Abstract
Objective
To compare the effectiveness of small dose of propofol or midazolam in treating laryngospasm following extubation in adult patients undergoing oropharyngeal operations.
Methods
The study was conducted in Al-Zahra Hospital, Al-Azhar University, Egypt. One hundred and twenty adult patients, with age range 30–50 years, ASA physical status I–II, of either sex undergoing elective oropharyngeal surgeries under general anesthesia were randomly allocated to one of three equal groups (n = 40) using a computer generated randomization table. At extubation before suction, the patients in the three groups were administered intravenously propofol 0.8 mg/kg diluted in 20 ml (Group P) or midazolam 0.05 mg/kg diluted in 20 ml (Group M) or saline 20 ml as control group (Group C). The following parameters were recorded: hemodynamic changes (heart rate and mean arterial blood pressure), the frequency and severity of laryngospasm and cough were recorded before time of extubation and up to 5 min using four point scale.
Results
Compared with the control group, there was a significant decrease in the mean arterial pressure and increase in pulse rate in both groups after administration of the study drugs and up to 5 min after extubation, and this change was comparable and similar in both groups. During emergence and up to 5 min, the incidence and severity of postoperative laryngospasm and cough were significantly lower (p < 0.05) in both propofol and midazolam groups as compared to control group. The change in both propofol and midazolam groups was insignificant and comparable.
Conclusion
We conclude that intravenous administration of small dose of propofol or midazolam before tracheal extubation decreases the incidence and severity of laryngospasm and coughing in adult patients undergoing oropharyngeal surgeries.
Introduction
Laryngospasm and airway complications such as coughing and oxygen desaturation are serious complications after tracheal extubation [Citation1]. Laryngospasm is considered a physiological exaggeration of the glottis closure reflex. This complication is more frequent in the following:
| . | Children. able 3 Incidence of severity of postoperative laryngospasm (data present as number percentage). | ||||
| i. | Patients with airway infection. | ||||
| ii. | Those undergoing manipulation of the airway. | ||||
| v. | Those using specific anesthetics. | ||||
| . | Those undergoing oral or pharyngeal surgeries, and | ||||
| i. | Smokers [Citation2]. | ||||
Extubation complications such as bucking, breath holding, laryngospasm and pulmonary edema continue to be major problems for the anesthesiologist, especially in oral surgery, because at the end of surgery the mouth is full of secretions and mixed blood and there is edema of the tissues. Deep anesthesia will delay recovery while light plane may result in coughing, breath holding efforts of self removal of tube, laryngospasm, pulmonary edema [Citation3], hypoxia and cardiac arrest [Citation4]. There has been considerable research conducted on methods and drugs to prevent coughing during emergence such as extubation at a great anesthetic depth, the use of succinylcholine [Citation5], topical lignocaine [Citation6], aerosolized lignocaine [Citation7], nitroglycerine [Citation8], small dose of propofol [Citation9], and magnesium [Citation10]. These methods all come with advantages and disadvantages.
Propofol is used widely in clinical anesthesia, and it is known to be an inhibitor of airway reflexes [Citation11]. It has been reported that single i.v. administration of a subhypnotic dose of propofol effectively prevents laryngospasm and coughing during emergence in children [Citation12,Citation13].
As laryngospasm is considered a life-threatening condition, it may increase the level of anxiety and in turn cause panic in most individuals; panic in turn triggers an episode of asthma, making this a vicious cycle, which can be broken by midazolam.
Therefore, we have performed this study in order to analyze the effects of small dose of propofol or midazolam on preventing laryngospasm and cough during the emergence from anesthesia following oropharyngeal surgeries.
Patients and methods
We designed a prospective, randomized, and controlled study using a computer–generated randomization table to evaluate the efficacy of small dose propofol or midazolam to prevent laryngospasm and coughing following oropharyngeal surgeries.
After approval from the local ethical committee, an informed written consent was obtained from 120 patients of American Society of Anesthesiologists (ASA) grade I & II, age range between 30 and 50 years, of either sex scheduled for elective oropharyngeal surgery (Uvulopalatopharyngoplasty (UPPP), Laryngoscopy with vocal cord surgery, Dental surgery, and Arytenoidectomy) under general anesthesia in Al-Zahra Hospitals, Al-Azhar University.
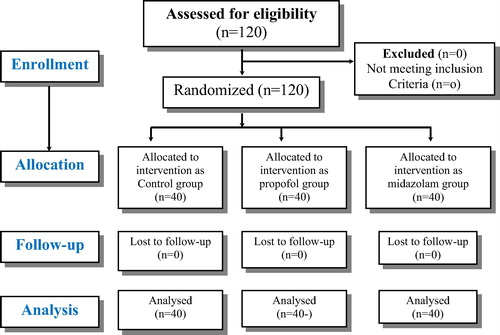
The duration of study was one year only from 2013 to 2014 and to get the unbiased results, the demographic matching was necessary. Hence, a sample size of 120 patients to get the preliminary trends was found to be feasible as shown in
Patients who received drugs such as lidocaine or a supplemental dose of narcotics before extubation were excluded from the study; patients of ASA grade III/IV, those above 60 years or below 12 years, and those with a full stomach were also excluded. Patients with a history of bronchial asthma, allergy especially chest, cardiovascular, or upper respiratory tract diseases, smokers and obese patients with BMI greater than 35 kg/m2 were not enrolled in the study.
Patients were included in this study after a review of their preoperative history, clinical examination and full investigation recorded in their hospital charts. Sedative premedication drugs were not given to the patients. After arrival to the operation room, the patients were randomly divided into three equal groups (40 patients each) by using computer generated randomization table.
| #x2022; | Control group (c): saline 20 ml was given at the time of extubation before suction. | ||||
| #x2022; | Propofol group (P): Propofol 0.8 mg/kg diluted in 20 ml given intravenously at extubation before suction. | ||||
| #x2022; | Midazolam group (M): Midazolam 0.05 mg/kg diluted in 20 ml given intravenously at extubation before suction. | ||||
Upon arrival in the operating room, intravenous cannula was inserted and electrocardiogram, non-invasive blood pressure, pulse oximeter, and end tidal CO2 were applied to all patients and their baseline vital signs were measured.
All patients were administered standard general anesthesia consisting of thiopental (4 mg/kg), fentanyl (1–2 μg/kg), and cisatracurium (0.15 mg/kg), administrated intravenously to facilitate tracheal intubation using the appropriate size of cuffed endotracheal tube. Anesthesia was maintained using 1–1.5% isoflurane in a mixture of oxygen and air at a ratio of 50:50. Ventilation was controlled mechanically and adjusted to maintain normocapnia (end tidal CO2 30–35 mmHg). The vital data of the patients (noninvasive arterial blood pressure, heart rate, oxygen saturation and end tidal carbon dioxide) were monitored continuously throughout the surgery. Adequate muscle relaxation during the operation was maintained by 0.05 mg/kg of cisatracurium every 30 min. Increments in dose of fentanyl 1 μg/kg were administered when there were signs of inadequate anesthesia (e.g. increases in arterial pressure greater than the target mean arterial pressure (MAP) or tachycardia more than 90 beat/min). Patients received their maintenance fluids (intravenous crystalloids) intraoperatively. At the end of surgery, residual neuromuscular blockade was antagonized using 0.05 mg/kg neostigmine and 0.01 mg/kg atropine.
A trained assistant anesthetist, not part of the study, prepared identical syringe with the study medication drugs. Three minutes before suction and extubation, an anesthesiologist injected the previously prepared study drugs for 10 s (propofol 0.8 mg/kg diluted in 20 ml normal saline for propofol group, midazolam 0.05 mg/kg diluted in 20 ml normal saline for midazolam group and 20 ml normal saline as control group).
Extubation of the endotracheal tube was performed when the patient followed oral commands of “Open your eyes” and showed regular spontaneous respiration, or when the patient attempted self-extubation.
If laryngospasm occurs, removal of the irritant stimulus, jaw thrust and administration of 100% oxygen are the first steps in management. Oxygen therapy should be started with a ‘T’ piece so that continuous positive airway pressure (CPAP) might be initiated which often breaks the spasm. In the case of prolongation of laryngeal spasm for more than 2 min after treatment or a drop of saturation to less than 70%, intubation is performed by administering 1 mg/kg succinylcholine and ventilating with 100% O2.
The following parameter were recorded by anaesthesia nurse blind to the patients’ group: (1) the incidence and severity of postextubation coughing and laryngospasm using four point scale. (2) The mean arterial pressure (MAP) and heart rate (HR) were recorded before suction, after suction and up to 5 min after extubation.
.1 Statistical analysis
The sample size was determined by referring previous studies which reported that the incidence of coughing after general anesthesia was 76% [Citation14]. When it was hypothesized that using propofol would reduce the occurrence of coughing to 50%, 25 patients are needed per group for a power analysis of 0.8 (α = 0.05, β = 0.2). Here, in anticipation of dropout, 40 patients per group, 120 patients in total, were determined. Statistical package for social science (SPSS) program version 17 (SPSS Inc, Chicago, Illinois, USA). The data were presented as mean ± SD, when quantitative, or numbers and percentages when qualitative. The following tests were done: A one-way analysis of variance (ANOVA) was used when comparing between more than two means and Chi-square (x2) test of significance was used in order to compare proportions between two qualitative parameters to analyze the incidence of baseline and up to 5 min postoperative adverse events. Probability (P-value) P-value <0.05 was considered significant, P-value <0.001 was considered as highly significant, and P-value >0.05 was considered insignificant.
Result
One hundred and twenty patients were enrolled in the study. They were divided randomly into 3 equal groups (40 in each group), Group C (control group), Group P (propofol group), and Group M (midazolam group).
There were no significant differences between all groups with regard to demographic data or ASA status, and types and duration of surgeries, as shown in ().
able 1 Patient characteristics and operation time (data represent as mean (SD) or number).
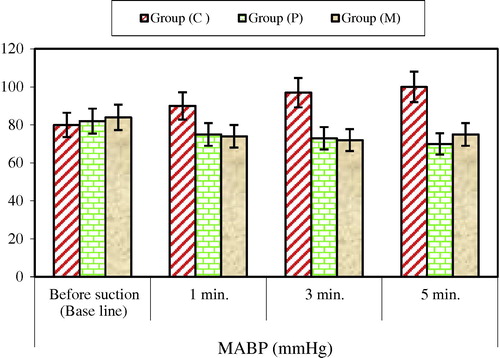
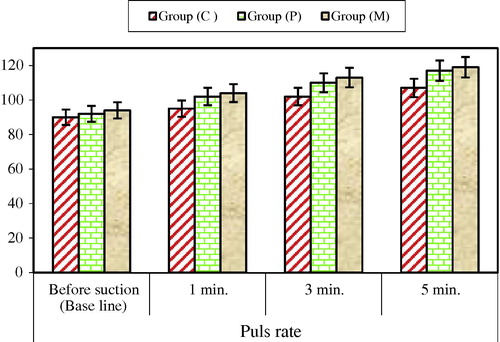
Hemodynamic changes: Before suction (baseline value): There were no significant differences between all groups as regards hemodynamic changes (pulse rate and blood pressure).
After suction and up to first 5 min after extubation: In the control group, there was significant increase in pulse rate and blood pressure in comparison with the baseline value (p < 0.001). In both Propofol and midazolam groups, there was significant decrease in blood pressure and increase in pulse rate in comparison with the baseline value which was significant statistically, and these changes were comparable and insignificant between both groups. Additionally, compared to the control group, both groups showed significant decrease in MAP and insignificant increase in pulse rate from the discontinuation of anesthetic drugs to 5 min after extubation as shown in and .
Incidence of postoperative laryngospasm (regardless of its severity) at time of extubation and up to 5 min was significantly lower (p < 0.05) in propofol and midazolam groups as compared to control group (see –).
able 2 Score of postextubation laryngospasm: (regardless of its severity).
able 4 Score of postextubation cough: (regardless of its severity).
Mild degree of laryngospasm was shown in 7 patients (17.5%) in control group, 15 patients (37.5%) in propofol group and 17 patients (42.5%) in midazolam group.
Moderate degree of laryngospasm was shown in 17 patients (42.5%) in control group, 7 patients (17.5%) in propofol group and 5 patients (12.5%) in midazolam group.
Sever degree of laryngospasm was shown in 12 patients (30%) in control group, 2 patients (5%) in propofol group and 4 patients (10%) in midazolam group.
The change in both propofol and midazolam groups was insignificant and comparable.
The incidence and grade of coughing during emergence was significantly lower in the propofol and midazolam groups compared to the control group. Grad (0) occur was shown in 4 patients (10%) in control group, 16 patients (40%) in propofol and 17 patients (42.5%) in midazolam group. Grad (1) occur was shown in 7 patients (17.5%) in control group, 16 patients (40%) in propofol and 15 patients (37.5%) in midazolam group. Grad (2) occur was shown in 14 patients (35%) in control group, 5 patients (17.5%) in propofol and 4 patients (10%) in midazolam group. Grad (3) occur was shown in 15 patients (37.5%) in control group, 3 patients (7.5%) in propofol and 4 patients (10%) in midazolam group. The change in both propofol and midazolam groups was insignificant and comparable as shown in .
able 5 Incidence of severity of postoperative cough (data present as number percentage).
Discussion
The main purpose of this study was to test the hypothesis that intravenous administration of small dose of propofol or midazolam before extubation would reduce the incidence and severity of postextubation laryngospasm and cough with safe hemodynamic changes in patients undergoing elective oropharyngeal surgeries.
Emergence from anesthesia and extubation induces variant physiological responses including unwanted circulatory and airway reflexes resulting in hypercirculatory manifestations in the form of tachycardia and hypertension and cough, laryngospasm, and bronchospasm. These events may predispose or induce multiple complications either in the operative site or elsewhere in the body [Citation15].
Various methods have been studied to prevent coughing during emergence from general anesthesia, such as extubation in a deep plane of anesthesia [Citation16], intra-cuff application of lidocaine [Citation17] or i.v. lidocaine [Citation18], and administration of dexmedetomidine [Citation19] and remifentanil [Citation20,Citation21]. These methods have various advantages, but they also have drawbacks so their clinical use can be.
In this study, when a single dose of propofol 0.8 mg/kg was administered at extubation before suction, it significantly reduced the incidence and severity of coughing during emergence as compared to control group, the NMDA inhibition effect of propofol is less likely to be the main mechanism for suppressing coughing, and there is need for more clinical studies regarding this matter. Such results are similar to a report that the incidence of coughing was reduced in children when propofol 0.25 mg/kg was used 1 min before extubation [Citation13].
In our study the administration of (100%) O2 + jaw thrust and positive pressure ventilation with the injection of intravenous drug therapy were done to relieve laryngospasm as well as cyanosis in most patients.
Subhypnotic doses of propofol (0.25–0.8 μg/kg) have been used previously for the treatment of postextubation laryngospasm [Citation22] and have proven effective. Propofol showed rapid action with no side-effects such as bradycardia or hypotension.
Benzodiazepines such as diazepam also decrease upper airway reflexes and have been previously used orally by Muphg et al. in the management and treatment of recurrent postoperative laryngospasm, and midazolam has been described to treat what is called psychogenic or hysterical stridor, which is most often seen in anxious adolescents and young adult [Citation23]
There have been various reported frequencies of cough during emergence from anesthesia. It is reported that they occur in 96% patients after extubation [Citation24]. Also, such cough responses occur from the chemically or mechanically sensitive ascending vagus nerve [Citation25]. However, cough responses are also affected by other ascending nerves and organs, the thorax, the diaphragm, and nerves connected to the abdominal muscles. It is not clear whether propofol can specifically suppress responses to airway irritation, yet there has been a report that it might be due to the diminishing effect of propofol on laryngeal responses. Also, propofol is considered to effectively suppress N-methyl-D-aspartate (NMDA) receptors and block the ascending pathway from the trachea [Citation26].
Our study also showed that both midazolam and propofol groups are associated with a significant and comparable increase in HR and decrease in MAP (but still within normal ranges) after administration of the study drugs and up to 5 min after extubation compared to control group. Propofol can significantly decrease the arterial pressure according to the dosage used during anesthetic induction [Citation27], and this appears in relation to systemic vascular resistance and a decrease in cardiac output. In addition, it does not have a significant direct effect on HR, but it may increase [Citation28]. In another study, a subhypnotic dose (0.3 mg/kg) of propofol can significantly increase the MAP and HR from the discontinuation of anesthetic drugs and up to 10 min in PACU. These results are considered to be because only a small dose of propofol was used in this study, and it did not have a significant effect on the change in MAP and HR during emergence. Another study shows significant decrease in the mean arterial pressure and heart rate in both propofol and midazolam groups after administration of the study drugs, and this decrease was comparable and similar in both groups, which is directly attributed to the relief from anxiety and hypoxia associated with laryngospasm.
Two potential limitations should be considered. First, the sample size enrolled in our study was limited to adult patients, and hence, it cannot predict the coughing suppression effect of propofol during emergence in pediatric patients receiving the same doses scheduled in our study, so further investigations are needed on wider population with different ages in order to concur our results, to confirm their safety, and to support the absence of any complications. Second, there are difficulties in adequately blinding studies as propofol is white solution. However, neither the surgeon nor the anesthesiologist conducting assessment was aware of the group allocation. We can conclude that the use of Propofol in a small dose (0.8 mg kg−1 body weight) or midazolam (0.05 mg kg−1 body weight) found to be useful drugs to relieve postextubation laryngeal spasm in most patients undergoing oropharyngeal surgeries. Because it was not found to be effective in all patients, succinylcholine still has a role to play in critical conditions. However, we recommend propofol or midazolam as a suitable alternative for relieving laryngeal spasm in situations where succinylcholine is contraindicated.
Conflict of interest
The authors declare that there are no conflicts of interest.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- J.M.BlairD.A.HillJ.P.FreeTracheal intubating conditions after induction with sevoflurane 8% in children. A comparison of two intravenous techniquesAnaesthesia552000774778
- A.B.S.HobaikaM.N.LorentzLaryngospasmRev Bras Anestesiol592009491495
- S.ChaudharyN.MakhijaR.S.RautelaV.MahajanR.ChawlaPost tracheal extubation laryngospasm induced pulmonary oedema. Department of Anaesthesiology and Critical care, University College of Medical Sciences and Guru Teg Bahadur Hospital DelhiAnaesth Clin Pharmacol1431998300302
- S.P.PadleyM.O.DownesCase report – pulmonary oedema secondary to laryngospasm following general anaesthesiaBrit J Radiol671994654655
- C.KocF.KocamonE.AygenecC.OzdemA.CekieThe use of preoperative lidocaine to prevent stridor and laryngospasm after tonsillectomy and adenoidectomyOtolaryngol Head Neck Surg1181998880882
- J.G.StaffelM.C.WeisslerE.P.TylerA.F.DrakeThe prevention of postoperative stridor and laryngospasm with topical lidocaineArch Otolaryngol Head Neck Surg117199111231128
- A.ZeidenD.HalabiA.BarakaAerosolized lidocaine for relief of extubation laryngospasmAnesth Analg10120051563
- A.N.SibaiI.YamoutNitroglycerin relieves laryngospasmActa Anaesthesiol Scand43199910811083
- G.AfshanU.ChohanU.I.QamarR.S.KamalIs there a role for a small dose of propofol in treatment of laryngeal spasm?Paediatr Anaesth122002625628
- N.GulhasM.DurmasS.DemerbilekThe use of magnesium to prevent laryngospasm after tonsillectomy and adenoidectomy: a preliminary studyPaediatr Anaesth1320034347
- K.McKeatingI.M.BaliJ.W.DundeeThe effects of thiopentone and propofol on upper airway integrityAnaesthesia431988638640
- Y.K.BatraM.IvanovaS.S.AliM.ShamsahA.R.Al QattanK.G.BelaniThe efficacy of a subhypnotic dose of propofol in preventing laryngospasm following tonsillectomy and adenoidectomy in childrenPaediatr Anaesth15200510941097
- H.J.PakW.H.LeeS.M.JiY.H.ChoiEffect of a small dose of propofol or ketamine to prevent coughing and laryngospasm in children awakening from general anesthesiaKorean J Anesthesiol6020112529
- E.S.KimM.J.BishopCough during emergence from isoflurane anesthesiaAnesth Analg87199811701174
- P.B.K.ChanOn smooth extubation without coughing and bucking [4]Can J Anesth492002324
- G.NeelakantaJ.MillerMinimum alveolar concentration of isoflurane for tracheal extubation in deeply anesthetized childrenAnesthesiology801994811813
- C.FaganH.P.FrizelleJ.LaffeyV.HannonM.CareyThe effects of intracuff lidocaine on endotracheal tube induced emergence phenomena after general anesthesiaAnesth Analg912000201205
- T.VenkatesanG.KorulaA comparative study between the effects of 4% endotracheal tube cuff lignocaine and 1.5 mg/kg intravenous lignocaine on coughing and hemodynamics during extubation in neurosurgical patients: a randomized controlled double-blind trialJ Neurosurg Anesthesiol182006230234
- G.GulerA.AkinZ.TosunE.EskitascogluA.MizrakA.BoyaciSingle-dose dexmedetomidine attenuates airway and circulatory reflexes during extubationActa Anaesthesiol Scand49200510881091
- J.H.LeeB.N.KooJ.J.JeongH.S.KimJ.R.LeeDifferential effects of lidocaine and remifentanil on response to the tracheal tube during emergence from general anaesthesiaBr J Anaesth1062011410415
- M.T.AouadA.A.Al-AlamiV.G.NasrF.G.SoukiR.A.ZbeidyS.M.Siddik-SayyidThe effect of low-dose remifentanil on responses to the endotracheal tube during emergence from general anesthesiaAnesth Analg108200911571160
- M.NawfalA.BarakaPropofol for relief of extubation laryngospasmAnaesthesia5720021028
- S.E.GoldenThe management and treatment of recurrent postoperative laryngospasmAnesth Analg84199713891396
- J.P.EstebeG.DolloP.Le CorreA.Le NaouresF.ChevanneR.Le VergeAlkalinization of intracuff lidocaine improves endotracheal tube-induced emergence phenomenaAnesth Analg942002227230
- J.G.WiddicombeAfferent receptors in the airways and coughRespir Physiol1141998515
- B.A.OrserM.BertlikL.Y.WangJ.F.MacDonaldInhibition by propofol (2,6 di-isopropylphenol) of the N-methyl-D-aspartate subtype of glutamate receptor in cultured hippocampal neuronesBr J Pharmacol116199517611768
- P.S.PagelD.C.WarltierNegative inotropic effects of propofol as evaluated by the regional preload recruitable stroke work relationship in chronically instrumented dogsAnesthesiology781993100108
- H.StephanH.SonntagH.D.SchenkD.KettlerH.J.KhambattaEffects of propofol on cardiovascular dynamics, myocardial blood flow and myocardial metabolism in patients with coronary artery diseaseBr J Anaesth581986969975