?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
The purpose was to study the effect of recombinant human erythropoietin (rHuEPO) and iron or iron alone with acute normovolemic hemodilution (ANH) on blood transfusion requirements in elective myomectomy patients.
Methods
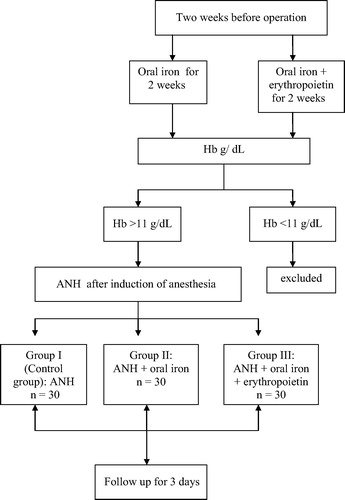
Ninety female patients scheduled for myomectomy and ANH after induction of general anesthesia were randomly allocated into three equal groups (30 patients each); Group I (control group): Patients scheduled for ANH alone; Group II: Patients received oral ferrous iron sulfate 320 mg tablets twice daily for 2 weeks before surgery; and Group III: Patients received oral ferrous iron sulfate 320 mg tablets twice daily and recombinant human erythropoietin (rHuEPO) in a dose of 100 IU/kg subcutaneously twice a week for 2 weeks before surgery.
Results
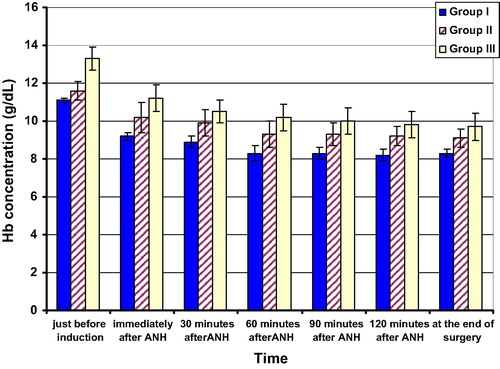
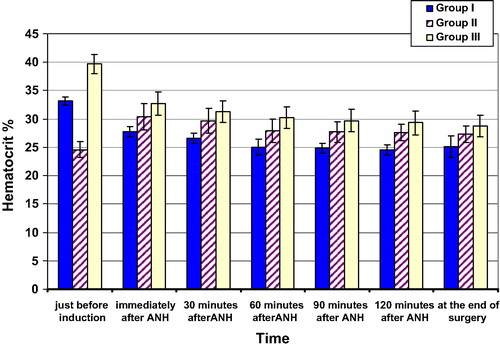
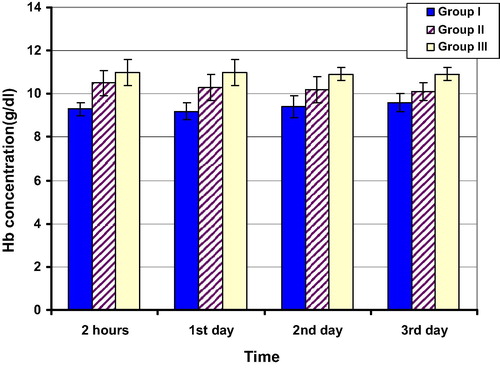
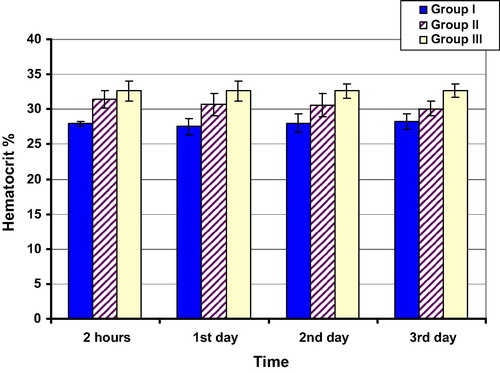
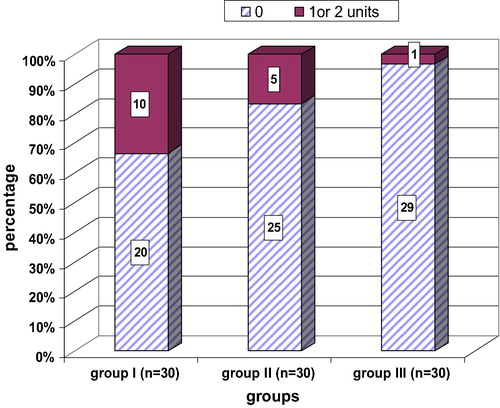
There was a significant increase in Hb (g/dL) and Hct % (p < 0.0001) in groups II and III compared to group I, and in group III compared to group II at all the predetermined times. There was a significant increase in blood volume that can be removed by ANH (ml) in groups II (1250 ± 280) and III (1986.7 ± 292.8) compared to group I (987. 4 ± 176.6), and in group III compared to group II (p < 0.001). The median number of blood units removed by ANH was significantly increased in group III {3 (1–3)} compared to groups I and II {2 (1–3)} (p < 0.001). The number of patients who received homologous blood transfusion was decreased in group III [1 (3.33%)] compared to the two other groups, and in group II [5 (16.7%)] compared to group I [10 (33.3%)].
Conclusion
Preoperative iron alone or iron and erythropoietin added to acute normovolemic hemodilution help to reduce the need for allogenic blood transfusion in myomectomy patients. Further studies are needed to evaluate their use in older patients with higher risk for thrombosis and hypertension.
Introduction
Homologous blood transfusion faces many difficulties including the safety, high costs and limited supply. So, there is a need to minimize transfusion of blood components [Citation1], and a restrictive transfusion strategy in hemodynamically stable patients is recommended [Citation2].
Acute normovolemic hemodilution (ANH) has the benefit of reducing blood loss, as whole blood is shed perioperatively at lower hematocrit (% Hct) values. Also, platelets and coagulation factors remain functional because the blood collected by ANH is returned to the patient within 8 h of collection and is stored at room temperature in the operating room. In addition, testing the blood units is not essential [Citation3].
The most important risk factor for blood transfusion is pre-existing anemia [Citation4] which may be present in about 75% of patients scheduled for elective surgery [Citation5]. The most common cause of impaired erythropoiesis is absolute deficiency of iron stores especially in young children, pregnant and premenopausal women and elderly people [Citation6]. Their management depends on repletion of iron stores and most patients respond well to oral iron therapy [Citation7]. Erythropoietin increases the preoperative hemoglobin (Hb), hematocrit % (Hct %), and production of red blood cells (RBCs) [Citation8]. So, the aim of this work was to study the effect of adding erythropoietin and iron or iron alone to acute normovolemic hemodilution (ANH) on blood transfusion requirements in elective myomectomy patients.
Patients and methods
This study was carried out in Tanta University Hospital from September 2012 to September 2013 on 90 female patients scheduled for elective myomectomy at the Gynecology and Obstetric Department after obtaining an institutional board approval. A written informed consent was obtained from each patient or their closest relative and all the data in the study were confidential; every patient had a secret code and private file and the results were used for scientific purpose only.
The trial is registered in the Australian New Zealand Clinical Trials Registry: ACTRN12615000152527.
The primary end point of the study in each group was the percentage of patients who received homologous blood transfusion and the number of homologous blood units they received in the first 3 postoperative days. The sample size for each group was calculated based on the data of a previous pilot study in our institute. Thirty patients in each group were required for erythropoietin and iron to decrease the percentage of homologous blood transfusion by about 30%, with 90% power and a cutoff of 0.05% for statistical significance.
Patients aged >18 and <60 years with hemoglobin level >11 g/dL at the time of ANH were included in this study, while, patients who refused to participate in the study and received blood or blood components in the preceding 4 weeks, with severe hepatic, renal or heart disease were excluded from the study.
Patients were randomly allocated into three equal groups (30 patients each): Group I (control group): Patients scheduled for ANH alone after induction of general anesthesia; Group II: Patients received oral ferrous iron sulfate 320 mg tablets twice daily for 2 weeks before surgery and scheduled for ANH after induction of general anesthesia; and Group III: Patients received oral ferrous iron sulfate 320 mg tablets twice daily and recombinant human erythropoietin (rHuEPO) in a dose of 100 IU/kg subcutaneously twice a week for 2 weeks before surgery and scheduled for ANH after induction of general anesthesia. Randomization between groups II and III (treatment groups) was done using closed sealed envelops and computer generated random numbers two weeks before surgery, while, patients of the control group were selected randomly at the time of operation. A blinded nurse, who did not participate in data collection read the patient’s number.
The ANH was started just after tracheal intubation, and the volume to be withdrawn was calculated (maximum 3 units), while maintaining the Hct level >28%. The first 1000 cc of blood withdrawn was replaced with equal volume of hydroxy-ethyl starch 6%, then any additional blood was replaced with crystalloid solution in the ratio of 3:1.
Hemoglobin (Hb) and hematocrit (Hct) % were measured preoperatively 2 weeks (baseline values) and one week before surgery; intra-operatively just before induction of anesthesia, immediately after ANH then at 30, 60, 90, 120 min and at the end of surgery; and Postoperatively; after 2 h and, once daily for the first 3 days. The number of patients in each group who received homologous blood transfusion and, the number of units they received was recorded.
The volume of blood that could be withdrawn during ANH from each patient was calculated using the following formula [Citation9]:
V = Volume of blood that could be removed. EBV = Estimated blood volume. Hi = initial hematocrit level. Hf = the target hematocrit level following ANH. Hav = the average hematocrit level of Hi and Hf.
The number of blood units withdrawn by ANH was recorded, and the volume of blood loss was estimated by estimation of blood in the surgical sponges (5 mildly, 10 → moderately, and 15 → severely soaked) and pads (50 → mildly, 100 → moderately, and 150 → severely soaked) and, by observing the volume of blood in the suction apparatus and the surgical drains.
Blood transfusion was given if Hb level was <8 g/dL and, if there was abnormal ECG, ischemic heart disease or obstructive lung disease and the Hb level was 8–10 g/dL. No transfusion was given if Hb level was >10 g/dL [Citation10]. If the patient was in-need for blood transfusion, the blood removed by ANH was given first, starting with the last unit collected then, homologous blood. At the end of surgery all autologous blood units were returned to the patient.
All patients were pre-medicated with 0.01 mg/kg midazolam before induction of anesthesia and monitored for ECG, oxygen saturation, capnograph and non-invasive blood pressure. A urinary catheter was inserted for collection of urine output. The patients were pre-oxygenated with oxygen 100% for 5 min, then anesthesia was induced with 2 mg/kg propofol and 1 μg/kg fentanyl and tracheal intubation was facilitated with cisatracurium 0.3 mg/kg. Anesthesia was maintained with oxygen 100%, isoflurane 1–1.5%, fentanyl 0.5 μg/kg every 30 min and incremental doses of cisatracurium for muscle relaxation and mechanical ventilation to maintain normocapnia. At the end of surgery, anesthesia was discontinued and muscle relaxants were reversed with neostigmine 0.04 mg/kg and atropine 0.01 mg/kg. The patient was extubated when she was fully awake. The occurrence of any complication was recorded.
The data were analyzed using SPSS (version 20), quantitative data were expressed as mean ± SD (for age, weight, preoperative platelet count, duration of anesthesia, Hb (g/dL), Hct %, estimated blood volume, volume of blood that can be removed by ANH, and volume of blood loss) and analyzed using F Test for comparison within the same group and among the three groups, and Tukey’s test is used as post hoc test and independent-t-test for comparison between the groups III and II for Hb (g/dL) and Hct % preoperatively. The number of blood units removed by ANH (did not follow the normal distribution) was expressed as median (range) and Kruskal–Wallis H test was used for comparison among the studied groups, while, the ASA, the number of patients who received homologous blood transfusion, and complications were expressed as number %. P < 0.05 was considered statistically significant.
Results
The studied groups were comparable for age, weight, ASA state, preoperative platelet count and time of anesthesia (p > 0.05) () ().
able 1 Patient characteristics and duration of anesthesia (minutes) in the studied groups.
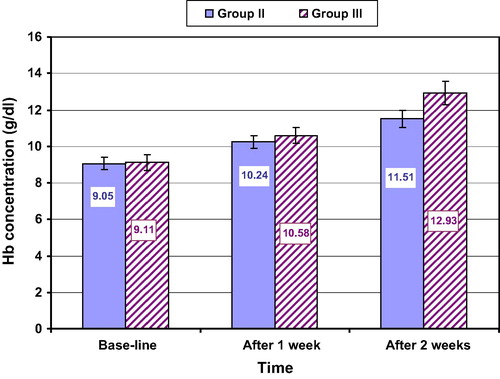
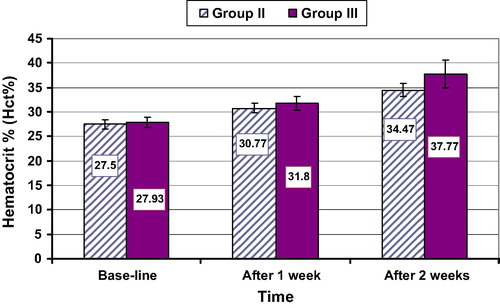
Preoperatively in groups II and III there was a significant increase in the values of Hb (g/dL) and Hct % 1 and 2 weeks after treatment compared to their baseline values in both groups; the values after the second week were significantly higher than those after the first week in both groups (p < 0.001). The two groups were comparable for the baseline Hb (g/dL) (p = 0.572) and Hct % (p = 0.108) then, there was a significant increase in the mean values of Hb in group III compared to group II after 1 (p = 0.001) and 2 weeks (p < 0.0001) and Hct % (p = 0.002 and <0.001) after 1 and 2 weeks respectively ( and ). The values of Hb (g/dL) and Hct % in groups II and III were significantly higher compared to group I, and higher in group III compared to group II (p < 0.0001) at all the predetermined times during intra-operative and post-operative periods ().
The volume of blood that can be removed by ANH (ml) was increased significantly in groups II and III compared to group I, and in group III compared to group II (p < 0.001). The median number of blood units removed by ANH was increased significantly in group III compared to groups I and II (p < 0.001), while, there was no significant difference among the three studied groups as regards the estimated blood volume (p = 0.7) and the blood loss (p = 0.5) ().
able 2 ANH related blood volumes (ml) in the studied groups.
As regards the number of patients who did not receive homologous blood units, it was increased significantly in group III [29 (96.66%)] compared to the two other groups, and in group II [25 (83.33%)], compared to group I [20 (66.66%)]. Consequently the number of patients who received homologous blood transfusion was decreased in group III [1 (3.33%)], compared to the two other groups and in group II [5 (16.7%)], compared to group I [10 (33.3%)] ().
There were few complications related to oral iron therapy; 8 (26.6%) patients in group II and 7 (23.3%) patients in group III had constipation, while, 5 (16.6) patients in group II and 6 (20%) patients in group III had heartburn. There were no serious complications related to erythropoietin therapy e.g. hypertension or thrombosis.
Discussion
As regards the Hb and Hct % in the present study, preoperatively, one and two weeks after treatment, there was a significant increase in Hb and Hct % in groups II and III compared to their baseline values which can be explained by the fact that normal heme production and erythropoiesis depend on adequate iron stores [Citation11]. This is in agreement with the study of Prasad et al. [Citation12], and Yang et al. [Citation13], while, Mundy et al. [Citation14] found that oral ferrous sulfate was not effective in treatment of anemia associated with hip or knee surgeries. They postulated that the inflammatory response to surgical trauma affects iron metabolism through the release of interleukins, tumor necrosis factor and endotoxins, and Parker [Citation15], and Lachance et al. [Citation16] found similar results. This may be attributed to the different patient population in those studies, older patients with orthopedic trauma, while the patients in the present study were younger with chronic blood loss.
There was a significant increase in the mean values of Hb and Hct % in group III compared to group II after 1 and 2 weeks of treatment which could be explained on the basis of the role of erythropoietin in erythropoiesis as it affects positively the last step of erythrocyte production in mammals through binding to its specific receptor leading to induction of proliferation and differentiation of erythroid progenitors [Citation17]. Similar results were obtained by Kosmadakis et al. [Citation18], Hudis et al. [Citation19], Bovy et al. [Citation20], and Silver et al. [Citation21].
Moreover, we found a significant increase in Hb and Hct % in groups III and II compared to group I, and in group III compared to group II at all predetermined times in the intra- and postoperative periods. This can be explained by the fact that iron stores of the patients were deficient preoperatively due to repeated blood loss so, the values of Hb and Hct % in group II were better than those of group I. The induction of erythropoiesis after erythropoietin therapy may exacerbate borderline iron deficiency and oral iron supplementation is very important to obtain the best results [Citation22] so, the best results were obtained with group III. The results obtained by Corwin et al. [Citation23], Karkouti et al. [Citation24], Kateros et al. [Citation25], Laffosse et al. [Citation26], Lepor et al. [Citation27] and Delasotta et al. [Citation28] are in agreement with our results. Contrary to our results, Madi-Jebara et al. [Citation29] and Karkouti et al. [Citation30] reported weak response of erythropoietin and iron for correction of severe postoperative anemia (despite accelerated erythropoiesis as indicated by increased reticulocytic count). This may be caused by the negative effect of inflammation on erythropoietin receptor and the pro-inflammatory cytokines may have an inhibitory effect on erythroid progenitor cells and disturb iron metabolism in the postoperative period [Citation31] while, we used erythropoietin and iron 1 and 2 weeks preoperatively; moreover, Madi-Jebara et al. [Citation29] used a single low dose of erythropoietin (300 IU) which is less than the dose used in the present study.
A significant increase in the volume of blood that could be removed by ANH was observed in groups III and II compared to group I, and in group III compared to group II. Also, the median number of blood units removed by ANH was significantly increased in group III compared to the other two groups. Similar results were obtained by Sonzogni et al. [Citation32] and Bovy et al. [Citation20].
Concerning the number of patients who received homologous units, comparison among the studied groups revealed that it decreased significantly in group III compared to the other two groups. The results reported by Corwin et al. [Citation23], Karkouti et al. [Citation24], Silver et al. [Citation21], Kateros et al. [Citation25], Laffosse et al. [Citation26], Yoo et al. [Citation33], Cladellas et al. [Citation34] and Delasotta et al. [Citation28] are in agreement with our results, while, Grobmyer et al. [Citation35] disagreed with our results, as they found no significant difference in the transfusion rate between groups and this may be due to inhibition of erythropoiesis in their patients (abdominal and pelvic malignancies) by several mediators including tumor necrosis factor alpha, interleukin-1 and 6 and transforming growth factor-beta [Citation36].
As regards the complications, there were few minor complications related to oral iron therapy and could be tolerated (did not need any treatment); 8 (26.6%) patients in group II and 7 (23.3%) patients in group III had constipation, while, 5 (16.6) patients in group II and 6 (20%) patients in group III had heartburn. There were no serious complications related to erythropoietin therapy e.g. hypertension or thrombosis.
We conclude that, preoperative iron alone or iron and erythropoietin added to acute normovolemic hemodilution help to reduce the need for allogenic blood transfusion in myomectomy patients. The study has some limitations as, the participants were middle aged females, so the safety of erythropoietin in older, hypertensive or cardiac male patients must be studied. Also, it is better to be repeated on a larger sample size.
Conflict of interest
None declared.
Funding
The researchers supported this work fund.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- A.ShanderA.HofmannJ.IsbisterH.Van AkenPatient blood management – the new frontierBest Pract Res Clin Anesthesiol272013510
- R.A.ZolloM.P.EatonM.KarezR.PasternakL.G.GlanceBlood transfusion in the peri-operative periodBest Pract Res Clin Anesthesiol262012475484
- D.R.SpahnL.T.GoodnoughBlood transfusion 2. Alternatives to blood transfusionLancet38120131885518865
- L.T.GoodnoughA.ManiatisP.EarnshawG.BenoniP.BerisE.BisbeD.A.FergussonDetection, evaluation, and management of preoperative anemia in the elective orthopedic surgical patient: NATA guidelinesBr J Anaesth10620111322
- P.BerisM.MuñozJ.A.García-ErceD.ThomasA.ManiatisP.Van der LindenPerioperative anemia management: consensus statement on the role of intravenous ironBr J Anaesth10052008599604
- D.RajeH.MukhtarA.OshowoC.I.ClarkWhat proportion of patients referred to secondary care with iron deficiency anemia have colon cancer?Dis Colon Rectum50200712111214
- L.T.GoodnoughIron deficiency syndromes and iron-restricted erythropoiesisTransfusion527201215841592
- C.CouvertRecombinant human erythropoietin and management of anemia in orthopedic surgeryTransfus Altern Transfus Med820065257
- P.P.OppitzM.A.StefaniAcute normovolemic hemodilution is safe in neurosurgeryWorld Neurosurg792013719724
- G.SandersN.MellorK.RickardsA.RushtonI.ChristieJ.NichollProspective randomized controlled trial of acute normovolemic hemodilution in major gastrointestinal surgeryBr J Anaesth9362004775781
- P.M.SuttonT.CresswellJ.P.LiveseyK.SpeedT.BaggaTreatment of anemia after joint replacement. A double blind, randomized, controlled trial of ferrous sulfate versus placeboJ Bone Joint Surg (Br)8620043133
- N.PrasadV.RajamaniD.HullinJ.M.MurrayPost-operative anaemia in femoral neck fracture patients: does it need treatment? A single blinded prospective randomised controlled trialInjury4010200910731076
- Y.YangH.LiB.LiY.WangS.JiangL.JiangEfficacy and safety of iron supplementation for the elderly patients undergoing hip or knee surgery: a meta-analysis of randomized controlled trialsJ Surg Res17122011e201e207
- G.M.MundyS.J.BirtwistleR.A.PowerThe effect of iron supplementation on the level of haemoglobin after lower limb arthroplastyJ Bone Joint Surg Br8722005213217
- M.J.ParkerIron supplementation for anemia after hip fracture surgery: a randomized trial of 300 patientsJ Bone Joint Surg Am9222010265269
- K.LachanceM.SavoieM.BernardS.RochonJ.FafardR.RobitailleP.A.VendittoliS.LévesqueS.de DenusOral ferrous sulfate does not increase preoperative hemoglobin in patients scheduled for hip or knee arthroplastyAnn Pharmcother4562011764770
- D.VittoriN.PregiG.PérezG.GarbossaA.NesseThe distinct erythropoietin functions that promote cell survival and proliferation are affected by aluminum exposure through mechanisms involving erythropoietin receptorBiochim Biophys Acta17431–220052936
- N.KosmadakisE.MessarisA.MarisS.KatsaragakisE.LeandrosM.M.KonstadoulakisG.AndroulakisPerioperative erythropoietin administration in patients with gastrointestinal tract cancer. Prospective randomized double-blind studyAnn Surg23732003417421
- C.A.HudisC.L.VogelJ.R.GralowD.WilliamsWeekly epoetin alfa during adjuvant chemotherapy for breast cancer: effect on hemoglobin levels and quality of lifeClin Breast Cancer622005132142
- C.BovyE.BaudouxJ.P.SalmonY.BeguinIncreased iron absorption during autologous blood donation supported by recombinant human erythropoietin therapyTransfusion469200616161623
- M.SilverM.J.CorwinA.BazanA.GettingerC.EnnyH.L.CorwinEfficacy of recombinant human erythropoietin in critically ill patients admitted to a long-term acute care facility: a randomized, double-blind, placebo-controlled trialCrit Care Med349200623102316
- M.CladellasJ.BrugueraJ.Comin-coletIron therapy alone or in combination with erythropoietin in surgical and medical cardiac patientsTransfus Altern Transfus Med122012143149
- H.L.CorwinA.GettingerR.G.PearlM.P.FinkM.M.LevyM.J.ShapiroM.J.CorwinEfficacy of recombinant human erythropoietin in critically ill patients: a randomized controlled trialJAMA28822200228272835
- K.KarkoutiS.A.McCluskeyL.EvansN.MahomedM.GhannamR.DaveyErythropoietin is an effective clinical modality for reducing RBC transfusion in joint surgeryCan J Anaesth5242005362368
- K.KaterosV.I.SakellariouI.P.SofaianosP.J.PapagelopoulosEpoetin alpha reduces blood transfusion requirements in patients with intertrochanteric fractureJ Crit Care2522010348353
- J.M.LaffosseV.MinvilleP.ChironA.ColombaniC.GrisJ.C.PourrutB.EychenneO.FourcadePreoperative use of epoietin beta in total hip replacement: a prospective studyArch Orthop Trauma Surg130120104145
- H.LeporM.LipkinD.SlovaThe preoperative use of erythropoietin stimulating proteins prior to radical prostatectomy is not associated with increased cardiovascular or thromboembolic morbidity or mortalityUrology756201014241428
- L.A.DelasottaF.OrozcoS.M.JafariJ.L.BlairA.OngShould we use preoperative epoetin- in the mildly anemic patient undergoing simultaneous total knee arthroplasty?Open Orthop J720134750
- S.N.Madi-JebaraG.S.SleilatyP.E.AchouhA.G.YazigiF.A.HaddadG.M.HayekM.C.AntaklyV.A.JebaraPostoperative intravenous iron used alone or in combination with low-dose erythropoietin is not effective for correction of anemia after cardiac surgeryJ Cardiothorac Vasc Anesth18120045963
- K.KarkoutiS.A.McCluskeyM.GhannamM.J.SalpeterI.QuirtT.M.YauIntravenous iron and recombinant erythropoietin for the treatment of postoperative anemiaCan J Anaesth53420061119
- K.van der PuttenB.BraamK.E.JieC.A.GaillardMechanisms of disease: erythropoietin resistance in patients with both heart and kidney failureNat Clin Pract Nephrol4120084757
- V.SonzogniG.CrupiR.PomaF.AnnechinoF.FerriP.FilisettiP.BellavitaErythropoietin therapy and preoperative autologous blood donation in children undergoing open heart surgeryBr J Anaesth8732001429434
- Y.C.YooJ.K.ShimJ.C.KimY.Y.JoJ.H.LeeY.L.KwakEffects of single recombinant human erythropoietin injection on transfusion requirements in preoperatively anemic patients undergoing valvular heart surgeryAnesthesiol11552011929937
- M.CladellasN.FarréJ.Comín-ColetM.GómezO.MeroñoM.A.BoschJ.VilaEffects of preoperative intravenous erythropoietin plus iron on outcome in anemic patients after cardiac valve replacementAm J Cardiol1107201210211026
- S.R.GrobmyerA.W.HemmingN.HarrisK.BehrnsH.LoganA pilot prospective randomized trial of postoperative epoetin alfa in patients undergoing major operation for upper gastrointestinal malignancyAm J Clin Oncol3262009570573
- N.CasadevallCellular mechanism of resistance to erythropoietinNephrol Dial Transplant10619952730