Abstract
Background
Intranasal surgery under general anaesthesia has potential to complicate immediate postoperative recovery period with multitude of respiratory problems. These include from mild respiratory distress to oxygen desaturation to moderate to significant laryngospasm. These problems can be mitigated by employing some innovative manoeuvres by anaesthesiologists to achieve smooth and safe recovery.
Study setting
The study was conducted at PAF Hospital MM Alam after permission from the hospital ethics committee from March 2013 to December 2013.
Level of evidence
The study conforms to level 1b of evidence rating scale.
Study design
This randomised control trial included 120 American Society of Anaesthesiologists physical status I patients aged less than 40 years of both genders, undergoing intranasal surgery under general anaesthesia, who were randomly divided into two groups naming Throat Wash (TW) group or Simple Suction (SS) group. Patients of both groups were induced general anaesthesia as per set protocol while TW group was subjected to throat wash after removal of throat pack while SS group was only suctioned under direct laryngoscopy. Incidence of any adverse respiratory event in immediate post-extubation period was recorded for further comparison.
Results
1.6% patients in TW group developed laryngospasm as compared to 15% patients of SS group (P < 0.0001). 4.8% patients of TW group and 44.9% patients of SS group developed moderate to significant respiratory problems respectively (P < 0.0001). 5% patients in SS group had to re-intubated as compared to none in the TW group (P < 0.00001). Debris recovered during throat wash in TW group included clogs of blood, pieces of bones, cartilage and polyps, rhinolith, and wax from the packing gauze as compared to only some clots of blood in the SS group.
Conclusion
Throat wash, after removal of throat pack in nasal surgery, ensures clearer airway and decreases the risk of adverse respiratory events in immediate post-extubation period. The adverse sequel due to un-recognised debris in the upper airway is minimised resulting in smooth recovery and rapid discharge from the post-anaesthesia care unit.
Introduction
Septal surgery is undertaken to improve airflow through the nasal passages and ventilation of the sinuses. Patients present for surgery owing to near-total nasal airway obstruction due to gross septal deviation, inferior turbinate hypertrophy, or a single or multiple nasal polyps or surgery for cosmetic reasons, etc. [Citation1]. Some nasal procedures can be performed under local anaesthesia with or without sedation, and others usually require general anaesthesia [Citation2–Citation4]. The choice of general or local anaesthetic depends on patient factors, duration and site of surgery, and complexity of the procedure. Generally, local anaesthesia is suitable for minor or more anterior procedures while for more complex or longer procedures, including partial or total inferior turbinectomy, intranasal polypectomy, submucosal resection (SMR) of septum, septoplasty and augmentation septorhinoplasty is general anaesthesia is preferred by many otorhinolarygologists due to the risk of complications [Citation5].
Nearly all nasal surgery has the potential to contaminate the lower airway with blood or secretions and debris such as blood clot/cartilage/bone remnants, rhinolith, paraffin wax and mucous plugs. It is essential that the anaesthesiologist recognises this and takes measures to prevent it. A south-facing or reinforced tracheal tube is often used with a throat pack to reduce blood contamination of the lower airway [Citation6]. Throat pack is an essential part of nasal surgery as it prevents blood and debris from entering into laryngopharynx as well as blood being getting into the stomach which may result in post-operative nausea and vomiting. At the end of surgery, the pack should be carefully removed and noted.
At the conclusion of the surgery, the nasal airway is often blocked with surgical packs which may make it extremely difficult to maintain an airway. Extubation of a tracheal tube is usually undertaken with the patient “awake” or “deep”, each having its own pro and cons so the decision has to be individualised [Citation7]. Many anaesthesiologist must have experienced an increased incidence of coughing, laryngospasm, explained and unexplained oxyhemoglobin desaturation early after extubation and rarely may have seen development of negative pressure pulmonary oedema due to severe laryngospasm in patients undergoing the nasal surgery [Citation8,Citation9]. The patients complicated by these adverse events often require re-intubation, ventilation and sometimes ICU admission prolonging their length of hospital stay considerably increasing the cost.
Measures to achieve safe and smooth recovery from anaesthesia without any adverse sequel include direct laryngoscopy and pharyngoscopy in every patient, and a careful inspection of the oral cavity and postnasal area. There should be flexion of neck to encourage any clot to fall past the soft palate, and direct visualisation of the passage of a suction catheter behind the soft palate. Any clot or debris left behind can be inhaled after removal of a tracheal tube and lead to total airway obstruction and death—hence the term “coroner’s clot” [Citation6].
We have investigated the addition of post-operative throat wash with copious amounts of normal saline after removal of throat pack and before awakening the patient from general anaesthesia under direct laryngoscopy.
Objective
The objective of this study was to compare post-operative recovery with or without pre-extubation throat wash in patients undergoing intranasal surgery under general anaesthesia.
Study setting
The study was done at Pakistan Air Force Hospital MM Alam from March 2013 to December 2013 in Operation Theatre department in collaboration with ENT department.
Materials and methods
This parallel type randomised control study was conducted after taking written permission from hospital ethics committee subsequent to a thorough presentation on study proposal. Their concern about the patient confidentiality was adequately addressed. One hundred and twenty American Society of Anaesthesiologists (ASA) physical status I patients of both sexes, aged 40 years or less, undergoing Sub-mucosal Resection (SMR) of septum/septorhinoplasty/rhinoplasty were included in the study. Any patients with significant respiratory or cardiac disease, moderate to severe OSA, history of airway reactivity or any other comorbidity were excluded from the study. The patients were randomly selected (using random number generator) to receive throat wash [Throat Wash Group (TW group)] or simple suction [Simple Suction group (SS group)].
All the patients were admitted to the hospital one day before the scheduled surgery. Routine clinical chemistry tests and hepatitis B and C screening were performed as per the hospital protocol. Written informed consent was obtained from all patients. In the operation theatre an intravenous 22 gauge (I.V) cannula was inserted to each patient for I.V infusion (Lactated Ringers solution) and administration of drugs. Before induction of anaesthesia, all the patients were explained that an intranasal packing will be inserted after the surgery and they should try to breathe from mouth after they wake up from anaesthesia. Peri-operative monitoring was applied which included continuous 5 lead ECG, non-invasive arterial pressure at 3 minutes interval, SpaO2, end-tidal carbon dioxide (ETCO2) and end-tidal anaesthetic agent (ETAA).
After determination of baseline monitoring parameters and premedication with glycopyrolate 0.1–0.2 mg, metoclopramide 10 mg and tramadol 70–80 mg, standard induction with propofol (1.5–2.5 mg/kg) and atracurium (0.4–0.5 mg/kg) was done. An appropriate sized oral RAE or reinforced ETT was used to intubate and fixed in midline to facilitate the surgical access. Throat was packed to safeguard the oro- and laryngo-pharynx from contamination of blood and surgical debris. The patient was maintained on close circuit anaesthesia using Datex Ohmeda’s Avance® Carestation® on isoflurane and 30% Air oxygen mixture. Injection Paracetamol 1 g IV was given during the surgery for postoperative analgesia. Injection Ondansatron 4 mg and injection Dexamethasone 8 mg were given towards the end of the surgery to prevent post-op nausea and vomiting.
The TW group patients (n = 62) were selected to receive throat wash with normal saline. After surgery was finished all patients were suctioned under vision with the help of laryngoscopy. Throat pack was taken out and 30–40 ml of lukewarm normal saline was poured into oropharynx through a 50 ml big nozzle syringe and suctioned out with the help of suction catheter under vision. The procedure was repeated three times by which time the throat would be cleared off almost all the blood and surgical debris such as blood clots/pieces of bone or cartilage/wax from the packs/rhinolith.
The SS group (n = 60) patients got simple suction under vision only. Throat pack was taken out and suction was done to clear throat of any visible debris/blood with the help of direct laryngoscope.
After the suctioning/throat wash, anaesthetic agent was turned off and patients were allowed to reverse from general anaesthesia. All the patients were reversed using neostigmine (2.5 mg) and glycopyrolate (0.5 mg) and extubated only when they were able to spontaneously open their eyes or respond to verbal commands.
In the immediate post-op recovery period patients of both the groups were observed for any major or minor complications such as moderate to severe laryngospasm, difficulty in breathing, unexplained desaturations or emergence delirium. The frequency of these adverse events was recorded in each group to be compared with each other.
Statistical analysis
All the data collected by were entered into IBM ®Statistical package for Social sciences (SPSS) version 21.0; and were analysed using SPSS. The descriptive statistics were used to calculate mean, standard deviation and averages, etc. Cross tabs and chi square test were used to compare means and calculate p value. P value < 0.05 was considered significant.
Results
Demographically both the groups were quite similar showing no considerable difference between them. TW group patients were aged 23.45 ± 3.46 years as compared to 24.65 ± 4.27 years in SS group. Male to female ratio in TW group was 4.82:1 while it was 5:1 in SS group.
In patients of TW group, only one patient (1.6%) developed laryngospasm while in SS group 15 patients (25%) experienced mild to moderate laryngospasm. Chi squared equals 14.636 with 1 degrees of freedom. The two-tailed P value equals 0.0001 which signifies it to be statistically significant ().
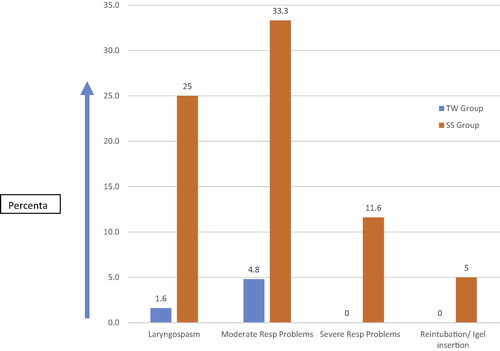
In TW group, only 3 (4.8%) patients had moderate post-op respiratory problem such as difficulty in breathing, post-op desaturation and delirium while in SS group 20 (33.3%) patients had moderate problems and 7 (11.6%) patients had significant respiratory problems. In total (33.3% + 11.6%) 44.9% patients in SS group showed moderate or significant respiratory problem in immediate post recovery period (). Chi squared equals 26.522 with 1 degrees of freedom. The two-tailed P value is less than 0.0001. The association between rows (groups) and columns (outcomes) is considered to be extremely statistically significant.
Three (5%) patients in SS group required a re-intubation/LMA insertion to maintain airway after muscle relaxation.
The debris which was recovered during the throat wash included clotted blood, pieces of cartilage, bone and polyp, rhinolith, wax from the paraffin gauzes used for the nasal packs and soft tissue like part of polyp. shows the frequency and percentage difference between the two groups. In SS group despite doing proper laryngoscopy and pharyngoscopy nothing more than clotted blood could be suctioned out.
able 1 Table signifies the efficacy of throat wash in removing surgical debris in patients undergoing intranasal surgery under general anaesthesia. Throat wash was significantly superior in removing all types of debris as compared to Simple suction.
Discussion
An experienced anaesthesiologist always takes nasal surgery very seriously because of its inherent risks of compromised airway due to the intra-nasal packing and decreased accessibility to full airway after surgery. Most of the anaesthesiologist face a Catch-22 situation as how to proceed for the safe and smooth reversal and recovery in patients undergoing nasal surgery under general anaesthesia. Some prefer deep extubation while others opt for a full awake recovery. Many must have experienced themselves managing adverse airway issues such as moderate to severe laryngospasm or inadvertent desaturation after nasal surgery, making it a horrendous experience for them. Sometimes they have to manage a patient developing post-operative delirium and confusional state or emergence agitation which is usually associated with tightly packed nose or multitude of respiratory problems. Few cases have been reported who developed negative pressure pulmonary oedema due to the severe laryngospasm requiring post-operative mechanical ventilation and ICU admission [Citation10].
Contrary to the common thinking, despite the throat pack there is still risk of airway contamination as the tracheal cuff is below the glottic and subglottic airway, and blood can still pass down from the nasopharynx, past a throat pack, along the outer surface of the tracheal tube to the level of the vocal cords and subglottis. This can also result in increased incidence of laryngospasm or difficult recovery period.
Studies have shown that nasal packing is a cause for significant morbidity and discomfort in the immediate post-operative period [Citation11]. Awan et al., have investigated and observed that the routine use of nasal packing after septoplasty is controversial among many rhinologists [Citation12]. Still many otorhinolaryngologist have been trained to place nasal packing after intranasal surgery, so they consider it a norm. The presence of this packing makes the immediate post-operative recovery period delicate. The patients who underwent septoplasty with bilateral totally occlusive nasal packing had an increased risk of experiencing respiratory distress [Citation13]. The return of normal breathing effort followed by consciousness and a tightly packed nose makes the patient put in extra effort to breathe forcefully. The presence of any debris may result in laryngospasm, sudden respiratory distress or unexplained desaturation warranting advanced airway manoeuvring.
Severe laryngospasm is a very serious complication which can lead to negative pressure pulmonary Oedema [Citation14]. This is potentially life threatening and can result in re-intubation, mechanical ventilation, admission to an intensive care unit (ICU), and a prolonged length of hospital stay [Citation15,Citation10]. There is a requirement of prompt detection, diagnosis, and treatment of this syndrome. One of the patients in SS group developed this complication but was adequately managed and discharged next day from the ICU.
The rationale behind the introduction of throat wash was based on the premise the most careful suctioning and laryngoscopy were still imperfect in removing all the debris which may hamper the smooth recovery. While employing throat wash, we observed that the debris such as clogs of clotted blood, pieces of bone and cartilage, rhinolith and wax from the paraffin gauzes (which were used to pack the nose) were frequently removed. Comparison of both the groups under study as shown in highlights that throat wash was far superior in ensuring the removal of all the hard debris as compared to simple suction. This resulted in a far clearer airway, confident anaesthetist, smooth recovery, safe patient and satisfied surgeon.
Many centres around the world now advocate the use of flexible laryngeal mask airway (LMA) for nasal surgery under general anaesthesia to reduce these types of complications [Citation7,Citation16,Citation17]. This is an advanced use of the LMA and hence only be practised in experienced hands [Citation17]. We now have developed our own institutional protocol for use of LMA in nasal surgery and have achieved some promising results. But still many of our colleagues prefer to use traditional endotracheal tube for nasal surgery.
Considering the effectiveness of this simple manoeuvre in preventing potentially life threatening complications, a comprehensive research of the medical literature on PubMed and other indexing service surprisingly yielded no similar studies or interventions. The lack of evidence suggests that either the problem is not adequately understood or the anaesthesiologists have been reluctant to share their experiences. Further research in other settings is warranted to develop and propose a practice guideline or expert review which may further elaborate the benefits or otherwise of this intervention in the patients undergoing intranasal surgery under general anaesthesia.
Conclusion
Intranasal surgery under general anaesthesia has inherent risk of complications in the postoperative recovery period due to the occlusive nasal packing, pooling of surgical debris in oro-pharynx and restricted airway access. Achieving uneventful and smooth recovery is a goal of any conscientious anaesthesiologist. Direct laryngoscopic suctioning has been employed since long to clear the airway from the surgical debris. We have found that throat wash with lukewarm normal saline is extremely effective in removing occult surgical debris such as clotted blood, pieces of polyps, cartilage and bone, rhinolith, and wax from packing gauzes. It ensures clearer airway, confident anaesthetist, smooth recovery, safe patient and satisfied surgeon.
Competing of interest
We declare that we have no financial or other competing interests attached with this research.
Conflict of interest
Nill.
Financial disclosure
Nil.
Notes
Institution where Study was carried out: Pakistan Air Force Hospital, MM Alam, Pakistan.
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- B.O.O’DonoghueEar nose and throat surgeryM.MorganG.M.HallShort practice of anaesthesia1998Chapman & HallLondon317335
- V.SrinivasanR.B.ArasarathamG.A.JankelowitzDay-case septal surgery under general anaesthesia and local anaesthesia with sedationJ Laryngol Otol1091995614617 [PubMed]
- J.A.CookR.D.McRaeR.M.IrvingL.N.DowieA randomized comparison of manipulation of the fractured nose under local and general anaesthesiaClin Otolaryngol151990343346 [PubMed]
- J.WaldronD.B.MitchellG.FordReduction of fractured nasal bones versus general anaesthesiaClin Otolaryngol141989357359 [PubMed]
- A.J.ManigliaFatal and major complications secondary to nasal and sinus surgeryLaryngoscope991989276283 [PubMed]
- M.A.FeldmanA.PatelAnaesthesia for eye, ear, nose and throat surgeryR.D.MillerMiller’s anaesthesia2005Churchill Livingstone ElsevierUSA2368
- A.C.WebsterP.K.Morley-ForsterV.JanzenAnesthesia for intranasal surgery: a comparison between tracheal intubation and the flexible reinforced laryngeal mask airwayAnesth Analg881999421425 [PubMed]
- V.M.MehtaG.Har-ElN.A.GoldsteinPostobstructive pulmonary edema after laryngospasm in the otolaryngology patientLaryngoscope116200616931696 [PubMed]
- LourdesAl GhofailyCourtneySimmonsLindaChenRenyuLiuNegative pressure pulmonary edema after laryngospasm: a revisit with a case reportJ Anesth Clin Res32013252 [PubMed] [Free PMC Full Text]
- J.R.HolmesR.N.HensingerE.W.WojtysPostoperative pulmonary edema in young, athletic adultsAm J Sports Med191991365371 [PubMed]
- S.M.BanglawalaM.GillD.D.SommerA.PsaltisR.SchlosserM.GuptaIs nasal packing necessary after septoplasty? A meta-analysisInt Forum Allergy Rhinol32013418424 [PubMed]
- M.S.AwanM.IqbalNasal packing after septoplasty: a randomized comparison of packing versus no packing in 88 patientsEar Nose Throat J872008624627 [PubMed]
- M.CayonuA.AcarE.HorasanlıA.AltundagM.SalihogluComparison of totally occlusive nasal pack, internal nasal splint, and transseptal suture technique after septoplasty in terms of immediate respiratory distress related to anesthesia and surgical complicationsActa Otolaryngol1342014390394 [PubMed]
- J.J.BaltimorePostlaryngospasm pulmonary edema in adultsAORN J701999468476 479; quiz 480-4 [PubMed]
- T.VisvanathanM.T.KlugerR.K.WebbR.N.WesthorpeCrisis management during anaesthesia: laryngospasmQual Saf Health Care142005e3 [PubMed] [Free PMC Full Text]
- A.KaplanG.J.CrosbyN.BhattacharyyaAirway protection and the laryngeal mask airway in sinus and nasal surgeryLaryngoscope1142004652655 [PubMed]
- P.J.WilliamsC.ThompsettP.M.BaileyComparison of the reinforced laryngeal mask airway and tracheal intubation for nasal surgeryAnaesthesia501995987989 [PubMed]
