Abstract
Neurofibromatosis is an autosomal dominant disease characterized by widespread effects on different systems of the body. A 65 year old male who had to undergo surgery on the left thigh had neurofibromatosis type 1 with extensive neurofibromas all over his body, including the entire back. Patient was given spinal anaesthesia, at L3–L4 intervertebral space. Successful subarachnoid block was obtained and the surgery was performed successfully without any untoward complications.
Introduction
Neurofibromatosis is a group of hereditary diseases transmitted in autosomal dominant manner. It has extensive effects on ectodermal and mesodermal tissue and is the most common type of neurocutaneous syndromes. On clinical and genetic grounds, neurofibromatosis has been classified into two different types – neurofibromatosis type 1 (NF1) and neurofibromatosis type 2 (NF2). Von Recklinghausen disease, also known as neurofibromatosis 1 (NF1), is characterized by multiple cafe-au-lait spots in the skin, multiple peripheral nerve tumors, and a variety of other dysplastic abnormalities of the skin, nervous system, bones, endocrine organs, and blood vessels [Citation1]. The birth incidence of NF1 lies between 1 in 2500 and 1 in 3300 and its prevalence in the population is 1 in 5000 [Citation2]. NF2 is defined by the presence of bilateral vestibular schwannomas. The birth incidence of NF2 lies between 1 in 33,000 and 1 in 40,000 with a prevalence within the population of 1 in 210,000 [Citation3]. Both NF1 and NF2 can present as a non-generalized form in which only one body part is affected.
All this requires astute decisions on part of the anaesthesiologist confronted with such a case posted for surgery, as unique obstacles must be overcome for success.
Case report
A 65 year old male with body weight 58 kg and height 166 cm presented with a fungating ulcer for the past two months gradually increasing in size, which developed from one nodule present on the anterior aspect of his left thigh.
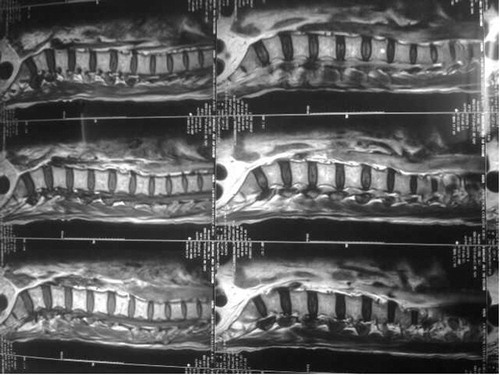
In the preoperative laboratory assessment all the investigations were within normal range. A pulmonary Function Test was done which was within normal range. A cranial and spinal MRI was advised to rule out central nervous system involvement, which showed no abnormality ().
On physical examination, the patient’s entire body was covered with nodules of different sizes (). Oral examination revealed lesions on the tongue. To rule out deeper involvement of the airways, indirect laryngoscopic examination was done, the results of which were normal. The rest of the physical examination was normal. There was no associated deformity of the spine. There was no history of any other associated comorbidity. The patient consented for regional anaesthesia only, so it was decided to conduct the case under spinal anaesthesia. A written informed consent was obtained. On arrival in the operating room, an 18-gauge intravenous line was secured and all the standard monitors were attached. 500 ml lactated ringer’s solution was administered, and the patient was placed in sitting position for subarachnoid block. After preparing the site, spinal anaesthesia was successfully performed between L3 and L4 intervertebral space, with a 26-gauge needle and 3 ml of 0.5% hyperbaric bupivacaine (). The patient was immediately placed in supine position and oxygen was supplemented via Hudson’s mask at a flow rate of 6 l/min. After 5 min, the level of anaesthesia was checked and the surgery was started after 10 min. 1.5 mg of midazolam IV was administered to sedate the patient.
The surgery lasted for 1 h. All hemodynamic parameters were stable during the operation. The urinary output was 150 ml. The patient was then shifted to the postoperative recovery room where he was observed for 3 h and subsequently shifted to the surgical ward, with no postoperative complications reported. He was discharged on the 5th postoperative day.
Discussion
Neurofibromatosis is an autosomal dominant disease that has widespread effects on ectodermal and mesodermal tissue. Neurofibromatosis-1 (NF1) is the commonest member of the group which may affect different systems with varying severity. Neurofibromin, encoded by the gene NF-1 located on chromosome 17, is involved in tumour suppression. Inactivation of the NF-1 gene results in the production of a shortened version of this tumour suppression protein, which leads to loss of function and subsequent development of many different types of tumours seen with the disease. Although neurofibromas are the characteristic lesions of the disease, they may have widespread effects on the airway, respiratory system, cardiovascular system, central nervous system, gastrointestinal and genitourinary system.
Intra-oral manifestations may be seen in approximately 5% of patients [Citation4]. Distinct lesions may affect the tongue [Citation5,Citation6] and larynx [Citation7,Citation8], and may also be found in the cervical region and parapharyngeal space. These may cause obstruction and distortion of the airway, both prior to or after induction of anaesthesia. The difficulty with laryngoscopy and intubation encountered may require emergency tracheostomy. So, preoperative evaluation should involve imaging with indirect laryngoscopy or CT or MRI. In addition, the presence of macroglossia, macrocephaly, specific mandibular abnormalities [Citation9] and cervical spine involvement may contribute to difficulties of airway management.
Neurofibromas originating from the mediastinum or those spreading from the retroperitoneum may cause tracheal or bronchial compression [Citation10]. Though rare, intrapulmonary neurofibromas may be associated with cough and dyspnoea. Pulmonary fibrosis may be associated in up to 10–20% of cases with NF-1 [Citation11]. The pulmonary fibrosis is usually of adult onset and progressive, [Citation12,Citation13] and may culminate in pulmonary hypertension and right ventricular failure [Citation14]. Spinal deformities such as kyphosis and scoliosis with rotation can occur resulting in reduction in lung volume or even respiratory failure in severe cases. Hence a detailed evaluation of respiratory system preoperatively is essential and should include a chest X-ray, a CT scan of the thorax and detailed lung function testing.
Hypertension occurs in approximately 6% of NF-1 patients and in 30% of these cases, it is secondary to renovascular disease, coarctation of aorta or phaeochromocytoma [Citation15]. In hypertension present in young NF-1 patients, it is usually because of renal artery stenosis [Citation16]. Phaeochromocytoma affects between 0.1% and 5.7% of patients with NF1 but almost 25% of patients with phaeochromocytoma have the disease [Citation17]. Vascular neurofibromatosis is seen in some cases and it may be a cause of aortic and cerebral aneurysms [Citation18]. Superior Vena Obstruction may occur due to large mediastinal tumours [Citation10]. Clearly, a detailed clinical history coupled with relevant investigations is must in preoperative assessment of the cardiovascular system. Regular arterial blood pressure monitoring should be mandatory in all NF-1 patients and any anti-hypertensives that are nephrotoxic must be prescribed with caution. Urinary catecholamine estimation and abdominal CT scan should be performed if there is any suspicion of Phaeochromocytoma.
A large part of the morbidity and mortality of NF-1 is accounted for by tumours of the central nervous system. Anaesthetic assessment should include history of seizures, headaches, compressive symptoms and others that may suggest undiagnosed CNS tumours. An MRI and CT scan of the head and spine should be made mandatory.
The choice between general and regional anaesthesia in patients with neurofibroma thus requires careful consideration. Traditionally, general anaesthesia has been the usual approach as coexisting cranial or spinal neuromas might worsen neurological outcome in patients who have been administered for regional anaesthesia. However, associated airway abnormalities, cardiovascular, central nervous system and other anomalies make general anaesthesia more risky.
Management of the patients with neurofibroma at the back poses a challenge to the anaesthesiologist. Decision between regional and general anaesthesia should also be meticulously weighed. The identification of the spinous process at the back is quite difficult but not impossible by an experienced anaesthesiologist.
Conflict of interest
The authors declare that there are no conflict of interests.
Contribution
Qazi Ehsan Ali performed the procedure and proofreading.
Zaid Saghir Ahmed assisted the procedure.
Syed Hussain Amir electronic preparation and proofreading.
Sajad Hussain Najar helped in reference collection.
Abdullah Zoheb Azhar patient assessment.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- D.HirataH.NaraT.InabaVon Recklinghausen disease in a patient with X-linked agammaglobulinemiaIntern Med41200210391043
- F.W.CroweW.J.SchullJ.V.NeelA clinical, pathological, and genetic study of multiple neurofibromatosis1956Charles C. ThomasSpringfield (IL)
- S.M.HusonWhat level of care for the neurofibromatoses?Lancet353199911141116
- E.BadenH.E.PierceW.F.JacksonMultiple neurofibromatosis with oral lesions; review of the literature and report of a caseOral Surg81955263280
- S.C.SharmaS.SrinivasanIsolated plexiform neurofibroma of tongue and oropharynx: a rare manifestation of von Recklinghausen’s diseaseJ. Otolaryngol.2719988184
- R.W.SmithA treatise on the pathology, diagnosis and treatment of neurofibroma1849Hodges and SmithDublin
- M.Chang-LoLaryngeal involvement in von Recklinghausen’s disease: a case report and review of the literatureLaryngoscope871977435442
- M.McD.FisherAnaesthetic difficulties in neurofibromatosisAnaesthesia301975648650
- L.LeeY.-H.YanM.J.PharoahRadiographic features of the mandible in neurofibromatosisOral Surg Oral Med Oral Path Radiol Endod811996361367
- R.E.OakleyG.J.GrotteProgressive tracheal and superior vena caval compression caused by benign neurofibromatosisThorax491994380381
- S.A.DavisR.L.KaplanNeurofibromatosis and interstitial lung diseaseArch Dermatol114197813681369
- J.L.BurkhalterJ.U.MoranoM.B.McCayDiffuse interstitial lung disease in neurofibromatosisSouth Med J791986944946
- S.S.SagelJ.V.ForrestF.B.AskinInterstitial lung disease in neurofibromatosisSouth Med J681975647649
- B.H.R.StackJ.StJ.ThomasPulmonary infiltrationsR.A.L.BrewisG.J.GibsonD.M.GeddesRespiratory medicine1990Balliere TindallLondon1188
- S.M.HusonRecent developments in the diagnosis and management of neurofibromatosisArch Dis Child641989745749
- E.BourkeP.B.B.GatenbyRenal artery dysplasia with hypertension in neurofibromatosisBr Med J21971681682
- M.W.McClellanJ.HerringE.EnquistH.R.KeiserW.M.LinehanVon Recklinghausen’s disease and phaeochromocytomasJ Urol162199915821586
- L.J.RubinsteinThe malformative central nervous system lesions in central and peripheral forms of neurofibromatosis. A neuropathological study of 22 casesNY Acad Sci48619861429