Abstract
Background
Cognitive dysfunction is the impairment of the mental process and affected by blood pressure. The aim of this work was to assess the cognitive dysfunction after controlled hypotensive and normotensive anesthesia in middle aged patients undergoing septoplasty.
Methods
Sixty patients (ASA I–II), 21 to 50 years were included in the study, undergoing septoplasty operation. Patients were randomly assigned into two equal groups, namely group (A), who were generally anesthetized and associated with controlled hypotension and group (B), who were generally anesthetized and associated with local anesthesia. Heart rates, blood pressure and oxygen saturation were measured throughout the operation. Mini Mental State Examination (MMSE) was used for evaluation of cognitive functions preoperatively and postoperatively.
Results
Regarding cognitive function, there were no statistically significant differences between both groups in preoperative and after 24 h of postoperative period, but there were statistically significant decrease in group (A) in relation to group (B) after 30 minutes and 60 minutes and the incidence of postoperative cognitive dysfunction in group (A) was 23.3% after 30 min, 13.3% after 60 min and 6.6% after 24 h, but in the other group (B) there were no recorded cases of cognitive dysfunction at 30 min,60 min and 24 h.
Conclusion
Increasing isoflurane MAC and using controlled hypotension to get bloodless field can affect the cognitive function appear in MMSE score but light volatile anesthetic combined with regional anesthesia with local vasoconstrictors is better regime to get better postoperative cognitive function.
Introduction
Cognitive dysfunction is the impairment of the mental process of perception, memory and information processing which allows the individual to acquire knowledge and plan for the future [Citation1]. Cognitive dysfunction may complicate recovery after operation and affect middle aged patients who may have to give up work and social activities [Citation2].
General anesthetic agents, postoperative analgesic regiment, and hypotension associated with anesthesia can cause postoperative cognitive dysfunction [Citation3]. Induced hypotensive anesthesia is essential for drying surgical field during maxillofacial operation like septoplasty to reduce blood loss, ease in operation technique and shorten duration of surgery. Hypotensive anesthesia is associated with the risk of reduced perfusion to important organs and tissues, mainly the brain, heart and kidneys [Citation4].
Bleeding is one of the biggest complications of nasal surgery. Minimization of intraoperative blood loss allows the surgeon to have an operative field which he can visualize well. Blood loss can be minimized by applying epinephrine-containing local anesthetic to the nasal mucosa, maintaining a slight head-up position, and using controlled hypotension in appropriate individuals [Citation5].
The aim of this work was to assess the cognitive dysfunction after controlled hypotensive and normotensive anesthesia in middle aged patients undergoing septoplasty.
Patients and methods
After obtaining approval from the Ethical committee and written informed consent, 60 patients ASA I or II, aged 21–50 years were included undergoing septoplasty operation in Misr University for Science and Technology hospital from October 2014 till June 2015. Patients were randomly assigned into two equal groups, namely group (A), who were generally anesthetized and associated with controlled hypotension and group (B) who were generally anesthetized and associated with local anesthesia and vasoconstrictor. Distribution of the patients into the groups was done by using computer-generated randomization code. Patients with arrhythmias, congestive heart failure, coronary arterial disease, hypertension, cerebrovascular diseases, neuropsychiatric disorders and known allergic reaction were excluded from the study.
Patients of both groups were fasting for 8 hours before operations. They did not receive any premedications. Intraoperative monitors were continuous electrocardiography (ECG), pulse oximetry (Sp02), capnography and invasive arterial blood pressure through a 20 gauge catheter inserted into the redial artery. Ringer’s solution with a rate of 5–10 ml/kg was started through an 18 gauge cannula. Patient’s head raised 40 degree.
In group (A): Anesthesia was introduced by propofol 2.5 mg/kg, fentanyl 1 μg/kg and atracurium 0.5 mg/kg to facilitate oral intubation. Anesthesia was maintained by starting minimum alveolar of concentration (MAC) of isoflurane 2% in 50% oxygen and 50% air. The MAC increased to maintain mean blood pressure between 50 and 60 mmHg or reducing mean blood pressure by 30% of baseline. The patients were mechanically ventilated, adjusted to maintain end tidal CO2 pressure between 30 and 35 mmHg. At recovery, muscle relaxant was antagonized with neostigmine and atropine. The patients were transferred to the recovery room on eye opening and responding to verbal command.
In group (B): The anesthetic management was the same as group (A) except that the isoflurane concentration was adjusted to maintain normotensive blood pressure throughout the operation. General anesthesia was supplemented with local anesthesia as follows: initially a topical nasal decongestant (xylometazoline hydrochloride 0.1%) was applied. The nose was packed with local anesthetic soaked gauze and then supplemented with submucosal injection of local anesthetic with epinephrine (1% lidocaine with 1:200,000 epinephrine). The surgical conditions for a bloodless operative field were observed every 10 minutes by the same attending surgeon, who was blinded to the patient groups trying to keep the surgical field condition below 2 (Appendix 1).
Mini Mental State Examination (MMSE) was used for evaluation of cognitive functions [Citation6]. The MMSE was chosen because it is easily applicable, highly valid, and reliable, enabling frequent application. It consists of questions, evaluating orientation to time and places, registration, attention, calculation, short-term recall, language ability, and constructional ability. The MMS was performed 30 min before entry of the patient to the operating room (MMSP), 30 min (MMS30) and 60 min (MMS60) after extubation of the patient, at the recovery room, and at the postoperative 24th hour (MMS24), by the same anesthesiologist, trained in the use of the test and blinded to the patient group allocation. The maximum score being 30 points, a decrease of 2 or more was recorded as cognitive function decline and a score lower than 24 was recorded as cognitive impairment.
Aldrete post-anesthesia recovery score was obtained for each patient at the postoperative 30 and 60 minutes, so that cognitive function testing would only be applied to patients with the similar post-anesthesia recovery state [Citation7] (Appendix 2). An Aldrete Score ⩾7 was considered as the patient being awake and MMS was applied. The patients were transferred to the ward following the completion of MMS60 and meeting our discharge criteria (the patient being alert and oriented, stable vital signs, talkative and cooperative, with adequate pain control, minimal nausea, and vomiting). Postoperative analgesia was achieved by giving ketorolac 30 mg intravenously every 4 h to both groups.
.1 Statistical analysis
By using PASS program for sample size calculation, it was calculated that a sample size of 30 per group would achieve 80% power at p value less than 0.05. All statistical calculations were carried out using the computer program statistical package for social science (SPSS Inc. Chicago, Illinois, USA) version 11 for Microsoft windows. Data were expressed as mean plus standard deviation (SD) in demographic data except male and female numbers, MMSE, and Blood pressure unpaired T-test was used to compare data between groups. Results were considered statistically significant if P value was less than 0.05.
Results
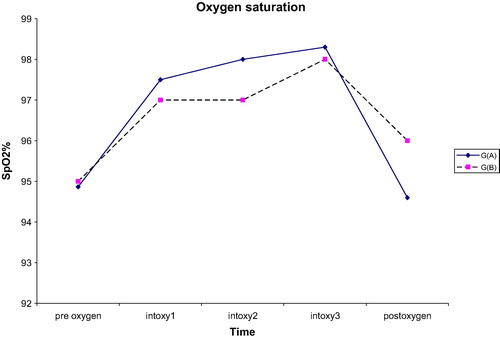
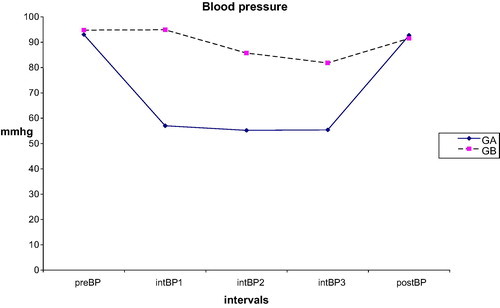
A total 60 patients ASA I-II enrolled in this study, undergone septoplasty operation. According to demographic data, both groups were similar and there were no statistical significant differences between ages, weight, heights, BMI, anesthesia minutes and surgical times as shown in . There were no statistical differences regarding heart rate (HR) and oxygen saturation during preoperative, intraoperative and postoperative periods . Measuring blood pressure in preoperative and postoperative periods was not significantly different between groups (A) and (B), but significantly decreased in group (A) (57, 55 and 55 mmHg) than in group (B) (94.9, 85.7 and 81.8 mmHg) during intraoperative period as shown in .

able 1 Demographic data numeric numbers represented by mean ± SD.
The Aldrete score of all patients in both groups, at the postoperative 30 and 60 minutes, was greater than 7. All the patients were awake during MMSE evaluation.
Regarding cognitive function evaluation, by using (MMSE), there were no statistically significant differences between both groups in preoperative period and after 24 h of postoperative period (MMSE 24), in group (A) (27.3 and 26.7) and group B (28.1 and 27.2), but there were statistically significant differences between both groups after 30 minutes (MMSE 30) and 60 minutes (MMSE 60) in group (A) (24 and 24.9) and in group (B) (26 and 26.5) as shown in . The incidence of postoperative cognitive dysfunction in group (A) was 7 cases 23.3% after 30 min, 4 cases 13.3% after 60 min and 2 cases 6.6% after 24 h, but in the other group (B) there were no recorded cases of cognitive dysfunction at 30 min, 60 min and 24 h as shown in .
able 2 Mini Mental State Examination (MMSE) scores and percentage of patients suffered postoperative cognitive dysfunction (PCD).
Discussion
This study evaluated the effect of hypotensive anesthesia on postoperative cognitive function (POCD). This was performed by randomizing patients undergoing septoplasty operation and equally divided into two groups: (A) and (B). Many techniques have been used to deal with bleeding during septoplasty but none of them is ideal. In the present study, in group (A) bloodless field was achieved by isoflurane induced controlled hypotensive anesthesia with mean blood pressure which was around 50 mmHg and local anesthesia plus vasoconstrictor with normal blood pressure in group (B).
In group (A) there was cognitive decline at 30 and 60 min as measured by MMSE postoperatively, and these results were comparable to results of Celebi and his colleagues, who measured the effect of hypotensive anesthesia on cognitive function by using MMSE as a tool to assess cognitive function. Esmolol and remifentanil were given separately in groups to induce controlled hypotension, and there was postoperative cognitive dysfunction in both groups [Citation8].
Chen et al. have stated that at the postoperative 60 min, 51% of patients in desflurane group and 57% of patients in sevoflurane group showed significant decreases in cognitive function. In 3 h, 85% of patients returned to their basal cognitive function levels and at the postoperative 24 h, all patients but one had normal basal MMSE scores. Our finding in group (A) was the incidence of postoperative cognitive dysfunction 23.3% after 30 min, 13.3% after 60 min and 6.6% after 24 h. Our finding is far more different from finding in this study because our study population was younger compared to previous study as elderly patients are susceptible to cognitive dysfunction [Citation9].
Gruvstad and his colleagues [Citation10] found greater impairment in psychiatric and psychometric tests after hypotensive anesthesia which were comparable to the results of the present research. In the present study, there were differences between both groups (A) and (B) related to postoperative cognitive function but these results were not similar to results obtained by Eckenhoff and his colleagues [Citation11] where the postoperative cognitive function was similar in both groups (hypotensive and normotensive groups). The contradiction may be due to difference in tool of assessing the cognitive function.
Rohan and his colleagues [Citation12] observed increased incidence of postoperative cognitive dysfunction within 24 h after minor surgery generally anesthetized in elderly, and about 47% of patients suffered postoperative cognitive dysfunction in both groups (propofol and sevoflurane groups). The incidence of postoperative cognitive dysfunction was more than the incidence in group (A) so it was 23.3% after 30 min, 13.3 after 60 min and 6.6% after 24 h in this research. The difference was due to the fact that the participants were younger in the present research than in Rohan’s research.
After surgery, patients may suffer a decline in cognitive function due to multifactorial causes as anesthetic agents, postoperative analgesia requirement, inflammatory or metabolic endocrine stress response associated with surgery, hypotension, increased age, duration of anesthesia, less education and postoperative infection. Cognitive function impairment observed in MMSE score applied on hypotensive group (A) can be attributed mainly to the residual effect of general anesthesia, surgical stress and hypotension [Citation8].
Increasing the dose of general anesthesia isoflurane to produce controlled hypotensive anesthesia, affects the brain function including neuronal membranes, receptors, ion channels, neurotransmitters, cerebral blood flow and metabolism. Hole et al. [Citation13] and Chung et al. [Citation14] observed during the early postoperative days significant cognitive impairment in elderly patients after general anesthesia and not after subarachnoid or epidural analgesia. Tzabar reported a highly significant greater incidence of cognitive failures after general anesthesia compared with local analgesia for 3 days after day case surgery [Citation15].
Stress response hormones of the adrenocortical axis have recognized effects on memory and behavior, modulating synaptic transmission and neuronal circuit plasticity. Mediators of the acute phase response, including cytokines and heat shock proteins, have well-described effects on behavior and learning. Reactive oxygen species and oxidative stress, as seen in severe sepsis, are also associated with decreased cognitive function. Furthermore, the induced surgical stress response that could also contribute to the occurrence of POCD is substantially altered by regional block but not by general anesthesia [Citation16].
Changes in cerebral perfusion and metabolism during surgery may be significantly affected by anesthetic management. These include alterations in systemic blood pressure, cardiac output, cerebral metabolic rate, the degree of hypocarbia, and concurrent use of pharmacologic agents with vasoconstrictor activity. In addition, general anesthesia has direct pharmacologic effects on the brain. The physiological effects of general and regional anesthesia on cerebral blood flow, oxygen delivery, and cerebral metabolism are markedly different. Many patients and some clinicians presume that cognitive dysfunction and other complications should be less frequent with regional anesthesia than with general anesthesia [Citation17].
It is assumed that drugs used for general anesthesia blocking central cholinergic transmission result in a relative lack of acetylcholine in the brain, which is essential for learning and memory. Drugs affecting the cholinergic system are atropine, scopolamine, opioids, benzodiazepines, ketamine, H2-blocker, volatile anesthetics, and propofol [Citation18].
There is strong evidence suggesting that low blood pressure is accompanied by diminished cognitive performance, primarily involving attention and memory. The relationship between blood pressure and cortical activity is also reflected in a negative correlation between blood pressure and a wave activity in the spontaneous electroencephalogram (EEG). This suggests that low blood pressure is associated with a reduced tonic cortical arousal [Citation19].
Healthy individual processes of autoregulation keep the cerebral blood flow constant within a wide range of arterial blood pressure. In order to ensure stable perfusion, cerebral resistance vessels constrict during increases and dilate during reductions in systemic blood pressure. Autoregulation is considered to be a protective mechanism which prevents brain ischemia during blood pressure decrease, and guards against capillary damage and edema formation. Under normal conditions the limits within which cerebral blood flow is assumed to be constant are approximately between a mean arterial pressure (MAP) of 60 and 150 mmHg [Citation20].
If arterial blood pressure is outside of this range, cerebral blood flow rises or falls with respective increases or decreases in blood pressure. Slight reductions of blood pressure below the lower limit of autoregulation can be compensated by an increase of the extraction coefficient of oxygen from the blood. Further reductions ultimately lead to irreversible brain damage [Citation21].
Conclusion
Increasing isoflurane MAC and using controlled hypotension to get bloodless field can affect the cognitive function appear in MMSE score but light volatile anesthetic combined with regional anesthesia with local vasoconstrictors is better regime to get better postoperative cognitive function in patients undergoing septoplasty.
Conflict of interest
The author has no conflict of interest to declare.
Notes
Peer review under responsibility of Egyptian Society of Anesthesiologists.
References
- C.D.HanningPostoperative cognitive dysfunctionBr. J. Anaesth.9520058287
- T.JohnsonT.MonkL.S.RasmussenH.AbildstromP.HouxK.KorttilaH.M.KuipersC.D.HanningV.D.SiersmaPostoperative cognitive dysfunction in middle-aged patientsAnesthesiology96200213511357
- J.T.MollerP.CluitmansL.S.RasmussenP.HouxH.RasmussenJ.CanetLong-term postoperative cognitive dysfunction in the elderly ISPOCD1 study ISPOCD investigators international study of post-operative cognitive dysfunctionLancet3511998857861 Erratum in: Lancet 1998; 351: 1742
- M.BarakL.YoavI.Abu el-NaajHypotensive anesthesia versus normotensive anesthesia during major maxillofacial surgery: a review of the literature2015Hindawi Publishing Corporation the Scientific World Journal VolumeBerlin7 pages Article ID 480728
- U.GalwayD.AlamAnesthesia for septoplasty and rhinoplastyAnesthesia for otolaryngologic surgery2013Published by Cambridge University Press113120
- M.F.Folstein“Mini-mental state”. A practical method for grading the cognitive state of patients for the clinicianJ Psychiatr Res121975189198
- J.AldreteD.KroulikA postanesthetic recovery scoreAnesth Analg491970924934
- N.CelebiF.ArtukogluD.DalF.SaricaogluV.CelikerU.AyparEffect of hypotensive anesthesia on cognitive functions; a comparison of esmolol and remifentanil during tympanoplastySaudi Med J28200713571361
- X.ChenM.ZhaoP.F.WhiteS.LiJ.TangR.H.WenderThe recovery of cognitive function after general anesthesia in elderly patients: a comparison of desflurane and sevofluraneAnesth Analg93200114891494
- M.GruvstadLarsKebbonB.A.LofChanges in mental functions after induced hypotension: immediate and late effects of operations under hypotensive anesthesia on cerebral functionsPublisher Munksgaard, Acta Psychiatr Scand3719621112
- J.E.EckenhoffJ.R.ComptonA.LarsonM.B.DurhR.M.DaviesAssessment of cerebral effects of deliberate hypotension by psychological measurementsLancent1964711714
- D.RohanD.J.BuggyS.CrowleyF.K.H.LingH.GallagherC.ReganD.C.MoriartyIncreased incidence of postoperative cognitive dysfunction 24 h after minor surgery in the elderly.Can J Anesth5222005137142
- A.HoleH.TerjesenH.BreivikEpidural versus general anaesthesia for total hip arthroplasty in elderly patientsActa Anaesth Scand241980279287
- F.ChungR.MeierE.LautenschlaegerF.j.CarmichaelA.ChungGeneral or spinal anaesthesia: which is better in the elderly?Anesthesiology671987422427
- Y.TzabarA.j.AsburyK.MillarCognitive failures after general anaesthesia for day-case surgeryBr J Anaesth761996194197
- F.JinF.ChungMinimizing perioperative adverse events in the elderlyBr J Anaesth8742001608624
- T.P.SzatrowskiM.E.CharlsonCognitive effects after epidural vs. general anesthesia in older adultsJAMA27419954450
- B.JungwirthW.ZieglgänsbergerE.KochsG.RammesAnesthesia and postoperative cognitive dysfunction (POCD)Cent Nerv Syst Agents Med Chem820083747
- S.DuschekR.SchandryReduced brain perfusion and cognitive performance due to constitutional hypotensionClin Auton Res1720076976
- S.DuschekR.SchandryCognitive performance and cerebral blood flow in essential hypotensionPsychophysiology412004905913
- J.M.ChillonG.L.BaumbachAutoregulation of cerebral blood flowK.M.A.WelchL.R.CaplanD.J.ReisB.K.SiesjoB.WeirPrimer on cerebrovascular diseases1995Academic PressSan Diego5154
ppendix 1
Category scale for intraoperative surgical field evaluation
Appendix 2
ppendix 3
The Mini-Mental State Examination

