (NIBP, ECG and SPO2). Anesthetic plan included epidural block plus general anesthesia. An epidural catheter was placed at 10 cm at T12–L1 level in lateral position to facilitate postoperative analgesia. Then patient’s position was made supine and patient was induced with O2, fentanyl 100 μg, propofol 100 mg and atracurium 25 mg. After this an arterial line was placed in right radial artery for FloTrac-Vigileo™ (Edward Lifesciences, Irvine, CA, USA) monitor guided fluid therapy by measuring stroke volume variation (SVV). After induction and mask ventilation, direct laryngoscopy was done on which Cormack-lehane grading appeared 2a with clear visibility of vocal cords. During endotracheal intubation, we found some resistance and could not pass endotracheal tube of size 8.0 mm. Subsequently intubation was tried with serially smaller endotracheal tubes of size 7.5 mm, 7 mm, 6.5 mm and 6 mm but was unsuccessful. The endotracheal tubes could not be passed beyond the glottic opening. Then we tried to pass bougie through trachea on which we felt abnormal gritty sensation. After mask ventilation with O2 again, we were able to insert 3 no. AMBU AuraOnce Disposable Laryngeal Mask (AMBU; AMBU A/S, Denmark) for securing airway. In the meanwhile we called ENT surgeons for help. As there appeared to be some form of obstruction at the infra-glottic level, fiberoptic bronchoscopy was done which revealed multiple nodular excrescences present along the entire length of the trachea occupying almost three-fourths of the tracheal circumference ((b)).
Since the patient was having persistent severe lower gastrointestinal blood losses, the surgery could not be deferred till a definitive diagnosis of the airway condition was made. Intubation was thus attempted with serially smaller tubes and the patient was finally intubated with a 5.5 mm ET tube. Despite a smaller ET tube, we were able to ventilate the patient and his respiratory parameters (i.e. airway pressure, tidal volume) were maintained within normal limits throughout the surgery.
The surgery was completed in 3 h. Blood loss was around 650 ml. 2 PRBC and 1.8 L crystalloids were given intraoperatively. Patient’s hemodynamic status was monitored continuously with FloTrac-Vigileo™ (Edward Lifesciences, Irvine, CA, USA) monitor.
For analgesia epidural infusion of 0.625% bupivacaine with 2 μg/ml fentanyl at the rate of 6 ml/h was given during perioperative period. There was no intraoperative complication subsequently. After completion of the surgery, neuromuscular block was reversed with injection of neostigmine 2.5 mg plus glycopyrrolate 0.4 mg. Then patient was extubated and shifted to AMBU LMA. On LMA patient was electively transferred to the ICU for observation where the LMA was removed. The patient subsequently had good respiratory efforts and there was no evidence of airway obstruction. Postop period was uneventful.
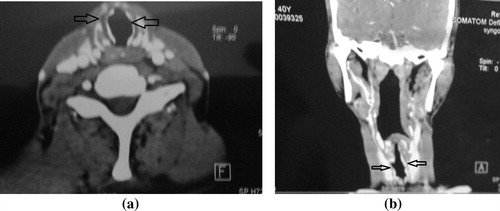
A contrast enhanced computed tomography (CECT) neck was done subsequently which showed tracheal wall calcification of the anterolateral wall with sparing of the membranous part suggestive of “Tracheobronchopathia osteochondroplastica” (). A biopsy of the lesion was also done which was reported as bronchial cartilage with abnormal and unevenly distributed mineralization and it confirmed the diagnosis of TO.
3 Discussion
Tracheobronchopathia osteochondroplastica (TO) is a rare disorder. It has been described as a benign disorder characterized by the presence of hard, white, cartilaginous and or osseous nodules in the tracheobronchial tree, classically sparing the posterior membranous wall. The lesions of TO are located most commonly in the distal two-thirds of trachea and major bronchi, although proximal trachea, lobar and segmental bronchi may be involved. It was first described in 1857 in the autopsy findings of a tuberculosis patient [Citation3]. The cause of the condition is unknown, but several theories have been postulated. Ecchondroses and endochondroses from the tracheal rings, metaplasia of the elastic tissue or a primary localized amyloidosis of the lower respiratory tract that has undergone ossification are the various theories that have been described. However none of these theories have been substantiated.
A possible association with atrophic rhinitis and pharyngitis was found by Harma and Suurkari [Citation4]. Our patient gave no history suggestive of allergic rhinitis.
The condition is usually asymptomatic and hence the exact estimates of its prevalence are not known. In one study the prevalence was reported as four out of 550 bronchoscopies [Citation5]. In symptomatic patients the symptoms reported include chronic cough, hemoptysis and dyspnea.
The prognosis of TO is usually satisfactory and relies upon the size and site of the lesions. Progressive lesions may lead to obstructive pneumonitis and atelectasis due to airway blockage. Initially conservative treatment in the form of antibiotics for intermittent infection of respiratory tracts is commenced. In case of failure of conservative management, surgical treatment is mandatory. Numerous surgical modalities including laser ablation, mechanical debulking, resection of the involved airway, partial laryngectomy and bronchoscopic removal of lesions have been used [Citation6–Citation8].
Case reports of TO as an incidental finding on intubation or a cause of difficult intubation are being reported [Citation2,Citation6,Citation7]. One of the cases was so severe that a size 4.0 microlaryngoscopy tube was eventually passed over a bougie that had been placed through a rigid bronchoscope [Citation6]. In this case, the lesion was removed with a carbon dioxide laser before the patient was extubated the following day. Several cases of TO have been described associated with various malignancies including two with colorectal carcinoma. In one case TO was diagnosed incidentally on CT in a patient who had previously undergone a hemicolectomy for colorectal carcinoma [Citation1].
At present it is not clear whether this is an incidental finding or there is any etiopathological correlation between these conditions. Till such time that more case reports are brought forward and more studies are done into the etiopathogenesis of this condition, the urgency of the surgery and the severity of the condition guide the management of the patient. In one case report surgery scheduled under general anesthesia was canceled as intubation had been impossible and anesthesia induction was reversed [Citation9]. Awareness of this entity and its anticipation in patients with colorectal carcinoma may help anesthetists to manage similar cases appropriately in the future [Citation10]. Also it shall help in future research being directed to this condition.
Implication statement
Tracheobronchopathia osteochondroplastica, a known cause of difficult intubation was found during surgery in a patient with carcinoma colon. Whether this is an incidental finding or the two have any correlation remains to be deciphered.
Note: Informed written consent to publication was obtained from the patient for this case report.
Financial support
None.
Conflict of interest
No conflict of interest.
Notes
Available online 19 January 2015
References
- KamleshMohanStephenOwenCheeYeongTracheobronchopathia osteochondroplastica as an incidental findingAsian Cardiovasc Thorac Ann1232004280281
- D.ThomasC.StonellK.HasanTracheobronchopathia osteoplastica: incidental finding at tracheal intubationBr J Anaesth8732001515517
- S.WilksOssific deposits on the larynx, trachea and bronchiTrans Pathol Soc Lond8185788
- R.A.HarmaS.SuurkariTracheopathia chondro-osteoplastica: a clinical study of 30 casesActa Otolaryngol841977118123
- G.PrimerTracheobronchopathia osteochondroplasticaPrax Klin Pneumol33197910601063
- A.R.BirzgalisW.T.FarringtonL.O’KeefeJ.ShawLocalised tracheopathia osteoplastica of the subglottisJ Laryngol Otol1071993352353
- D.C.SmithR.PillaiC.E.GillbeTracheopathia osteochondro plastica: a cause of unexpected difficulty in tracheal intubationAnaesthesia421987536538
- DutauHerveMusaniAliI.Treatment of severe tracheobronchopathia osteochondroplasticaJ Bronchol Intervent Pulmonol1132004182185
- Ahmad.TadjeddeinZhamak.KhorgamiHamed.AkhlaghiTracheobronchopathia osteoplastica: cause of difficult tracheal intubationAnn Thorac Surg81200614801482
- M.A.WarnerD.H.ChestnutG.ThompsonM.BottcherD.TobertM.NofftzTracheobronchopathia osteochondroplastica and difficult intubation: case report and perioperative recommendations for anesthesiologistsJ Clin Anesth2582013659661