Abstract
Background
During tourniquet induced ischemic reperfusion, reactive oxygen species and cytokines appear and cause cellular damage and remote tissue injury.
Aim
To compare the effects of preoperative intravenous infusion of N-acetyl cysteine or ascorbic acid on the production of malonyldialdehyde as a marker of oxidative stress and IL-6 and IL-8 as markers of systemic inflammation after ischemic reperfusion as primary outcomes. Also both agents were compared regarding post-deflation hemodynamic effects and post-deflation changes in arterial pH and lactic acid as secondary outcomes.
Patient and methods
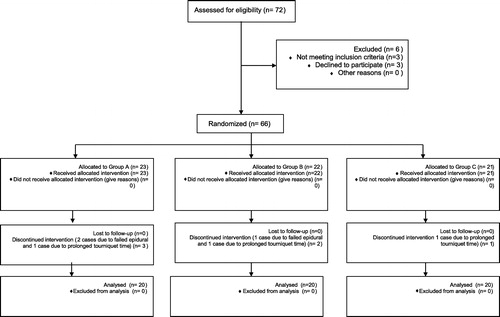
60 patients, scheduled for unilateral lower extremity surgery with a pneumatic tourniquet, were included. The study was designed as a randomized controlled parallel arms superiority trial. Baseline collection of blood samples was done and then patients were randomly classified into three groups: Group A; received 1 g Ascorbic acid, group N; received 10 mg/kg NAC and group C (control group): received 100 ml saline infusion. Epidural anesthesia was administrated. Two blood samples were drawn at each assessment time. One sample for arterial blood pH and lactic acid measurement and the other blood sample was centrifuged and stored at −20 °C for subsequent analysis of MDA, IL-6 and IL-8.
Results
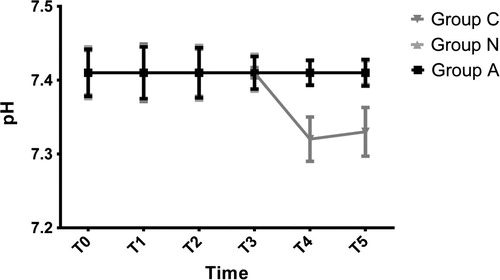
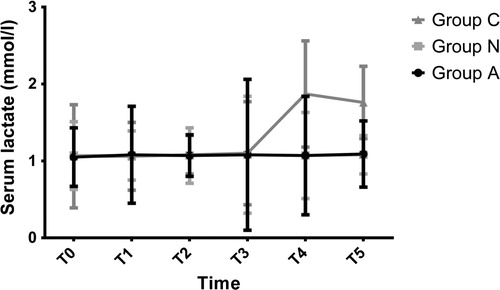
Levels of MDA, IL-6, and IL-8 were significantly increased in group C after tourniquet release compared with the baseline. In groups A and N, MDA did not increase over baseline values, but IL-6 and IL-8 levels were increased and their levels were significantly less than in the control group. Changes in hemodynamics, pH and serum lactate were more evident in group C than groups A and N.
Conclusion
Both N-acetyl cysteine and ascorbic acid reduce post-deflation increase in blood levels of markers of oxidative stress and markers of systemic inflammation and thus both are beneficial in preventing post-tourniquet deflation ischemic reperfusion injury in lower limb surgery.
Introduction
Application of proximal pneumatic tourniquet is widely used in extremity surgeries to control intraoperative bleeding. Ischemia occurs following tourniquet inflation, and reperfusion occurs after deflation because of the re-establishment of blood flow [Citation1]. The hemodynamic and metabolic effects that occur with tourniquet application depend on the duration of tourniquet placement, size of the ischemic area, type of anesthesia, and the cardiovascular condition of the patient [Citation2]. Sequestration of oxygenated blood cells in the extremity during ischemia leads to the appearance of free oxygen radicals [Citation3]. With the event of reperfusion, the Reactive Oxygen Species (ROS) and cytokines appear and cause damage to cellular structures through the process of the lipid peroxidation of cellular membranes and macromolecules [Citation4]. The Cellular damage that occurs after reperfusion of previously viable ischemic tissue is defined as ischemic reperfusion (IR) injury [Citation5]. Antioxidant medications and/or cytokine-modulating therapies might, therefore, reduce morbidity [Citation6]. Lipid peroxidation represents a chain reaction leading to oxidation of polyunsaturated fatty acids, disrupting membrane structure and producing toxic metabolites such as malonyldialdehyde (MDA) which is used as a sensitive marker of ischemic reperfusion injury [Citation7]. Interleukin 6 (IL-6), which is reliable indicator of systemic inflammation, also correlates with the extent of reperfusion injury [Citation8]. IL-6 has been correlated with the activation of circulating neutrophil and potential tissue injury [Citation9]. Circulating IL-8 has also been implicated with the process of lower limb ischemia–reperfusion injury which may cause neutrophil sequestration and increased microvascular permeability especially in the lung [Citation10]. N-acetyl cysteine (NAC), an n-acetyl derivative of the amino acid L-cysteine, is a thiol-containing compound which has been widely used for many years as a mucolytic drug in the treatment of chronic obstructive pulmonary disease. It also has antioxidant, cytoprotective and microcirculatory effects [Citation11]. Its pharmacological actions include restoration of cellular antioxidant potential by restoration of depleted glutathione, direct scavenging of oxygen-free radicals, and inhibition of neutrophil activity and TNF production [Citation12]. Vitamin C, also known as ascorbic acid, is a water-soluble antioxidant molecule that removes the aqueous phase oxygen free radicals by a rapid electron transfer and inhibits oxidative damage to important biological macromolecules, including DNA, proteins, and lipids [Citation13].
In this prospective, double blind, placebo controlled study we compared the effects of preoperative intravenous infusion of N-acetyl cysteine or Ascorbic acid on the production of MDA as a marker of oxidative stress and IL-6 and IL-8 as markers of systemic inflammation after tourniquet induced ischemic reperfusion injury during lower limb surgery as primary outcomes. Also we compared both agents regarding post-deflation hemodynamic effects by comparing total doses of ephedrine consumed and post-deflation changes in arterial pH and lactic acid levels as secondary outcomes.
Patients and methods
After approval of the hospital ethics committee and written informed consent, 60 patients ASA physical status I or II, aged 25–45 years, scheduled for unilateral lower extremity surgery with a pneumatic tourniquet for a duration of 60–90 min, were included in this study. Exclusion criteria included the presence of vascular disease, cardiorespiratory disease, renal insufficiency, liver dysfunction, diabetes or the administration of any antioxidant or anti-inflammatory drug.
No premedication was given. Warm fluids were given to control the mean arterial blood pressure and temperature within normal ranges throughout the study. The study was designed as a randomized controlled parallel arms superiority trial. Baseline collection of blood samples (T0) was done and then sealed, and opaque envelopes containing a computer-generated random sequence were used for randomization of three groups. Randomization type was simple and the randomization code was concealed until the end of the trial and analysis of data.
Group A (Ascorbic acid group): N = 20, received 1 g vitamin C (Ascorbic acid) dissolved in 100 mL 0.9% normal saline intravenously infused within one hour. Group N (N-acetyl cysteine group): N = 20 N received 10 mg/kg NAC dissolved in 100 mL 0.9% normal saline intravenously infused within one hour and Group C (control group): N = 20 received the same volume of saline (100 mL) infused intravenously within one hour as a placebo.
After infusion of the study drugs, epidural anesthesia was administrated at the L2–L3 or L3–L4 interspace using 0.5% bupivacaine. The sensory block level was kept below T10 (in order to minimize the hypotensive effect of epidural anesthesia as possible). The lower extremity was exsanguinated and a pneumatic tourniquet was inflated to a pressure of approximately twice the systolic blood pressure. All operations were performed in the supine position.
Intraoperative arterial blood pressure values of 20% less than basal were considered hypotensive. Intravenous bolus (IV) ephedrine 3 mg was administered as a bolus in the setting of hypotension followed by 1 mg increments to restore baseline blood pressure. When intraoperative bleeding occurred, volume replacement was initiated with saline instead of blood products. The patient demographics, the tourniquet times, volume of local anesthetic and the dosages of ephedrine were recorded. Two blood samples were drawn at each assessment time, at baseline (T0), 1 min after tourniquet placement (T1), 1 min before tourniquet release (T2), 5 min after tourniquet release (T3), 20 min ATR (T4) and 1 h ATR (after tourniquet release) (T5). One sample for Arterial blood pH and serum lactate measurement and the other blood sample were centrifuged to separate the serum and plasma, which were then stored at −20 °C for subsequent analysis of MDA, IL-6 and IL-8.
The plasma MDA was analyzed by the method of thiobarbituric acid reaction (Jiancheng Bio-engineering Research Institute, Nanjing, China); IL-6 and IL-8 were determined using enzyme linked immunosorbent assay with kits (Jingmei Sciences Co., Ltd., Shenzhen, China) according to manufacturer’s instructions.
To maintain the double blind nature of the study, an anesthesia resident who was not present during the patients’ group allocation and tourniquet application collected data and analyzed blood gas. Circulating mediators were analyzed by investigators who were unaware of the patients’ group assignment and the blood gas results.
Statistical methods
Statistical analysis was done using GraphPad© Prism© for Windows© version 6 and GraphPad© Instat© version 3.05 (GraphPad Software, Inc., San Diego California, USA).
It was estimated that a sample of 20 patients per group would have a power of 86% to detect a large effect size of f = 0.45 as regards the primary outcome (production of malonyldialdehyde, IL-6 and IL-8) measures using the F-test and assuming a two-sided type I error of 0.05.
Continuous numerical variables were presented as mean (SD) and intergroup comparisons were done using one-way analysis of variance (ANOVA) with the use of the Tukey–Kramer test for post hoc comparisons. Discrete variables were presented as median (interquartile range) and the Kruskal–Wallis test was used for comparison of the groups. Categorical data were presented as ratio or as number (%) and the Pearson chi square test was used to test between-group differences.
Results
All 60 patients who were included completed the study. As is shown in , there were no differences between the 3 groups as regards the demographic data. The types of surgical procedures were comparable in the 3 groups as well as were the tourniquet time, the upper level of sensory block, and the volume of local anesthetic used.
able 1 Demographic and operative data.
In the control group (C), MDA, IL-6, and IL-8 levels were significantly increased at T3, T4 and T5 after release of the tourniquet compared with the baseline (p-value < 0.0001). In groups (A and N), MDA did not increase over baseline values. IL-6 and IL-8 levels were increased in both groups (A and N) at T3, T4 and T5 after release of the tourniquet, but their levels were significantly less than in the control group ().
able 2 Assays of plasma malonyldialdehyde and serum interleukins levels.
There was no difference between the three groups comparing the total dose of ephedrine used to control the blood pressure before tourniquet release, while there were significant differences between the three groups as regards the total dose of ephedrine used to control blood pressure after tourniquet release (ATR) (p-value < 0.0001) (). In group C there was more consumption of ephedrine than the other two groups.
able 3 Total dose of ephedrine.
and show pH and lactic acid values in the 3 groups at different observation times. There were a decrease in pH and an increase in serum lactate at T4 and T5 only in group (C) when compared with the other 2 groups.
Discussion
The aim of our study was to compare the effects of preoperative intravenous infusion of N-acetyl cysteine or Ascorbic acid on the production of MDA as a marker of oxidative stress and IL-6 and IL-8 as markers of systemic inflammation after tourniquet induced ischemic reperfusion injury during lower limb surgery as primary outcomes. Also we compared both agents regarding post-deflation hemodynamic effects by comparing total doses of ephedrine consumed and post-deflation changes in arterial pH and serum lactate as secondary outcomes.
During tourniquet induced ischemia, cells cannot maintain their membrane integrity, which releases calcium and phospholipid A2 as well as formation of polyunsaturated fatty acids and fatty acid radicals [Citation14]. With reperfusion, fatty acid radicals react with oxygen, triggering lipid peroxidation, which is an autocatalytic mechanism leading to oxidative destruction of cell membranes that increases membrane permeability and stimulates leukocyte chemotaxis with the production of toxic reactive metabolites and cell death [Citation15]. Thus, oxygen derived free radicals and proteolytic enzymes are released from the cells and these materials damage the cells in remote tissues. Consequently, amino acid modifications including 8-hydroxydeoxyguanosine, carbonyls, methionine sulphoxide and MDA are produced. Those oxygen-free radicals or lipid peroxides are short lived and difficult to measure directly. MDA is a more stable degradation product of lipid peroxides, is often assayed, and is believed to reflect the lipid peroxidation level [Citation16]. A significant increase in the level of MDA has been observed in the lung tissue and in plasma of patients undergoing lower limb ischemia–reperfusion [Citation17,Citation18]. IL-6, which is a reliable indicator of systemic inflammation, also correlates with the extent of reperfusion injury and has also been associated with the activation of circulating neutrophil and potential tissue injury [Citation8,Citation9]. Circulating IL-8 has also been implicated in the process of lower limb ischemia–reperfusion injury by a mechanism suggested to involve neutrophil sequestration and increased microvascular permeability in the lung [Citation19,Citation10]. The correlations of the increased levels of MDA, IL-6, and IL-8 with the hemodynamic and blood gas variables in our study support the hypothesis that lipid peroxidation and systemic inflammatory response may play a role in ischemic reperfusion injury after tourniquet induced lower limb ischemia.
The results of our study showed that the use of preoperative N-acetyl cysteine or ascorbic acid decreased the production of MDA, IL-6 and IL-8 during reperfusion after tourniquet induced ischemia, also during the post-inflation period, and there were more stable hemodynamics and no changes in pH or lactic acid levels with the use of these two drugs.
The reduction of the harmful effects of reperfusion injury has been investigated through different approaches including the following: anesthetic techniques [Citation20], preconditioning [Citation21] and drugs as ketamine [Citation22], dexmedetomidine [Citation23] or propofol [Citation24].
NAC is an antioxidant which reacts strongly with the hydroxyl radical and with hypochloric acid, but reacts poorly with the hydrogen peroxide and superoxide radicals. It may also have an indirect antioxidant effect by facilitating glutathione biosynthesis and supplying GSH for glutathione peroxidase catalyzed reactions [Citation25]. A study done by Nagasaki and co-workers showed that in glutathione-depleted liver, NAC prevents hepatic injury and improves liver integrity after I/R injury, as a direct free-radical scavenger not by acting as a substrate for glutathione synthesis [Citation26]. Low-dose N-acetyl cysteine infusion (5 mg/kg/h) was found to attenuate lipid peroxidation and IR injury in arthroscopic knee surgery requiring tourniquet application [Citation27]. In a study conducted by Koca and his co-workers, NAC and ischemic preconditioning were found to have protective effect on the occurrence of oxidative stress resulting from IR period by preventing MDA, super oxide dismutase glutathione peroxidase, total antioxidant capacity, and total oxidant status changes in routine arthroscopic knee surgery [Citation28].
Vitamin C, also known as ascorbic acid, is a potent water soluble natural antioxidant that quenches ROS and inhibits ROS mediated nitric oxide inactivation. In addition, vitamin C can act as coantioxidant by regenerating other antioxidants [Citation29].
Nightingale et al. found that in patients with cardiac failure, nitric oxide (NO) bioavailability increased in the brain stem and blood vessels after intravenous infusion of high-dose vitamin C, leading to improvements in blood vessel distensibility and baroreceptor reflex function. They also reported that this phenomenon directly prevented free oxygen radicals from suppressing the baroreceptors. Oxidative stress regulates NO metabolism in the brain stem and is, therefore, involved in baroreceptor reflex regulation. This might maintain the vascular resistance and baroreceptor reflex and, as a result, mean arterial pressure could also be maintained with the use of high-dose vitamin C [Citation30].
Clinically, the antioxidant effect of vitamin C has been studied in some surgical models. A study done by Dingchao et al., reported that MDA, creatinine phosphokinase (CPK-MB) and lactate dehydrogenase (LDH) levels decreased following the administration of high-dose vitamin C in patients undergoing open heart surgery which may offer some protection for cardiac muscle [Citation31].
In a study conducted by Basili et al., they reported that in patients undergoing elective percutaneous coronary intervention, vitamin C infusion blunted in vivo the increase of 2 markers of oxidative stress, namely (8-OHdG) 8-hydroxy-2′-deoxyguanosine and 8-iso-prostaglandin F2alpha (F2-IPs) with concomitant improvement of thrombolysis in myocardial infarction (myocardial perfusion grade) [Citation32].
Another study showed that vitamin C infusion before percutaneous coronary intervention (PCI) was associated with a lower incidence of PMI (Periprocedural myocardial injury). The investigators suggested that the cardioprotective effect of vitamin C may result from the inhibition of oxidative stress [Citation33].
Administering high-dose vitamin C to elderly patients undergoing bilateral total knee replacement (TKR) surgery could lower MDA levels and prevent the unstable hemodynamics and hypoxia caused by IR injury in both knees, decreasing the incidence of both cardiopulmonary complication and mortality rates [Citation34].
In conclusion, the results of our study showed that both N-acetyl cysteine and vitamin C (ascorbic acid) reduce post-deflation increase in blood levels of markers of oxidative stress and markers of systemic inflammation and thus both are beneficial in preventing post-tourniquet deflation ischemic reperfusion injury in lower limb surgery.
Limitations of the study
There were no limitations of the study.
Conflict of interest
No conflict of interests.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- M.MathruD.J.DriesL.BarnesP.ToninoR.SukhaniM.W.RooneyTourniquet–induced exsanguinations in patients requiring lower limb surgeryAnesthesiology8419961422
- M.GirardisS.MilesiS.DonatoM.RaffaelliA.SpasianoG.AntonuttoThe hemodynamic and metabolic effects of tourniquet application during knee surgeryAnesth Analg912000727731
- A.WakaiJ.H.WangD.C.WinterJ.T.StreetR.G.O’SullivanH.P.RedmondTourniquet–induced systemic inflammatory response in extremity surgeryJ Trauma512001922926
- M.J.ConcannonC.G.KesterC.F.WelshC.L.PuckettPatterns of free-radical production after tourniquet ischemia implications for the hand surgeonPlast Reconstr Surg891992846852
- H.K.EltzschigC.D.CollardVascular ischaemia and reperfusion injuryBr Med Bull7020047186
- R.W.BusuttilG.S.LipshutzJ.W.Kupiec-WeglinskiRPSGL-Ig for improvement of early liver allograft function: a double-blind, placebo-controlled, single-center phase II studyAm J Transplant112011786797
- J.M.MccardThe evolution of free radicals and oxidative stressAm J Med1082000652659
- R.M.RoumenT.HendriksJ.van der Ven-JongekrijgG.A.NieuwenhuijzenR.W.SauerweinJ.W.van der MeerCytokine patterns in patients after major vascular surgery, hemorrhagic shock, and severe blunt trauma: relation with subsequent adult respiratory distress syndrome and multiple organ failureAnn Surg2181993769776
- V.AsensiE.ValleA.MeanaJ.FiererA.CeladaV.AlvarezIn vivo interleukin-6 protects neutrophils from apoptosis in osteomyelitisInfect Immun72200438233828
- D.W.HarkinD.A.BarrosK.McCallionM.HoperM.I.HallidayF.C.CampbellBactericidal/permeability-increasing protein attenuates systemic inflammation and acute lung injury in porcine lower limb ischemia–reperfusion injuryAnn Surg2342001233244
- B.SekhonC.SekhonM.KhanS.J.PatelI.SinghA.K.SinghN-Acetyl cysteine protects against injury in a rat model of focal cerebral ischemiaBrain Res971200318
- Z.SunA.LassonK.OlandersX.DengR.AnderssonGut barrier permeability, reticuloendothelial system function and protease inhibitor levels following intestinal ischemia and reperfusion-effects of pre-treatment with N-acetyl-L-cysteine and indomethacineDigest Liver Dis342002560569
- S.BasiliG.TanzilliE.MangieriIntravenous ascorbic acid infusion improves myocardial perfusion grade during elective percutaneous coronary intervention: relationship with oxidative stress markersJACC Cardiovasc Interv32010221229
- T.YoshiokaK.KawadaT.ShimadaLipid peroxidation in maternal and cord blood and protective mechanism against activated-oxygen toxicity in the bloodAm J Obstet Gynecol13531979372376
- H.AkarA.SaracC.KonuralpComparison of histopathologic effects of carnitine and ascorbic acid on reperfusion injuryEur J Cardiothorac Surg192001500506
- S.Homer-VanniasinkamJ.N.CrinnionM.J.GoughPost-ischaemic organ dysfunction; a reviewEur J Vasc Endovasc Surg141997195203
- Y.J.ChengY.P.WangC.T.ChienC.F.ChenSmall-dose propofol sedation attenuates the formation of reactive oxygen species in tourniquet–induced ischemia–reperfusion injury under spinal anesthesiaAnesth Analg94200216171620
- M.VanC.OlgunerU.KocaA.R.SismanK.MuratliA.KarciO.MaviogluIschaemic preconditioning attenuates haemodynamic response and lipid peroxidation in lower extremity surgery with unilateral pneumatic tourniquet application: a clinical pilot studyAdv Ther252008355366
- P.G.RaijmakersA.B.GroeneveldJ.A.RauwerdaG.J.TeuleC.E.HackAcute lung injury after aortic surgery: the relation between and leg microvascular permeability to 111 indium-labelled transferrin and circulating mediatorsThorax521997866871
- I.BudićD.PavlovićT.CvetkovićN.DjordjevićD.SimićI.MilojevićThe effects of different anesthesia techniques on free radical production after tourniquet–induced ischemia–reperfusion injury at children’s ageVojnosanit Pregl6782010659664
- L.N.LinL.R.WangW.T.WangL.L.JinX.Y.ZhaoL.P.ZhengIschemic preconditioning attenuates pulmonary dysfunction after unilateral thigh tourniquet–induced ischemia–reperfusionAnesth Analg1112010539543
- F.SaricaogluD.DalA.E.SalmanM.N.DoralK.KilinçU.AyparKetamine sedation during spinal anesthesia for arthroscopic knee surgery reduced the ischemia–reperfusion injury markersAnesth Analg1012005904909
- E.BostankoluH.AyogluS.YurtluR.D.OkyayG.ErdoganY.DenizDexmedetomidine did not reduce the effects of tourniquet–induced ischemia–reperfusion injury during general anesthesiaKaohsiung J Med Sci2920137581
- O.AldemirH.CelebiC.CevikE.DuzgunThe effects of propofol or halothane on free radical production after tourniquet induced ischaemia–reperfusion injury during knee arthroplastyActa Anaesthesiol Scand45200112211225
- G.SenerO.TosunA.O.SehirliMelatonin and N-acetyl cysteine have beneficial effects during hepatic ischemia and reperfusionLife Sci7224200327072718
- H.NagasakiH.NakanoK.BoudjemaEfficacy of preconditioning with N-acetylcysteine against reperfusion injury after prolonged cold ischemia in rats liver in which glutathione had been reduced by buthionine sulphoximineEur J Surg16421998139146
- F.SaricaogluD.DalA.E.SalmanO.A.AtayM.N.DoralM.A.SalmanEffect of low-dose N-acetyl-cysteine infusion on tourniquet–induced ischaemia reperfusion injury in arthroscopic knee surgeryActa Anaesthesiol Scand492005847851
- K.1.KocaY.YurttasT.CayciS.BilgicU.KaldirimThe role of preconditioning and N-acetylcysteine on oxidative stress resulting from tourniquet–induced ischemia–reperfusion in arthroscopic knee surgeryJ Trauma7032011717723
- S.J.PadayattyH.SunY.WangVitamin C pharmacokinetics: implications for oral and intravenous useAnn Intern Med1402004533537
- A.K.NightingaleD.J.BlackmanR.FieldRole of nitric oxide and oxidative stress in baroreceptor dysfunction in patients with chronic heart failureClin Sci (Lond)1042003529535
- H.DingchaoQ.ZhiduanH.LiyeThe protective effects of high-dose ascorbic acid on myocardium against reperfusion injury during and after cardiopulmonary bypassThorac Cardiovasc Surg421994276278
- S.BasiliG.TanzilliE.MangieriV.RaparelliS.Di SantoP.PignatelliIntravenous ascorbic acid infusion improves myocardial perfusion grade during elective percutaneous coronary interventionJACC Cardiovasc Interv322010221229
- Z.J.WangW.K.HuY.Y.LiuD.M.ShiW.J.ChengY.H.GuoThe effect of intravenous vitamin c infusion on periprocedural myocardial injury for patients undergoing elective percutaneous coronary interventionCan J Cardiol301201496101
- J.Y.LeeC.J.KimM.Y.ChungEffect of high dose vitamin C on oxygen free radical production and myocardial enzyme after tourniquet ischaemia reperfusion injury during bilateral total knee replacementJ Int Med Res384201015191529