?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Laparoscopic surgery produces measurable effects on cardio-circulatory, respiratory and metabolic systems. Total intravenous anesthesia with propofol using target-controlled infusion technique guided by Bispectral Index monitoring ensures an optimum level of anesthesia. This study was designed to evaluate the hemodynamic changes with the use of BIS-guided TCI with propofol-fentanyl during either laparoscopic or open cholecystectomy.
Methods
Twenty-four ASA class I-II patients, scheduled for cholecystectomy under general anesthesia using BIS-guided TIVA with propofol-fentanyl delivered by TCI pump, were divided surgically into laparoscopic surgery group (LS group, n = 12) and open surgery group (OS group, n = 12). Hemodynamic data as well as stress hormones were measured at various time intervals.
Results
Within LS, there was rise of both cardiac output after abdominal insufflation (p < 0.05) and stroke volume after end of surgery (p < 0.05). Blood pressure decreased in the two groups after insufflation in LS and skin incision in OS (p < 0.01) as well as after 15 min (p < 0.05 & p < 0.01 respectively). LS showed decrease in SVR starting from insufflation till end of surgery, while OS showed this decrease only with skin incision. Heart rate decreased 15 min after surgical incision till end of surgery in OS while LS showed decrease only after end of surgery. Only in OS, norepinephrine & epinephrine levels showed significant rises throughout the period of study (p < 0.001). Cortisol level was elevated after 30 min in LS while OS showed a rise after the end of surgery (p < 0.001). ACTH levels increased in OS (p < 0.001). There was positive correlation between CO and epinephrine, norepinephrine and ACTH in OS.
Conclusion
BIS-guided TCI anesthesia with propofol-fentanyl offers a good and safe anesthesia technique for patients undergoing either laparoscopic or open cholecystectomy. The hemodynamic stability guided by esophageal Doppler monitor makes it a very appealing choice.
Abbreviations:
- TIVA
- Total intravenous anesthesia
- TCI
- target-controlled infusion
- BIS
- Bispectral Index
- EDM
- Esophageal Doppler ultrasonography monitoring
- TBRI
- Theodor Bilharz Research Institute
- ASA
- American society of anesthesiologists
- MBP
- mean blood pressure
- HR
- heart rate
- BMI
- body mass index
- Ce
- effect site concentration
- TOF
- train of four
- Ftc
- flow time corrected
- PV
- peak velocity
- SD
- stroke distance
- MA
- mean acceleration
- MD
- minute distance
- SV
- stroke volume
- CO
- cardiac output
- SVR
- systemic vascular resistance
- ACTH
- Adreno Cortico Trophic Hormone
- IAP
- intra-abdominal pressure
- CI
- cardiac index
Introduction
Laparoscopy for operative purposes most commonly cholecystectomy offers specific advantages to the patient. Apart from the anesthetic appeal, the shorter hospital stay and decreased postoperative morbidity are particularly strong arguments for laparoscopic surgery which became now a favored approach for surgeons [Citation1]. Laparoscopic surgery necessitates intra-abdominal gas insufflation (usually CO2) for inducing an artificial pneumoperitoneum with controlled intra-abdominal pressure. This implies cardio-circulatory, respiratory and metabolic changes [Citation2,Citation3]. Abdominal CO2 insufflation probably has some impact on the cardiovascular system with uncertain clinical significance [Citation4]. The need to extend laparoscopic surgery to extreme age groups with systemic complications calls for reevaluation of hemodynamic monitoring during these procedures [Citation5].
Propofol is usually the drug of choice during Total intravenous anesthesia (TIVA) because of its smooth induction, rapid recovery, short half life and negligible postoperative complications. The availability of target-controlled infusion (TCI) pumps allowed better control of its plasma levels thus increasing its safety and minimizing its side effects [Citation6].
TCI permits infusion of drugs at predefined rates according to a pharmacokinetic profile to reach a preset blood/site concentration. TCI system uses age, gender and weight of the patient to incorporate them into a pre-programmed pharmacokinetic model describing the distribution and elimination of the drug in the body. The target drug concentration is entered to the pump allowing it to calculate the loading bolus and maintenance infusion rates to maintain it constant [Citation7]. Optimization of TCI using Bispectral Index (BIS) monitoring ensures an optimum level of anesthesia with the minimum blood/site concentration and, hence, hemodynamic changes.
The thermodilution technique using pulmonary artery catheter is associated with several limitations [Citation1]. Esophageal Doppler ultrasonography monitoring (EDM) is an alternative technique for measuring cardiac output providing continuous inexpensive and relatively non-invasive tool. It is easy to insert and operate with minimal patient morbidity [Citation8]. Its use during abdominal surgery improved patient’s outcome mainly at the level of hospital stay, which is the optimal goal of laparoscopic surgery [Citation9].
Thus, the authors tested the hypothesis that the use of BIS-guided TCI with propofol-fentanyl might optimize the hemodynamic fluctuations previously reported with other anesthesia techniques during either laparoscopic or open cholecystectomy. The primary outcome observed in this study would be the effect of this technique on the cardiac output as measured using ODM, while the secondary outcome was the remaining hemodynamic variables as well as the stress hormones.
Subjects, materials and methods
After obtaining Ethical Committee approval of Theodor Bilharz Research Institute (TBRI) and patients’ written informed consents, this study was conducted on twenty-four adult patients (25–55 years old) ASA physical status I or II of either sex scheduled for laparoscopic or open cholecystectomy under general anesthesia using TIVA with propofol-fentanyl delivered by TCI pump. The study exclusion criteria were as follows: esophageal abnormalities, obesity class II or III (BMI > 35 kg m−2), pregnancy and lactation, chronic liver disease, diabetes mellitus, severe renal, endocrine, rheumatic, cardiopulmonary disease or malignancy and patients receiving medications with known effects on the sympathetic response or the hormonal secretion e.g. β-Blockers.
Power analysis was performed using a general power analysis program (G∗ power 3.0.10, Kiel, Germany). The power calculation was used to determine the minimum sample size, assuming an alpha of 0.05 at 80% power, based on an effect size of 0.58. A sample size of twelve patients per group would be required.
Patients fitting these inclusion criteria and scheduled for cholecystectomy either laparoscopic or open were included (the decision for the surgical technique was taken by the surgeon in charge). They were divided into two groups of twelve patients each: laparoscopic surgery group (group LS) or open surgery group (group OS).
Preoperative evaluation and routine preoperative investigations were done. Clinical examination included measuring body weight and height to calculate body mass index (BMI). Midazolam (0.05 mg kg−1) and ondansetron (4 mg) were given IM half an hour before operation as premedication. Patients were then transferred to the operating room. An 18G intravenous Teflon cannula was inserted in the contra-lateral antebrachial vein and was strictly reserved to propofol infusion. Ringer solution was then transfused at a rate of 6 ml kg−1 h−1 in the next 15 min. The following monitors were attached to the patients before the start of anesthesia: 5 leads ECG, non-invasive arterial blood pressure, peripheral oxygen saturation, end-tidal carbon dioxide tension, inhaled anesthetic gas analysis and neuromuscular monitoring (Infinity Kappa, Dräger, Lübeck, Germany). BIS module (Infinity®BISx TM SmartPod®) was attached to the monitor for consciousness level detection. Disposable BIS electrodes (BIS quatro, Aspect Medical Systems, USA) were placed on the forehead after cleaning the skin with alcohol. Temperature was monitored using a nasopharyngeal probe and normothermia was maintained with standard warming devices (Hawksley’s™ RippleHeat patient under-body water-filled mattress warming system, UK & 3M™ Bair Hugger™ model 750 warming unit using a whole over-body blanket with a surgical access, USA).
All basic readings were recorded before the beginning of anesthesia. Before induction, patients were pre-oxygenated with 8 l min−1 100% oxygen for 5 min. The Injectomat TIVA Agilia infusion pump (FresiniusKabi, Hamburg, Germany) was used in all cases. A 50 cc syringe filled with 1% propofol (10 mg ml−1) was loaded in the pump and attached to the peripheral IV cannula using a venous extension line. Anesthesia induction began with the use of IV fentanyl 2 μg kg−1. Intravenous propofol infusion was then started to reach a preset target brain concentration (effect site concentration Ce) of 5 μg ml−1 using the Schneider model pharmacokinetic profile. After drop of the BIS level below 60, the peripheral nerve stimulator was turned on and cisatracurium 0.15 mg kg−1 was injected IV to facilitate endotracheal intubation. After intubation, lungs were ventilated using 50% oxygen in air mixture with a tidal volume of 4–6 ml kg−1 and a respiratory rate adjusted to maintain PETCO2 between 30 and 35 mmHg with PEEP of 5 mmHg. An esophageal Doppler probe (CardioQTM/CardioQ-ODMTM, Deltex Medical Ltd., Chichester, Sussex, UK) was then inserted through the patient’s mouth after applying a water-based lubricant (35–40 cm from the incisor teeth) and positioned in order to get the best flow signal (hearing the sharpest sound with the highest peak and correct waveform amplification) with an ideal aortic waveform (sharp well defined outline with a predominantly black center). This was defined as the onset of the study. The Ce concentration of propofol was adjusted between 3.5 and 5 μg ml−1 during anesthesia maintenance to ensure a BIS level between 40 and 55. Supplemental dosages of fentanyl 1 μg kg−1 were given when mean blood pressure (MBP) or heart rate (HR) increased more than 20% of baseline readings while BIS level was still between 40 and 55. Cisatracurium (0.025 mg kg−1) was given once the first twitch in the TOF (T1) recovered to 25% of its baseline height. During laparoscopic surgery, pneumoperitoneum at 14 mmHg was performed through four-trocar ports and patients were placed at 30° reverse Trendelenburg position. Intraoperative intravenous fluid management consisted of warmed Ringer solution infused at a rate of 4–6 ml kg−1 h−1. No colloid or blood transfusion was used. Propofol infusion was discontinued by the end of skin closure. Residual neuromuscular blockade after surgery was antagonized by IV 0.05 mg kg−1 neostigmine and 0.02 mg kg−1 atropine. Multimodal analgesia in the form of paracetamol 15 mg kg−1 IV, started at the beginning of skin closure, and meperidine HCl 1 mg kg−1 IV, titrated as 10 mg increments, were both used for postoperative pain control.
.1 Hemodynamic measurements
Heart rate (HR) (beat min−1) and mean arterial pressure (MAP) (mmHg), flow time corrected (FTc) (msec), peak velocity (PV) (cm sec−1), stroke distance (SD) (cm), mean acceleration (MA) (cm sec−2), minute distance (MD) (cm), stroke volume (SV) (ml), cardiac output (CO) (l min−1), systemic vascular resistance (SVR) (dynes sec−1 cm–5) were recorded in the following timings in both groups: T0: onset of the study, T1: After insufflation (group LS) or skin incision (group OS), T2: Head-up position, T3: after 5 min, T4: after 15 min, T5: after 30 min, T6: end of operation. The peak velocity is calculated from the height of the waveform while its upstroke gives us the mean acceleration. These parameters are used by ODM for computing the remaining indices mainly stroke volume, cardiac output and systemic vascular resistance.
.2 Laboratory measurements
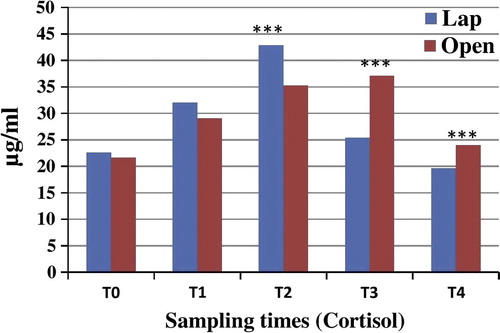
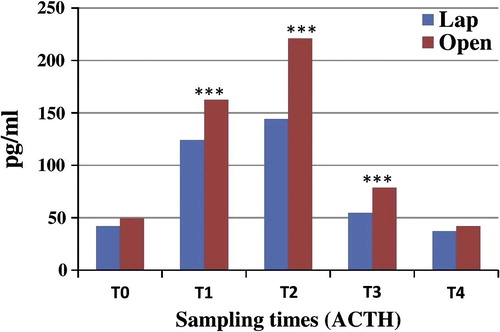
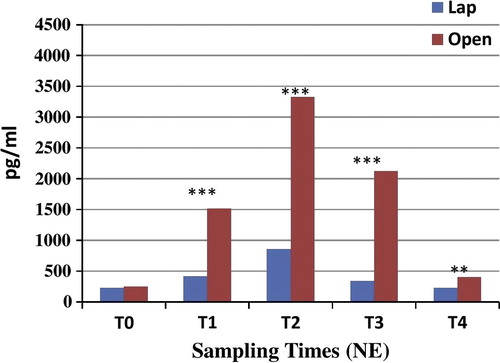
Five venous blood samples were collected peripherally at the following intervals in both groups: T0: before induction of anesthesia; T1: 30 min after the beginning of operation; T2: at the end of surgery and after deflation of the abdomen; T3: two hours after the end of surgery; T4: four hours after the end of surgery. The following stress hormones were estimated in the samples: epinephrine, norepinephrine, ACTH and cortisol.
Statistical analysis
Results are expressed as mean ± S.D. or number (%). Comparison between the two groups was performed using Kruskal–Wallis test. Comparison relative to baseline within the same group was performed using Wilcoxon sign rank test. Comparison between categorical data was performed using Chi square test. Correlation between different parameters was performed using Spearman correlation. The data were considered significant when the p value was ⩽0.05. Statistical analysis was done using the SPSS computer program (version 12 windows).
Results
Demographic data showed no statistical difference between the two groups as regards age, sex, weight and height, thus being comparable ().
able 1 Demographic features of the two studied groups.
Cardiac output measurements didn’t show statistical significant differences between the two groups at various timings. Within the laparoscopic group, there was a statistical significant increase in CO five minutes after initiation of abdominal insufflation (T3) (p < 0.05) and a rebound rise after the end of surgery (T6) (p < 0.01), a finding not present in the open surgery group (). Similarly, the stroke volume did not show any statistical significant difference between the two groups although there was a similar rebound significant rise in the laparoscopic group after the end of surgery (T6) as compared to the reading of the onset of the study (T0) (p < 0.05) (). There was a statistical significant decrease in the mean blood pressure in the two groups after insufflation in the laparoscopic group (T1) or skin incision in the open surgery group (T1) as well as after 15 min (T3) as compared to the reading of the onset of the study (T0). The mean blood pressure also showed a significant rise at T1 in the open surgery group as compared to the laparoscopic group (p = 0.049) (). The laparoscopic group showed a statistical significant decrease in SVR starting from insufflation till the end of surgery, while the open group showed statistical significance decrease only with skin incision (T1), while there was no statistically significant difference between the two groups in all timings (). Results showed no significant difference between both groups or within group as regards the stroke distance (). The minute distance showed a highly significant increase after the end of surgery (T6) in the laparoscopic group as compared to the onset of the study (T0) as well as compared to the open surgery group at the same timing (p = 0.049) (). There was no statistical significant difference in the mean acceleration in the two groups although the measurement 15 min after insufflation in the laparoscopic group (T4) showed potential significance (). The flow time corrected reading was significantly higher in the laparoscopic group after the end of surgery as compared to the open surgery group (T6) (p = 0.001) (). The heart rate was significantly decreased 15 min after surgical incision till the end of surgery in the open surgery group while the laparoscopic group showed significant decrease only after the end of surgery (T6) ().
able 2 Comparison between mean values of cardiac output (CO) (l min−1) measured at various timings of anesthesia in the two studied groups.
able 3 Comparison between mean values of stroke volume (SV) (ml) measured at various timings of anesthesia in the two studied groups.
able 4 Comparison between mean values of mean arterial blood pressure (MAP) (mmHg) measured at various timings of anesthesia in the two studied groups.
able 5 Comparison between mean values of systemic vascular resistance (SVR) (dynes sec−1 cm−5) measured at various timings of anesthesia in the two studied groups.
able 6 Comparison between mean values of stroke distance (cm) measured at various timings of anesthesia in the two studied groups.
able 7 Comparison between mean values of minute distance (cm) measured at various timings of anesthesia in the two studied groups.
able 8 Comparison between mean values of mean acceleration (cm sec−2) measured at various timings of anesthesia in the two studied groups.
able 9 Comparison between mean values of flow time corrected (msec) measured at various timings of anesthesia in the two studied groups.
able 10 Comparison between mean values of heart rate (beat min−1) measured at various timings of anesthesia in the two studied groups.
As regards the stress hormones, norepinephrine level showed a statistical significance rise throughout the period of surgery reaching its maximum 30 min after the beginning of surgery (p < 0.001) and sloping down gradually till four hours after the end of surgery although still highly significant. These changes were very clear in the open surgery group and did not show any significance in the laparoscopic group (). As with norepinephrine levels, epinephrine levels showed a similar trend but reaching its maximum two hours after surgery (p < 0.001) and dropping down afterward in the open surgery group. No similar changes were detected in the laparoscopic group (). The cortisol level was significantly elevated at T2 (30 min after the beginning of surgery) in the laparoscopic group while the open surgery group showed a significant rise after the end of surgery at T3 and T4 (p < 0.001) (). ACTH levels significantly increased at T1, T2 and T3 in the open surgery group (p < 0.001) returning back to the preoperative levels four hours after surgery in the open surgery group. The laparoscopic group did not show any statistical significant change ().

Discussion
BIS-guided total intravenous anesthesia is currently a new tool added to the armamentarium of the anesthesiologist to obviate the use of volatile anesthetics. Propofol with its unique characteristics as a short acting non-cumulative agent proved to be the ideal drug for this technique. Laparoscopic cholecystectomy with the hazards of pneumoperitoneum, and open cholecystectomy with its stress response both need a revision of the anesthetic technique for intraoperative optimization of their outcome. Hemodynamic changes during the procedure require also a thorough close monitoring offered ideally by the esophageal Doppler monitor as well as the measurement of the stress hormones since these changes are both neuro-humoral and mechanically mediated.
Hemodynamic disturbances in laparoscopic procedures are mainly due to pneumoperitoneum. When intra-abdominal pressure (IAP) reaches above 10 mmHg, hemodynamic disturbances are clinically significant, while above 15 mmHg, abdominal compartment syndrome can occur affecting multiple organ systems. The following equation can emphasize many cardiovascular manifestations
Pneumoperitoneum increases SVR and decreases CO but MAP usually increases since the increase in SVR surpasses the decrease in CO. These changes are relative to the rise in IAP. The increase in SVR is due to abdominal organs and vessels compression as well as difficulty to the flow through arterial beds caused by neurohumoral and mechanical components.
The drop in CO can be due to decreased venous return from compressed inferior vena cava, increased resistance in the venous circulation, hypovolemia from bowel preparation or the type of anesthesia used. The head up (reverse Trendelenburg) position reduces even more the venous return. CO typically decreases 10–30% [Citation10]. Thus, intraoperative cardiac function is affected by many factors such as preload, afterload, contractility, heart rate, type of anesthesia, positioning and myocardial compliance [Citation11]. Hypercapnia is known to affect the autonomic nervous system causing tachycardia, increased myocardial contractility and CO [Citation12]. Hirvonen and his colleagues showed that the reverse Trendelenburg position exaggerates the pneumoperitoneum-related decrease in venous return as well as cardiac preload and cardiac index [Citation13].
In the current study, cardiac output measurements didn’t show any statistical significant difference between the two groups at various timings even after head up position. Within the laparoscopic group, there was a statistical significant increase in CO 5 min after initiation of abdominal insufflation and a rebound rise after the end of surgery (T6), and this finding was not observed in open surgery group. This goes in accordance with the findings of Zhang and his colleagues who found that CO increases at IAP of 7.5 mmHg, normalizes at 15 mmHg and decreases at pressures around 30 mmHg. Thus, the rise of IAP does not always obviate a drop in CO [Citation14]. Our stable intraoperative hemodynamics are further supported by the study of Gu and his colleagues in children with ASA physical status I–II scheduled for laparoscopic procedures [Citation15]. The increase in CO after abdominal insufflation in laparoscopic group may be partially due to the hypercarbia as well as the absence of inhalational anesthetic negative inotropic effect. The BIS-guided target-infused propofol probably offered better hemodynamic control in this study through optimization of serum level of propofol thus minimizing its side effects. This goes in accordance with a study held in 2010 which concluded that during laparoscopic surgery with patients in the head-up position, TIVA technique may improve cardiac autonomic control by enhancing protective parasympathetic activity [Citation16]. After reverse Trendelenburg positioning CO decreased in this study. Bakri and El-Tablawy showed that this positioning may not be a major factor affecting intraoperative CO, thus the difference in anesthesia technique may contribute to these changes as patients in their study were maintained using isoflurane inhalational anesthesia while we used TIVA BIS-guided target-infused propofol [Citation17]. As the CO didn’t decrease, the stroke volume also did not show any significant decline, but, there was a similar rebound significant rise of both the CO and stroke volume in the laparoscopic group after the end of surgery (T6) compared to the reading at the onset of the study, and this may be due to the relief of the insufflation and increase in the venous return at the end of the procedure. Regarding arterial blood pressure, there was a statistical significant decrease in the mean arterial pressure in both groups: after insufflation in the laparoscopic group (T1), or skin incision in open surgery group (T1) and after 15 min (T3) compared to the reading at the onset of the study (T0). The laparoscopic group showed a statistical significant decrease in SVR throughout the whole procedure. SVR decreased only with skin incision in the open group. Similar to our results, Danzig and his colleagues showed an elevation of the mean arterial blood pressure with no change in the time course of SVR. Yet, they reported also many contradictions as a significant tendency for hypotension and bradycardia caused by the chronic use of cardiac medications (β-blockers and ACE inhibitors) acting against the tendency of blood pressure elevation after peritoneal insufflation. It is to be noted that their patients suffered from ischemic heart disease or aortic stenosis [Citation18]. In a case discussion held by Jones and his colleagues showing effect of laparoscopic cholecystectomy in a cardiac transplant patient with ejection fraction 15%, contrarily to our result there was a rise in MAP and SVR with insufflation of 10 mmHg with a minimal decline in CO. These differences may be due to the previous cardiac status of the patient and the anesthetic technique used [Citation19]. In the current study, the laparoscopic group showed a statistical significant decrease in SVR starting from insufflation till the end of surgery, while the open group showed statistical significance decrease only with skin incision (T1), and there was no statistically significant difference between the two groups in all timings. These results go in accordance with Deryck and his colleagues who found that propofol better maintained arterial pressure, increased arterial compliance and optimized the coordination between the left ventricle and the arterial vascular bed as compared to isoflurane [Citation20]. Regarding the surgical technique, it is known that increased IAP during laparoscopy induces circulatory changes due to redistribution of abdominal venous blood toward the thoracic cavity resulting in an increase in SV, CO, and MAP. Concurrently, on the arterial side, this increase in IAP causes a rise in MAP and SVR, potentially causing a decrease in both SV and CO. These effects are variable according to the level of IAP and the patient’s preload status which may explain the discrepancies in results between various studies [Citation21–Citation23,Citation4]. Contrary to our results, Joris and his colleagues demonstrated that at an IAP of 14 mmHg during laparoscopic cholecystectomy in healthy patients there was major hemodynamic changes such as an increase in MAP and SVR, and an almost 50% decrease in cardiac Index (CI). Increased venous resistance [Citation24] and compression of the abdominal aorta contributed to the increase in cardiac afterload [Citation25–Citation27]. These changes may be attributed to the difference in anesthetic technique used in these patients as well as the difference in monitoring facilities as our usage of propofol, BIS and non-invasive esophageal Doppler as opposed to invasive Swan-Ganz catheter.
Morbidity and mortality of patients undergoing surgical procedures depend not only on intraoperative complications, but also on the severity of the surgical wound which determines the body’s stress response [Citation28,Citation29]. The systemic response to surgical injury is complex involving psychological, physical stress, neuroendocrine and inflammatory mediators. In humans, there is anticipatory stress that is associated with elevations of cortisol and catecholamines on the day of surgery. The anesthetic management as well as the type of ventilation strategy and analgesia received has also been related to the level of surgical stress in such patients [Citation30]. Serum cortisol increases after acute stress. Its level indicates the degree of stimulation of the hypothalamic–pituitary–adrenal axis. Cortisol acts either directly or indirectly on different homeostatic mechanisms of body to attenuate the stress [Citation31]. In the current study, cortisol level was significantly elevated 30 min after the beginning of surgery in the laparoscopic group, while the open surgery group showed a significant rise after the end of surgery at T3 and T4. These results go in accordance with Zea and his colleagues who showed that in open cholecystectomy group the rise of serum cortisol was significant 6 h after the operation when compared to the laparoscopic group which fell after 48 h. However, at both intervals of time, 6 h and 48 h, the serum cortisol level was significantly higher in the open group [Citation32]. A study held by Krikri and his colleagues on male pigs showed that plasma adrenaline and noradrenaline concentrations were significantly lower during laparoscopic cholecystectomies and adrenalectomies than the open surgeries. These results meet ours although it is an experimental animal study with different anesthetic techniques [Citation33]. Our results showed that norepinephrine and epinephrine levels have a similar increase reaching their maximum 2-h after surgery and dropping down afterward in open surgery group. No similar changes were detected in the laparoscopic group. These results don’t meet Donald and his colleagues who compared the responses of the stress hormones to elective conventional and laparoscopic cholecystectomy and found that adrenaline did not significantly decrease by the laparoscopic approach, but there was a significant increase in the noradrenaline response. This difference in results may be due to the difference in anesthetic technique as their patients received fentanyl, thiopentone and vecuronium and maintained by [Citation34]. Some authors have argued that the trauma of laparoscopic cholecystectomy, although lacking the long incision in the abdominal wall, is ultimately not smaller than that of open surgery and thus the body’s response is practically the same. They have suggested that the tissue trauma in the form of intraperitoneal manipulations pulling of the gall bladder and mesentery are similar in both methods and the pneumoperitoneum is an aggravating factor on the surgical wound [Citation35,Citation36]. Calvo-Soto and his colleagues compared the stress response to laparoscopic cholecystectomy during spinal-general anesthesia and epidural-general anesthesia. They found that noradrenaline, adrenaline and total catecholamines that were measured pre- and intra-operatively were lower when compared to preoperative levels but they were significantly lower in the spinal-general group compared with the epidural-general group. They used different anesthetics and maintained it with sevoflurane. This may indicate a role of general anesthesia effect on stress hormones [Citation37].
Conclusions
In conclusion, this study suggests that BIS-guided TCI anesthesia using propofol-fentanyl offers a good and safe anesthesia method for patients undergoing either laparoscopic or open cholecystectomy. The hemodynamic stability offered by this technique makes it a very appealing choice. Thorough hemodynamic monitoring using the esophageal Doppler monitor tailors the drug administration in the safe limits and would probably offer an excellent guide in critically patients to its easiness in use and extensive real-time data acquisition. We must reiterate that our results should be considered in the context of this trial since our population was of a limited number and did not suffer from any chronic disease.
Conflict of interest
The authors declare that there are no conflicts of interest.
Acknowledgments
The authors gratefully appreciate the work of Dr. Hoda Abou Taleb and Dr. Tarek Diab, Professor in Theodor Bilharz Research Institute for their statistical assistance.
This study was supported by a full grant for the internal project department, Theodor Bilharz Research Institute and was registered as “project 87T” without any impact on the study design, collection, analysis and interpretation of data.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- R.W.WahbaF.BeiqueS.J.KleimanCardiopulmonary function and laparoscopic cholecystectomyCan J Anaesth42119955163
- S.Odeberg-WernermanA.SolleviCardiopulmonary aspects of laparoscopic surgeryCurr Opi Anesthesiol91996529535
- M.J.ColominaC.GodetF.PelliséJ.BagóC.VillanuevaTranscranial Doppler monitoring during laparoscopic anterior lumbar interbody fusionAnesth Analg976200316751679
- P.AlfonsiA.Vieillard-BaronM.CoggiaB.GuignardO.Goeau-BrissonniereF.JardinCardiac function during intraperitoneal CO2 insufflation for aortic surgery: a transesophageal echocardiographic studyAnesth Analg1025200613041310
- E.J.HaxbyM.R.GrayC.RodriguezD.NottM.SpringallM.MythenAssessment of cardiovascular changes during laparoscopic hernia repair using oesophageal DopplerBr J Anaesth7851997515519
- C.W.HogueJrT.A.BowdleC.O’LearyD.DuncalfR.MiguelM.PittsA multicenter evaluation of total intravenous anesthesia with remifentanil and propofol for elective inpatient surgeryAnesth Analg8321996279285
- F.GuarracinoF.LapollaC.CarielloA.DanellaL.DoroniR.BaldassarriTarget controlled infusion: TCIMinerva Anestesiol7162005335337
- M.SingerEsophageal Doppler monitoring of aortic blood flow: beat-by-beat cardiac output monitoringInt Anesthesiol Clin313199399125
- H.G.WakelingM.R.McFallC.S.JenkinsW.G.WoodsW.F.MilesG.R.BarclayIntraoperative oesophageal Doppler guided fluid management shortens postoperative hospital stay after major bowel surgeryBr J Anaesth9552005634642
- C.O’MalleyA.J.CunninghamPhysiologic changes during laparoscopyAnesthesiol Clin North America1912001119
- N.T.NguyenH.S.HoN.W.FlemingP.MooreS.J.LeeC.D.GoldmanCardiac function during laparoscopic vs open gastric bypassSurg Endosc16120027883
- K.C.SharmaR.D.BrandstetterJ.M.BrensilverL.D.JungCardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgeryChest11031996810815
- E.A.HirvonenE.O.PoikolainenM.E.PääkkönenL.S.NuutinenThe adverse hemodynamic effects of anesthesia head-up tilt and carbon dioxide pneumoperitoneum during laparoscopic cholecystectomySurg Endosc1432000272277
- Q.M.ZhangY.W.ChenD.W.HouY.R.ChenInfluence of laparoscopic surgery on cardiac function (an animal study)Chin J Ped Surg222001138140
- H.GuJ.LiuC.WuImpact of dexmedetomidine versus propofol on cardiac function of children undergoing laparoscopic surgeryInt J Clin Exp Med712201458825885
- C.Di IorioT.CafieroR.M.Di MinnoThe effects of pneumoperitoneum and head-up position on heart rate variability and QT interval dispersion during laparoscopic cholecystectomyMinerva Anestesiol76112010882889
- M.BakriM.El-TablawyHemodynamics respiratory and stress responses in morbidly obese versus non-obese patients during laparoscopic cholecystectomyAl-azhar Assiut Med J532007172185
- V.DanzigZ.KrskaR.DemesZ.DanzigováA.LinhartO.KittnarHemodynamic response to laparoscopic cholecystectomy – impacts of increased afterload and ischemic dysfunction of the left ventriclePhysiol Res5442005377385
- P.E.JonesS.C.SaysonD.C.KoehlerLaparoscopic cholecystectomy in a cardiac transplant candidate with an ejection fraction of less than 15%JSLS2119988992
- Y.L.DeryckS.BrimioulleM.MaggioriniD.de CanniereR.NaeijeSystemic vascular effects of isoflurane versus propofol anesthesia in dogsAnesth Analg8351996958964
- J.L.JorisD.P.NoirotM.J.LegrandN.J.JacquetM.L.LamyHemodynamic changes during laparoscopic cholecystectomyAnesth Analg65199310671071
- S.N.HarrisG.H.BallantyneM.A.LutherA.C.PerrinoJr.Alterations of cardiovascular performance during laparoscopic colectomy: a combined hemodynamic and echocardiographic analysisAnesth Analg8331996482487
- E.VivierO.MettonV.PiriouF.LhuillierJ.M.Cottet-EmardP.BrancheEffects of increased intra-abdominal pressure on central circulationBr J Anaesth9662006701707
- A.C.GuytonTextbook of medical physiology11th ed.2006WB Saunders Co.Philadelphia
- G.JJohannsenM.AndersenB.JuhlThe effect of general anaesthesia on the haemodynamic events during laparoscopy with CO2-insufflationActa Anaesthesiol Scand3321989132136
- R.TorrielliM.CesariniS.WinnockC.CabiroJ.M.MeneHemodynamic changes during celioscopy: a study carried out using thoracic electric bioimpedanceCan J Anaesth37119904651
- A.FalabellaE.Moore-JeffriesM.J.SullivanR.NelsonM.LewCardiac function during steep Trendelenburg position and CO2 pneumoperitoneum for robotic-assisted prostatectomy: a trans-oesophageal Doppler probe studyInt J Med Robot342007312315
- R.G.DouglasJ.H.ShawMetabolic response to sepsis and traumaBr J Surg7621989115122
- D.S.GannJ.F.AmeralEndocrine and metabolic responses to injury5th ed.S.SchwarzG.ShiresF.SpencerPrinciples of surgeryvol. 11989Mc Graw-Hill Book Company169
- D.W.WilmoreFrom Cuthbertson to fast-track surgery: 70 years of progress in reducing stress in surgical patientsAnn Surg23652002643648
- D.R.DerbyshireG.SmithSympathoadrenal responses to anaesthesia and surgeryBr J Anaesth5671984725739
- M.ZeaA.AneesN.IslamK.ZafarT.AshrafComparison of metabolic and inflammatory stress response after laparoscopic and open cholecystectomyInternet J Surg22220091
- A.KrikriV.AlexopoulosE.ZoumakisP.KatsaronisE.BalafasG.KouraklisLaparoscopic vs. open abdominal surgery in male pigs: marked differences in cortisol and catecholamine response depending on the size of surgical incisionHormones (Athens)1222013283291
- R.A.DonaldE.G.PerryG.A.WittertM.ChapmanJ.H.LiveseyM.J.EllisThe plasma ACTH AVP CRH and catecholamine responses to conventional and laparoscopic cholecystectomyClin Endocrinol (Oxf)3861993609615
- A.MilheiroF.C.SousaE.C.MansoF.LeitãoMetabolic responses to cholecystectomy: open vs. laparoscopic approachJ Laparoendosc Surg451994311317
- G.M.CooperA.M.ScogginsI.D.WardD.MurphyLaparoscopy – a stressful procedureAnaesthesia3731982266269
- P.Calvo-SotoA.Martíanez-ContrerasB.Trujillo-HernándezF.J.Peraza-GarayC.VasquezSpinal-general anaesthesia decreases neuroendocrine stress response in laparoscopic cholecystectomyJ Int Med Res4022012657665