Abstract
Background
Emergence agitation is a frequent postoperative problem in pediatric patients undergoing adenotonsillectomy. The incidence of EA is wide ranging in the literature from 10% to 80%.
Objective
The aim of this study was to assess the effect of dexmedetomidine in decreasing emergence agitation associated with sevoflurane in children after adenotonsillectomy.
Design
A prospective randomized study.
Setting
King Fahad military hospital, Saudi Arabia.
Methods
The study included 150 patients, classified randomly into two groups and received either sevoflurane or sevoflurane with dexmedetomidine. The Pediatric Anesthesia Emergence Delirium Scale (PAED) was used to assess the emergence agitation. If the PAED scale was ⩾16, the patient was considered agitated.
Results
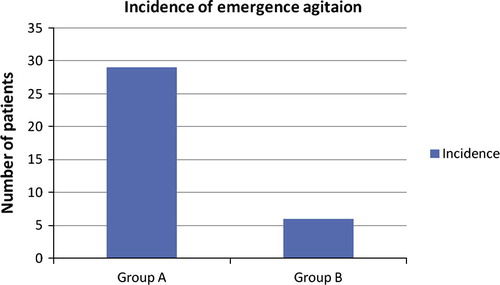
The incidence of emergence agitation was 29 patients in group A (38.66%) and 6 patients (8%) in group B (P < 0.001). Also the comparison of incidence time of agitation, nausea and vomiting and time of discharge from post-anesthesia care unit between the two groups was significant (P < 0.05).
Conclusion
Dexmedetomidine decreased significantly the incidence of agitation with sevoflurane in pediatric patients undergoing adenotonsillectomy and it was associated with a shorter time to extubation, lower incidence of postoperative nausea and vomiting and shorter post-anesthesia care unit length of stay.
Introduction
Emergence agitation (EA) is one of postoperative complications after adenotonsillectomy [Citation1], the incidence of EA is wide ranging in the literature from 10% to 80% [Citation2,Citation3] and the patient exhibits non-purposeful restlessness and agitation, thrashing, crying or moaning, disorientation, and incoherence [Citation4,Citation5].
Although it occurs for short duration, it may require pharmacological intervention, resulting in a prolonged post-anesthesia care unit stay. Its etiology is unclear and factors such as pain, rapid recovery, premedication, gender, age, preoperative anxiety and type of surgery have been suggested [Citation6,Citation7].
Sevoflurane is the most popular inhaled anesthetic agent in pediatric anesthesia. It is a smooth induction drug, which allows a safe and pleasant mask induction, provides fast recovery and impairs less cardiovascular function. Emergence from sevoflurane anesthesia is often associated with agitation in small children [Citation8].
Multiple medications including ketamine, propofol, clonidine, and opioids have been used effectively to prevent EA. However, these medications may increase sedation after anesthesia, cause slow awakening, and in some cases are associated with undesirable side effects, such as nausea and vomiting [Citation9].
Dexmedetomidine is a potent, selective α 2-adrenergic agonist. It can affect the brain and spinal cord α 2-adrenergic receptor, inhibition of neural discharge to produce sedative, analgesic, and anxiolytic effects. The Locus Coeruleus is a verified key part of the brain responsible for the regulation of arousal and sleep. Dexmedetomidine affects the brainstem locus coeruleus α 2-adrenergic receptors and produces sedative, hypnotic, and anxiolytic effects and it has also anesthetic-sparing effects without significant respiratory depression [Citation10–Citation12].
The aim of the study was to assess the role of dexmedetomidine on incidence of emergence agitation in children anesthetized with sevoflurane and undergoing adenotonsillectomy.
Methods
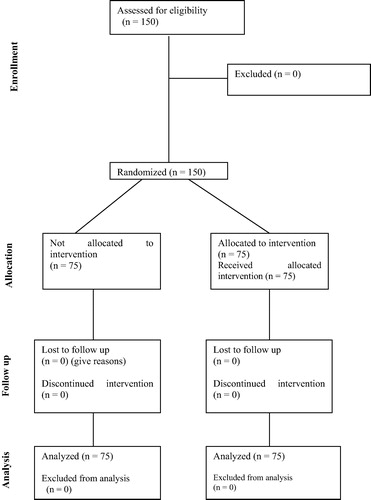
After approval from the local ethics committee and obtaining written informed parental consent in King Fahad military hospital, Khamis Mushait, Saudi Arabia, a study included 150 children, (age 4–14 year, ASA physical status I–II) who underwent elective outpatient adenotonsillectomy (June 2012–July 2014). Exclusion criteria were known allergy to the study medications, developmental delay, mental retardation, attention deficit/hyperactivity disorders, use of psychiatric medications, liver, renal, cardiac or respiratory diseases. In the preoperative waiting area, local anesthetic EMLA cream was used and after 30 min, intravenous line was inserted. The patients did not receive any premedications and were transferred to operative room; after attaching the monitors to patients, intravenous anesthetic induction was done by propofol (1–2 mg/kg), fentanyl (2 μg/kg), and rocuronium (0.6 mg/kg); after tracheal intubation, the patients were ventilated mechanically; and then the patients were randomly allocated (using simple randomization) into 2 equal groups (n = 75 each) and anesthesia was maintained with oxygen/air mixture (50:50) in addition to the following:
Group A (control group): the patients received sevoflurane 1–3% during the surgery.
Group B (dexmedetomidine group): the patients received sevoflurane and dexmedetomidine as an initial loading dose of 0.5 μg/kg (started after induction of anesthesia) over 10 min followed by intravenous infusion 0.1–0.3 μg/kg/h by a computer controlled infusion pump during the surgery. The loading and maintenance doses of dexmedetomidine were used to minimize its side effects on the heart rate and arterial blood pressure [Citation13,Citation14]. The dose of study medications (sevoflurane and dexmedetomidine) was adjusted to maintain the patient’s hemodynamics (heart rate and mean arterial blood pressure) within 20% of pre-induction values. End-tidal concentrations of sevoflurane were recorded every 5 min during the procedure (Dräger, Fabius GS, Premium Germany). For all patients, fentanyl 1 μg/kg was given a bolus dose as needed (if there was an increase in heart rate and mean arterial blood pressure >20% of pre-induction values) in addition to dexamethasone 0.5 mg/kg as anti-emetic and to decrease upper airway edema and after surgery, paracetamol suppository was given as 30 mg/kg and the anesthetics were discontinued; the oropharynx was suctioned and the patients were extubated when spontaneous breathing was adequate and reversal of muscle relaxants with neostigmine and atropine were performed and then the patients were transferred to the post-anesthesia care unit (PACU), where the observer was blinded about the study medication. In the PACU, fentanyl 1 μg/kg if the patients are complaining pain, requested pain medications, patients with pain score 4 or crying.
Monitoring of patients
Heart rate, noninvasive arterial blood pressure, arterial oxygen saturation (SPO2), end-tidal carbon dioxide (ETCO2), and body temperature were recorded before anesthesia induction and every 5 min during surgery. In the post-anesthesia care unit, the same parameters were monitored every 5 min in addition to Pediatric Anesthesia Emergence Delirium (PAED) Scale to assess the emergence agitation (minimal score is 0 and maximal score is 20 [Citation15]. The degree of emergence agitation is directly increases with the total score) (). In PAED of 16 or more, the child was considered agitated. The pain was assessed using objective pain score (). The observer scored pain every 5 min (none/insignificant pain (1–3), moderate pain (4–6), severe pain (7–10) [Citation16]). Patients with pain score 4 were treated with additional dose of fentanyl. The patients were transferred to the ward according to modified Aldrete score criteria [Citation17].
able 1 Pediatric anesthesia emergence delirium scale [Citation13].
able 2 Objective pain scale for postoperative pain [Citation14].
.1 Sample size calculation
Power analysis was performed using Chi square test for independent samples on frequency of patients complaining of post-operative agitation because it was the main outcome variable in the present study. A pilot study was done before starting this study because there are no available data in the literature for the incidence of postoperative agitation with dexmedetomidine administration. The results of the pilot study showed incidence of postoperative agitation of 10% in dexmedetomidine group, and 30% in control group. Taking power 0.8 and alpha error 0.05, a minimum sample size of 72 patients was calculated for each group. A total of patients in each group (75) were included to compensate for possible dropouts.
The statistical paragraph in material and methods
Data were statistically described in terms of mean ± standard deviation (±SD), median and range, or frequencies (number of cases) and percentages when appropriate. Comparison of numerical variables between the study groups was done using Student’s t test for independent samples. For comparing categorical data, Chi square (X2) test was performed. Exact test was used instead when the expected frequency is less than 5. p Values less than 0.05 were considered statistically significant. All statistical calculations were done using computer program Statistical Package for the Social Science (SPSS; SPSS Inc., Chicago, IL, USA) version 15 for Microsoft Windows.
Results
shows number of patients evaluated and enrolled. All patients have completed the study.
There were no significant differences regarding the demographic data, end-tidal carbon dioxide, arterial oxygen saturation, temperature, total dose of fentanyl, duration of surgery and anesthesia, and modified Aldrete score of patients (P > 0.05) ( and ). The heart rate decreased in both groups after induction but the comparison between the two groups was insignificant (). The decrease in heart rate below 80 bpm was in 5 patients of group A and 7 patients of group B, the comparison was insignificant (P = 0.172) (), and patients were managed with small dose of atropine 0.02 mg/kg. The mean arterial blood pressure decreased after induction in both groups but the comparison between the two groups was insignificant (). The decrease in mean arterial blood pressure below 50 mmHg was in 4 patients of group A and 5 patients of group B and patients were managed with small dose of ephedrine and bolus of fluids and the comparison was insignificant (P = 0.211) (). The end-tidal concentration of sevoflurane was significantly higher in group A than in group B and the mean was 2.23 ± 0.31 in group A patients and 0.82 ± 0.26 in group B patients (P < 0.001) ().
able 3 Demographic data of patients (Mean ± SD, number).
able 4 Intraoperative and postoperative data of patients (Mean ± SD, %, Number, Range, Median).
able 5 Complications related to the study (Mean ± SD, number, Range, Median, Percentage %).
The time to extubation (duration from end of anesthesia until the patients become fully awake and removal of endotracheal tube) between the two groups was significant and the mean was 17.06 ± 3.13 min in group A and 11.28 ± 2.09 min in group B patients (P < 0.001) ].
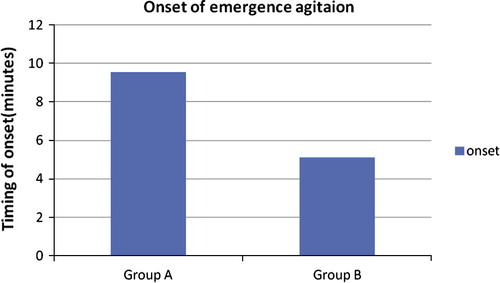
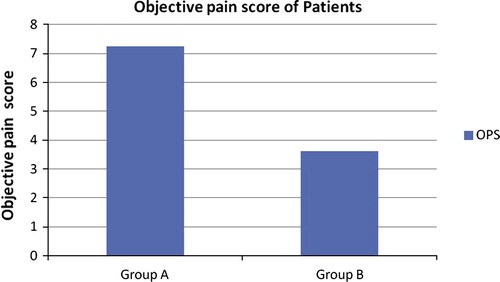
The incidence of emergence agitation was 29 patients (38.66%) in group A and 6 patients (8%) in group B, the comparison was significant between the two groups (P < 0.001) (, ), and patients were managed properly with midazolam 0.1 mg/kg intravenously. The onset of emergence agitation (time of agitation occurrence) was earlier in group A patients than in group B patients and the mean was 9.53 ± 3.82 min in group A and 5.13 ± 2.75 min in group B (P < 0.001) (, ). The objective pain score was higher in group A than in group B and the mean was 7.25 ± 1.19 in group A and 3.61 ± 0.82 in group B patients (P < 0.001) (, ). There was a statistical difference in the fentanyl dose during surgery and in the post-anesthesia care unit between the two groups and the total dose (μg/kg) was lower in group B than in group A patients (P < 0.001) ().
The incidence of nausea and vomiting was 11 patients in group A and 5 patients in group B (P = 0.031) (), and the patients were managed with single intravenous ondansetron dose 0.1 mg/kg.
The comparison of post-anesthesia care unit length of stay was significant and the mean was 43.90 ± 6.72 min in group A and 34.8 ± 4.84 min in group B (P < 0.001) ().
Discussion
The aim of the present study was to assess the effect of dexmedetomidine in decreasing the incidence of emergence agitation in children after adenotonsillectomy under sevoflurane.
The present study showed that the incidence of emergence agitation was 38.66% of group A and only 8% of group B patients and the dexmedetomidine reduced significantly the emergence agitation in children after adenotonsillectomy. In a double-blinded trial, 60 children (age 3–7 years) were randomly assigned to receive dexmedetomidine (0.5 μg/kg) IV or placebo. Sevoflurane was used for induction and maintenance of anesthesia. The incidence and severity of agitation in the dexmedetomidine group were lower than in the placebo group (P < 0.05) [Citation18]. Jia et al. [Citation19], compared sevoflurane and sevoflurane with dexmedetomidine (loading dose of 1 μg/kg followed by 1 μg/kg/Hr) in patients undergoing adenotonsillectomy and found the incidence of agitation decreased significantly with dexmedetomidine (P < 0.05) without any side effect related to dexmedetomidine; another study showed the incidence of emergence agitation was lower in dexmedetomidine group (loading dose of 1 μg/kg followed by 0.1 μg/kg/Hr) than in sevoflurane group (5% vs. 55%, P < 0.001) [Citation20] and the same result was reported by other studies [Citation21,Citation22].
Jin-hui et al. [Citation23], did a meta-analysis study included 27 trials and found the incidence of emergence agitation was as high as 40.3% in placebo group compared to 13.0% in dexmedetomidine group.
In the present study, the onset of agitation was earlier in group A than in group B and the comparison between the two groups was significant. Contrary to the result of the present study, Meng et al. [Citation24] compared sevoflurane and sevoflurane with different doses of dexmedetomidine (loading dose of 0.5 μg/kg or 1 μg/kg followed by 0.2 μg/kg/Hr or 0.4 μg/kg/Hr) and found the onset of agitation was insignificant (P > 0.05). The present study showed the pain score was higher in group A than in group B and dexmedetomidine decreased significantly the pain in group B; therefore, the required fentanyl dose was greatly higher in group A patients and the same result was reported by other studies [Citation18,Citation23,Citation25]. A meta-analysis study evaluated the prevention of EA, and concluded that the analgesia did not seem to play a role in preventing emergence agitation [Citation9], and adding of opioids for analgesia did not prevent the EA and may increase the occurrence of EA [Citation26]. Against to this result, Cohen et al. [Citation27] reported that the use of opioids considerably reduces the incidence of postoperative agitation, but causes nausea and vomiting as the same results of the present study and other studies [Citation21,Citation28], but another study found that no significant difference in incidence of nausea and vomiting between sevoflurane and sevoflurane with dexmedetomidine (P > 0.05) [Citation18]. The heart rate and mean arterial blood pressure dropped in some patients of the two groups but the comparison was insignificant and Guler et al. [Citation18] reported the same findings, but Kim et al. [Citation20] found that heart rate and mean arterial pressure were significantly lower in dexmedetomidine group than in sevoflurane during surgery (P < 0.05), and the same result was found by Ibacache et al. [Citation22].
Conclusion
Dexmedetomidine decreased significantly the incidence of agitation with sevoflurane in pediatric patients undergoing adenotonsillectomy and associated with a shorter time to extubation, and decreased total dose of sevoflurane, lower incidence of postoperative nausea and vomiting, lower pain score and shorter post-anesthesia care unit length of stay.
Limitations
Our study recognizes some limitations such as being single center study in addition to the small number of patients.
Competing interests and funding
The authors declare that they have no competing interests and all funding was from resources in King Fahad Military Hospital, Khamis Mushayt, Saudi Arabia.
Acknowledgments
This work was not supported by any company and we did not take any fund from any one and we are responsible for that. The authors thank all anesthesia technicians in the operative rooms and all nurses in the post-anesthesia care unit for their efforts and help to achieve this work.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- H.UysalS.TakmazF.YamanThe efficacy of intravenous paracetamol versus tramadol for postoperative analgesia after adenotonsillectomy in childrenJ Clin Anesth2320115357
- T.Voepel-LewisS.MalviyaA.R.TaitA prospective cohort study of emergence agitation in the pediatric postanesthesia care unitAnesth Analg96200316251630
- J.CraveroS.SurgenorK.WhalenEmergence agitation in paediatric patients after sevoflurane anesthesia and no surgery: a comparison with halothanePaediatr Anaesth102000419424
- M.A.OlympioPostanesthetic delirium: historical perspectivesJ Clin Anesth319916063
- I.ConstantR.SeemanInhalational anesthetics in pediatric anesthesiaCurr Opin Anaesthesiol182005277281
- S.M.WalkerR.D.HaugenA.RichardsA comparison of sevoflurane with halothane for pediatric day case surgeryAnaesth Intensive Care251997643649
- B.C.WeldonM.BellT.CraddockThe effect of caudal analgesia on emergence agitation in children after sevoflurane versus halothane anesthesiaAnesth Analg982004321326
- A.BeskowP.WestrinSevoflurane causes more postoperative agitation in children than does halothaneActa Anaesthesiol Scand431999536541
- S.DahmaniI.StanyC.BrasherPharmacological prevention of sevoflurane- and desflurane-related emergence agitation in children: a meta-analysis of published studiesBr J Anaesth1042010216223
- T.Voepel-LewisC.BurkeS.M.HaddenNurses’ diagnoses and treatment decisions regarding care of the agitated childJ Perianesth Nurs202005239248
- J.B.DyckM.MazeC.HaackThe pharmacokinetics and hemodynamic effects of intravenous and intramuscular dexmedetomidine hydrochloride in adult human volunteersAnesthesiology781993813820
- T.OkamotoT.MoriT.TakedaDexmedetomidine is an excellent sedative for voice monitoring surgeryMasui612012542554
- H.PhanM.C.NahataClinical uses of dexmedetomidine in pediatric patientsPaediatr Drugs1020084969
- F.SuG.B.HammerDexmedetomidine: pediatric pharmacology, clinical uses and safetyExpert Opin Drug Saf20115566
- N.SikichJ.LermanDevelopment and psychometric evaluation of the pediatric anesthesia emergence delirium scaleAnesthesiology100200411381145
- R.S.HanallahL.M.BroadmanA.B.BelmanComparison of caudal and ilioinguinal ilio-hypogastricnerve blocks for the control of postorchiopexy pain in pediatric ambulatory surgeryAnesthesiology661987823825
- J.A.AldreteThe post anesthesia recovery score revisitedJ Clin Anesth719958991
- G.GulerA.AkinZ.TosunSingle-dose dexmedetomidine reduces agitation and provides smooth extubation after pediatric adenotonsillectomyPaediatr Anesth152005762766
- J.JiaJ.ChenW.LeEffect of dexmedetomidine on emergency agitation on children after sevoflurane undergoing tonsillectomy and adenoidectomyMed Sci392012293296
- N.Y.KimS.Y.KimH.J.YoonEffect of dexmedetomidine on sevoflurane requirements and emergence agitation in children undergoing ambulatory surgeryYonsei Med J552014209215
- S.QiaoZ.CuiP.MaThe clinical research of dexmedetomidine used in tonsillectomy of children ChineseJ Clinicians6201211951197
- M.IbacacheH.R.MunozV.BrandesSingle-dose dexmedetomidine reduces agitation after sevoflurane anesthesia in childrenAnesth Analg9820046063
- C.Jin-huiY.Yong-qiC.Hui-junEffects of dexmedetomidine on postoperative recovery profile after sevoflurane anesthesia in pediatric patients: a meta-analysisJ Anesth Clin Res42013411
- Q.MengY.Zhong-yuan LuoDexmedetomidine reduces emergence agitation after tonsillectomy in children by sevoflurane anesthesia: a case-control studyInt J Pediatric Otorhinolaryngol76201210361041
- H.Abdel-ghaffarA.Abdel-HaleemEfficacy and safety of intraoperative dexmedetomidine in pediatric post-tonsillectomy pain: peritonsillar versus intravenous administration EgyptianJ Anesthesia272011219225
- J.P.CraveroM.BeachB.ThyrThe effect of small dose fentanyl on the emergence characteristics of pediatric patients after sevoflurane anesthesia without surgeryAnesth Analg972003364367
- I.T.CohenJ.C.FinkelR.S.HannallahThe effect of fentanyl on the emergence characteristics after desflurane or sevoflurane anesthesia in childrenAnesth Analg94200211781181
- A.SamyO.MohamedEffects of fentanyl and dexmedetomidine infusion on tracheal intubation and emergence agitation in children anesthetized with sevofluraneJ Am Sci82012451458