Abstract
Background
Laparoscopic surgical procedures have various benefits to the patient in terms of decreased tissue damage, early ambulation, decreased hospital stay and reduced analgesic needs. Pneumoperitoneum with carbon dioxide (CO2) leads to stimulation of the sympathetic nervous system which can be a risk factor in patients with cardiovascular diseases. Moreover, reverse Trendelenburg position affects homeostasis in laparoscopic surgeries. In this study, we compared the efficacy of clonidine (which is α2 adrenergic agonist) versus esmolol (which is ultra short acting cardio-selective β1-receptor antagonist) on the hemodynamic response during laparoscopic cholecystectomy.
Materials and methods
A total of 60 patients scheduled to undergo laparoscopic cholecystectomy were randomly assigned into two groups: Group C: received 2 μg/kg of clonidine diluted in 20 ml normal saline, given with slow intravenous infusion over 10 min just before induction of GA and Group E: received 1.5 mg/kg of esmolol as a loading dose over a period of 5 min just before induction of GA followed by 10 μg/kg/min as a maintenance dose throughout the procedure. No hypnotic medication was given on the evening before surgery. Systolic, diastolic, mean arterial blood pressures and heart rate were recorded at (1) baseline, (2) three minutes after endotracheal intubation, (3) before pneumoperitoneum, (4) fifteen minutes after pneumoperitoneum, (5) thirty minutes after pneumoperitoneum, (6) five minutes after release of CO2 and (7) five minutes after extubation. Degree of sedation according to Ramsay sedation score was assessed 15 min after reaching PACU.
Results
Both groups were similar with respect to demographic data. Clonidine group showed more stability in hemodynamic responses than esmolol group in all hemodynamic variables but with more postoperative sedation.
Conclusion
This study concluded that clonidine and esmolol provide hemodynamic stability in laparoscopic cholecystectomy but clonidine provides more stability with postoperative sedation.
Introduction
Laparoscopy has now become the standard technique of choice for cholecystectomy. Laparoscopic surgical procedures have various benefits to the patient in terms of decreased tissue damage, early ambulation, decreased hospital stay and reduced analgesic needs. The hallmark of laparoscopy is the creation of pneumoperitoneum with carbon dioxide (CO2) which leads to stimulation of the sympathetic nervous system resulting in pathophysiological changes characterized by increase in arterial pressure and systemic and pulmonary vascular resistance (SVR and PVR) early after the beginning of intra-abdominal insufflation with little change in heart rate (HR) which can be a risk factor for adverse cardiologic events in patients with pre-existing essential hypertension, ischemic cardiac disease, or increased intra-cranial or intra-ocular pressure [Citation1–Citation4]. Moreover, there is a significant change in the homeostasis observed in reverse Trendelenburg position used for laparoscopic surgeries. In addition, the anesthetic agents put together alter the cardiopulmonary function significantly [Citation5].
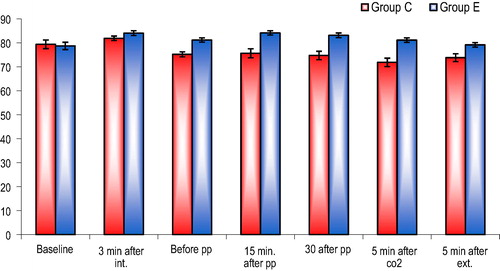
able 3 Changes in diastolic arterial pressure.
Different pharmacological agents such as α2 adrenergic agonists, magnesium sulfate [Citation6], beta-blockers [Citation7] and opioids [Citation8] are used to attenuate circulatory response due to pneumoperitoneum. Clonidine is a selective α2 adrenergic agonist which causes fall in blood pressure and heart rate (HR) with decreased SVR and cardiac output [Citation9]. Esmolol, an ultra short-acting cardio-selective β1-receptor antagonist, has been shown to blunt hemodynamic responses to perioperative noxious stimuli [Citation10]. Hence, the present randomized study was designed to evaluate and compare the efficacy of clonidine versus esmolol on hemodynamic response during laparoscopic cholecystectomy. In other words, the rationale of the study was to reach laparoscopic cholecystectomy with stable hemodynamics.
Materials and methods
This was a randomized, double blind, comparative clinical study performed in Ain shams University Hospitals from November 2014 till May 2015. After getting approval from the institutional ethical committee, an informed consent was taken from every patient enrolled in the study.
Sixty patients aged ⩾20–⩽60 years, ASA physical status I or II, planned for elective laparoscopic cholecystectomy were included. The exclusion criteria included the following: ASA physical status > 2, taking beta-blocking drugs or sedatives or antihypertensives or antipsychotics or analgesics, inability to communicate with the patient due to any reason, patients with neurologic, cardiovascular, renal, hepatic diseases or diabetes mellitus, pregnant or breast-feeding females, duration of procedure lasting for more than 120 min and anticipated difficult airway.
.1 Method of randomization
Patients were allocated randomly by a computer generated list of random permutations to one of two equal groups (30 patients each): group C and group E.
| #x2013; | Group C: Received 2 μg/kg of clonidine diluted in 20 ml normal saline, given with slow intravenous infusion over 10 min just before induction of GA. | ||||
| #x2013; | Group E: Received 1.5 mg/kg of esmolol as a loading dose over a period of 5 min just before induction of GA followed by 10 μg/kg/min as a maintenance dose throughout the procedure. | ||||
Randomization sequence was concealed in sealed envelopes performed by the help of an independent personnel. An appropriate code number was assigned to each patient, with an allocation ratio of 1:1. The study solutions were prepared and injected by an attending anesthesiologist who was not involved in the patient care or data collection. All patients, investigators and anesthesiologists were blinded to the infusion administered. Drug administration and data collection were carried out by investigators in a double-blind manner.
No hypnotic medication was given on the evening before surgery. Patients were premedicated with glycopyrrolate 0.02 mg/kg i.v. and ondansetron 4 mg i.v. in the preoperative room. Upon arrival in the operating room, monitors were attached to the patients and baseline parameters (heart rate, NIBP, oxygen saturation, temperature and end tidal CO2, and ECG) were recorded.
After pre-oxygenation with O2 100% for 3 min, anesthesia was induced with a standard anesthetic protocol using midazolam 0.03 mg/kg, fentanyl 1 μg/kg, thiopentone sodium 3–5 mg/kg, and tracheal intubation was facilitated by atracurium 0.5 mg/kg intravenously. Lungs were mechanically ventilated with O2 50% and anesthesia was maintained with isoflurane 0.8% and atracurium 0.1 mg/kg every 25 min. Ventilation was adjusted to maintain normocapnia (end-tidal carbon dioxide [EtCO2] 40 ± 5 mmHg). Pneumoperitoneum was created by insufflations of CO2 and operation table was tilted to about 15° reverse Trendelenberg. Intra-abdominal pressure was not allowed to exceed more than 14 mmHg. After 1 h of surgery, each patient received 1 g paracetamol infused over 30 min intravenously. During surgery, Ringer’s lactate solution was administered in maintenance dose as per Holliday-Segar formula. Any hypotension (MAP < 20% preoperative) was managed with a fluid bolus of normal saline 250–300 ml. If hypotension did not respond to fluid administration, then ephedrine 15 mg i.v. was ready to be administered. Any incidence of bradycardia (HR < 50/min) was treated with atropine 0.7 mg i.v.
At the end of surgery, residual neuromuscular block was reversed by the injection of neostigmine 0.05 mg/kg and glycopyrrolate 0.02 mg/kg i.v. and patient was extubated when respiration was sufficient, and they were able to obey commands. Esmolol infusion was stopped 5 min after extubation. Patients were transferred to the postanesthesia care unit (PACU) where they were monitored for any evidence of complications or adverse events. Systolic, diastolic, mean arterial blood pressures and heart rate were recorded at the following points of time:
(1) Prior to induction before receiving clonidine or esmolol (baseline).
(2) Three minutes after endotracheal intubation.
(3) Before pneumoperitoneum.
(4) Fifteen minutes after pneumoperitoneum.
(5) Thirty minutes after pneumoperitoneum.
(6) Five minutes after release of CO2.
(7) Five minutes after extubation.
Degree of sedation according to Ramsay sedation score was assessed 15 min after reaching PACU. Level of sedation score was as follows: 0 Awake and agitated 1 Awake and comfortable 2 Asleep and arousable 3 Asleep with sluggish response to verbal commands or touch 4 No response to verbal command or touch. The results obtained in the study are presented in tabulated manner.
The primary outcomes of our study were as follows: systolic blood pressure, diastolic blood pressure, mean blood pressure and heart rate. The secondary outcomes were as follows: postoperative sedation and any possible side effects of the 2 drugs.
.2 Statistics
Statistical presentation and analysis of the present study were conducted, using the mean, standard deviation, Chi-square, paired t-test and unpaired t-test by SPSS V17. Unpaired Student T-test was used to compare between related samples. Fisher’s exact test and Yates’ corrected chi-square are computed for 2 × 2 tables.
.3 Sample size
The sample size was calculated using Epicalc 2000 software depending on the results from previous studies [Citation6,Citation7] with the following parameters:
Type I error (α) = 5% with confidence level 95% and power of study 90% (power of test) with type error II 10% (Beta) with expected difference of 0.36. The minimal sample size was 28 in each group. A total of 30 patients in each group were included to compensate for possible dropouts. Corresponding P was computed. P < 0.05 was considered as statistically significant.
Results
There were no significant differences between the two groups with regard to demographic data such as age, sex, weight and ASA grade ().
able 1 Demographic data.
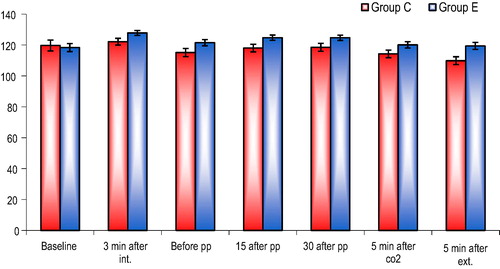
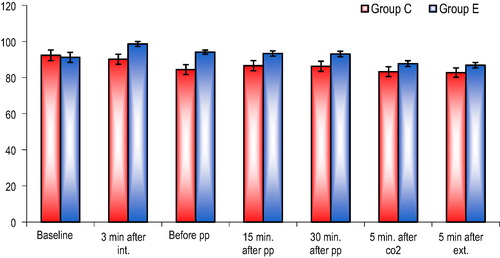
Preoperative vital data before induction (SBP, DBP, MBP and HR) were compared between the two groups of patients and no significant difference was found (baseline values of –). Systolic arterial pressure, diastolic blood pressure and mean blood pressure increased slightly after intubation in both groups and then decreased significantly intraoperatively and after extubation compared to baseline values but it was significantly lower in group C compared with group E (–) and (). One patient suffered from significant hypotension in group C which was managed with a fluid bolus of normal saline 300 ml and ephedrine 15 mg i.v.
able 2 Changes in systolic arterial pressure.
able 4 Changes in mean arterial pressure.
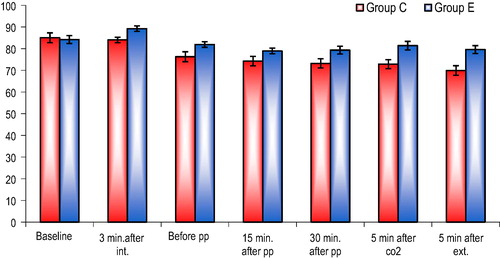
able 5 Changes in heart rate.
After intubation and till 5 min after extubation, mean HR values measured were significantly lower in group C compared to group E and in both groups the values were lower than baseline values except in group E 3 min after intubation (mean value was slightly higher than baseline value) (and ).
2 patients in group C required intravenous atropine due to bradycardia (HR < 50).
Degree of sedation according to Ramsay sedation score was assessed in patients 15 min after reaching PACU. The mean score in group C was significantly higher than the mean score in group E ().
able 6 Sedation score comparison between the two groups.
Discussion
Our study confirms that clonidine and esmolol can successfully control hemodynamic changes in laparoscopic cholecystectomy; however clonidine has stronger effects on the hemodynamics with a sedative effect.
Laparoscopic cholecystectomy is considered a minimally invasive procedure. Hemodynamic changes with pneumoperitoneum were first recognized in 1947 [Citation11]. Pneumoperitoneum using CO2 for laparoscopic surgery causes a rapid and immediate increase in plasma catecholamines and vasopressin [Citation12,Citation13] possibly due to an increase in intraperitoneal pressure and stimulation of the peritoneum by CO2. At intra-abdominal pressure of 15 mmHg, Joris et al. [Citation4] found a 35% increase in mean arterial pressure, a 65% increase in systemic vascular resistance, and a 90% increase in pulmonary vascular resistance, while there was a 20% decrease in cardiac output. Plasma concentrations of renin also increase during laparoscopy [Citation14]. The increase in catecholamines, renin and vasopressin induces a cardiovascular response characterized by abrupt elevations of arterial pressure, SVR and HR [Citation15]. The increase in these hemodynamic values significantly increases the incidence of myocardial ischemia, infarction and other complications [Citation16]. Various techniques such as gasless approach and many pharmacological agents have been used to counteract these detrimental effects of pneumoperitoneum. On the other hand, laryngoscopic stimulation of oropharyngeal structures may be an important factor in hemodynamic stress response associated with tracheal intubation [Citation17]. Instrumentation of the pharynx and tracheal intubation may result in tachycardia, hypertension and increased catecholamine concentration that may evoke life threatening condition among susceptible individuals especially those with cardiovascular disease [Citation18]. Also it may lead to occasional arrythmias, cough reflexes, increased intracranial pressure, and increased intraocular pressure. If no specific measures are taken to prevent the hemodynamic response, the HR can increase from 26% to 66% depending on the method of induction, and SBP can increase from 36% to 45% [Citation19].
Our study compared between clonidine and esmolol because both of these drugs antagonize such hemodynamic changes during laparoscopy surgeries. Clonidine, a selective α-2 adrenergic agonist, has desirable actions such as anxiolysis, sedation, analgesia, antiemesis, and prevention of shivering. It is a potent hypotensive agent. Clonidine inhibits catecholamine and vasopressin-mediated increase in SVR caused by pneumoperitoneum [Citation20]. Numerous studies using intravenous clonidine found effective prevention of hemodynamic derangements because of intubation and during laparoscopic cholecystectomy [Citation21,Citation22]. However, higher doses of clonidine resulted in significant bradycardia and hypotension [Citation23]. Malek et al. [Citation24] used 150 μg of clonidine as intravenous infusion while Sung et al. [Citation25] and Yu et al. [Citation26] used 150 μg of oral clonidine as premedication for maintenance of hemodynamic stability during pneumoperitoneum. Yu et al. even recommended its routine use as premedication in laparoscopic surgeries. Das et al. [Citation27] also used 150 μg of oral clonidine 90 min prior to surgery to prevent hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy. Kalra et al. [Citation28] used clonidine 1 μg/kg intravenously over a period of 15 min before pneumoperitoneum and clonidine group patients showed significantly better hemodynamic control than control group.
β-adrenergic receptor antagonists have also been used by various authors during surgery with the intention to attenuate the stress response of intubation and decrease the unwanted perioperative hemodynamic changes [Citation29]. Esmolol is the selective β-adrenergic receptor blocker available and with its rapid onset and extremely short duration of action, would appear to be an ideal drug for preventing acute increases in HR and SAP [Citation30].
As an optimal intravenous (IV) esmolol dose for use during anesthesia induction (laryngoscopy and intubation) and emergence (extubation) has been previously determined in some studies to be 1.5 mg/kg, we used the same bolus dose in our study [Citation31,Citation32]. Moreover, many studies have demonstrated that beta adrenergic blockers that exert depressive effects on the central nervous system as esmolol also decreases the need for intraoperative anesthetic agents, leading to rapid recovery from anesthesia [Citation31,Citation33,Citation34].
In this study, we compared between clonidine and esmolol in reduction of stress response and hemodynamic changes associated with laparoscopy. Both groups showed attenuation in SBP, DBP, MBP and HR increases in response to intubation with group C showing little increases compared to group E which was statistically significant. It was found that the SBP, DBP, and MBP values were lower with clonidine group compared to baseline values during pneumoperitoneum, release of CO2 and after extubation than esmolol group and it was statistically significant. Just one patient in clonidine group suffered from significant hypotension but it was managed rapidly with fluids and ephedrine. Generally, the fluctuations in blood pressure during such operation were attenuated in both groups; therefore, we can safely conclude that clonidine and esmolol stabilize blood pressure during various phases of anesthesia and laparoscopy. After intubation, esmolol group showed little increase in mean heart rate compared to baseline value while in clonidine group, mean heart rate was lower than baseline value. However, the heart rate was lower in both groups during the surgery as compared to baseline values and it was statistically significant. Moreover, the mean heart rate was lower in group C compared with group E throughout the procedure and it was statistically significant. In spite of its more pronounced effect on heart rate, just 2 patients receiving clonidine suffered from significant bradycardia and required atropine injection. None of esmolol group suffered from bradycardia. Definitely, the heart rate lowering effect of both study drugs reduces the myocardial oxygen demand of the patient which can be very useful in patients suffering from coronary artery disease. The sedative effect of clonidine was obvious postoperatively compared with esmolol group but sedation was not that deep as patients were arousable either verbally or by touch.
Conclusion
In laparoscopic cholecystectomy the use of clonidine or esmolol will provide hemodynamic stability but with a postoperative sedative effect more with clonidine.
Source of funding
No funding.
Conflict of interests
No conflict of interests.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- J.JorisAnesthetic management of laparoscopyMiller’s Anesthesia5th ed.1994Churchill LivingstoneNew York20112029
- R.W.WabhaF.BeiqueS.J.KleimanCardiopulmonary function and laparoscopic cholecystectomyCan J Anaesth4219955163
- K.C.SharmaR.D.BrandstetterJ.M.BrensilverL.D.JungCardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgeryChest1101996810815
- J.L.JorisD.P.NoirotM.J.LegrandN.J.JacquetM.L.LamyHemodynamic changes during laparoscopic cholecystectomyAnesth Analg75199310671071
- L.J.JeanAnaesthesia for laparoscopic surgeryR.D.MillerAnesthesia7th ed.2010Churchill LivingstoneNew York21852202
- N.K.KalraA.VermaA.AgarwalH.D.PandeyComparative study of intravenously administered clonidine and magnesium sulfate on hemodynamic responses during laparoscopic cholecystectomyJ Anaesthesiol Clin Pharmacol272011344348
- A.M.KoivusaloM.ScheininI.TikkanenEffects of esmolol on haemodynamic response to CO2 pneumoperitoneum for laparoscopic surgeryActa Anaesthesiol Scand421998510517
- C.LentschenerO.AxlerH.FernandezHaemodynamic changes and vasopressin release are not consistently associated with carbon dioxide pneumoperitoneum in humansActa Anaesthesiol Scand452001527535
- C.S.SungS.H.LinK.H.ChanW.K.ChangL.H.ChowT.Y.LeeEffect of oral clonidine premedication on perioperative haemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic cholecystectomyActa Anaesthesiol Sin3820002329
- P.F.WhiteB.WangJ.TangR.H.WenderR.NaruseA.SloninskyThe effect of intraoperative use of esmolol and nicardipine on recovery after ambulatory surgeryAnesth Analg976200316331638
- W.M.BookerD.M.FrenchP.A.MolanoFurther studies on the acute effects of intra abdominal pressureAm J Physiol1491947292298
- K.MyreM.RostrupT.BuanesO.StoklandPlasma catecholamines and haemodynamic changes during pneumoperitoneumActa Anaesthesiol Scand4231998343347
- C.MannG.BoccaraY.PouzeratteJ.ElietC.Serradel-Le GalC.VergnesThe relationship among carbon dioxide pneumoperitoneum, vasopressin release, and hemodynamic changesAnesth Analg8921999278283
- R.A.BaratzJ.H.KarisBlood gas studies during laparoscopy under general anesthesiaAnesthesiology301969463464
- J.F.LarsenF.M.SvendsenV.PedersenRandomized clinical trial of the effect of pneumoperitoneum on cardiac function and haemodynamics during laparoscopic cholecystectomyBr J Surg9172004848854
- J.G.McLaughlinD.E.ScheeresR.J.DeanB.W.BonnellThe adverse hemodynamic effects of laparoscopic cholecystectomySurg Endosc921995121124
- S.KiharaJ.BrimacombeY.YuguchiS.WatanabeN.TaguchiT.KumatsuzakiHaemodynamic responses among three tracheal intubation devices in normotensive and hypertensive patientsAnaesth Analg962003890895
- Kim, Woon-Young, Lee, Yoon-Sook, Ok, Se Jim, Kim, Jac-Hwan, Park, Young-Cheol, Lim, Hye-Ja. Lidocaine does not prevent bispectral index increases in response to endotracheal intubation. Anaesth Analg 2006; 102: 156–9 [International Anaesthesia Research Society].
- WylieChurchill DavidsonStress managementA practice of anesthesia7th ed.2003ArnoldLondonISBN 03407313031326
- M.P.ZalunardoA.ZollingerD.R.SpahnB.SeifertM.RadjaipourK.GautschiEffects of intravenous and oral clonidine on hemodynamic and plasma-catecholamine response due to endotracheal intubationJ Clin Anesth921997143147
- M.LaisalmiA.M.KoivusaloP.ValtaI.TikkanenL.LindgrenClonidine provides opioid-sparing effect, stable hemodynamics, and renal integrity during laparoscopic cholecystectomySurg Endosc1511200113311335
- J.MálekJ.KnorA.KurzováM.LopourováAdverse hemodynamic changes during laparoscopic cholecystectomy and their possible suppression with clonidine premedication. Comparison with intravenous and intramuscular premedicationRozhl Chir781999286291
- M.RayD.P.BhattacharjeeB.HajraR.PalN.ChatterjeeEffect of clonidine and magnesium sulphate on anaesthetic consumption, haemodynamics and postoperative recovery: a comparative studyIndian J Anaesth542010137141
- J.MalekJ.KnorA.KurzovaM.LopourovaAdverse hemodynamic changes during laparoscopic cholecystectomy and their possible suppression with clonidine premedication. Comparison with intravenous and intramuscular premedicationRozhl Chir781999286291
- C.S.SungS.H.LinK.H.ChanW.K.ChangL.H.ChowT.Y.LeeEffect of oral clonidine premedication on perioperative hemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic cholecystectomyActa Anaesthesiol Sin3820002329
- H.P.YuS.S.HseuH.W.YienY.H.TengK.H.ChanOral clonidine premedication preserves heart rate variability for patients undergoing laparoscopic cholecystectomyActa Anaesthesiol Scand472003185190
- DasMrinmoyRayManjushreeMukherjeeGauriHemodynamic changes during laparoscopic cholecystectomy: effect of oral clonidine premedicationIndian J Anaesth512007205210
- N.K.KalraA.VermaA.AgarwalH.D.PandeyComparative study of intravenously administered clonidine and magnesium sulfate on hemodynamic responses during laparoscopic cholecystectomyJ Anaesthesiol Clin Pharmacol272011344348
- A.M.KoivusaloM.ScheininI.TikkanenT.Yli-SuomuS.RistkariJ.LaaksoL.LindgrenEffects of esmolol on haemodynamic response to CO2 pneumoperitoneum for laparoscopic surgeryActa Anaesthesiol Scand4251998510517
- R.J.GorczynskiJ.E.ShafferR.J.LeePharmacology of ASL-8052, a novel beta-adrenergic receptor antagonist with an ultrashort duration of actionJ Cardiovasc Pharmacol56198377
- P.F.WhiteB.WangJ.TangThe effect of intraoperative use of esmolol and nicardipine on recovery after ambulatory surgeryAnesth Analg97200316331638
- I.TopcuT.OzturkT.TasyuzThe effects of esmolol on anesthetic and analgesic requirementTurk J Anaesth Reanim352007393398
- V.CollardG.MistralettiA.TaqiIntraoperative esmolol infusion in the absence of opioids spares postoperative fentanyl in patients undergoing ambulatory laparoscopic cholecystectomyAnesth Analg105200712551262
- I.SmithJ.V.HemelrijckP.F.WhiteEfficacy of esmolol versus alfentanil as a supplement to propofol-nitrous oxide anesthesiaAnesth Analg731991540546